Abstract
Objective: To explore the effects of laparoscopic myomectomy and open surgery on the postoperative inflammatory responses, endocrine statuses, and prognoses of uterine myoma patients. Methods: Uterine myoma patients (n=126) admitted to the Department of Gynecology in our hospital were recruited as the study cohort and divided into an observation group (n=63), and a control group (n=63). The patients in the observation group underwent laparoscopic myomectomies, and the patients in the control group underwent open surgery. The completion times, intraoperative blood loss volumes, postoperative hospital stay durations, postoperative exhaust times, preoperative and postoperative immune function, inflammatory factors, sex hormone levels, postoperative complications, and prognoses were observed. Results: The observation group showed shorter hospital stays, lower intraoperative blood loss volumes, and shorter postoperative exhaust times (P<0.001). After the surgery, CD3+%, CD4+%, and CD4+%/CD8+% were decreased, but the CD8+% was increased in the two groups (all P<0.01). The observation group had higher CD3+%, CD4+% and CD4+%/CD8+%, and lower CD8+% than the control group (all P<0.001). The C-reactive protein, TNF-α, and IL-6 levels were higher after the surgery in the two groups (all P<0.05), but the observation group had lower levels (all P<0.001). The follicle-stimulating hormone and luteinizing hormone levels were lower, but the estradiol levels were higher in the observation group compared to the levels in the control group (all P<0.001). The total number of complications in the observation group was significantly lower than it was in the control group (P<0.05). Conclusion: Laparoscopic myomectomy contributes to quick recoveries and short hospital stays, reduces the postoperative inflammatory response and immunosuppression, has little effect on the postoperative sex hormone levels, and has a low incidence of complications. It is worthy of clinical application.
Keywords: Uterine myoma, laparoscopic myomectomy, open surgery, inflammatory response, endocrine status, prognosis
Introduction
Uterine myomas are noncancerous growths of the uterus in female patients that often appear during the childbearing years (at the age of 30-50), with an incidence rate of 20-25% [1]. Although most uterine myomas are benign, 0.4-0.8% of them will become cancerous. Thus, for patients with poor drug treatment, uterine myomas should be surgically removed as soon as possible [2,3].
Surgery is the most effective way to treat uterine fibroids, and open surgery is most commonly used type of surgery [4,5]. But it causes great trauma and is not conducive to postoperative recovery [6,7]. However, due to its small trauma and quick recovery, laparoscopic myomectomy is increasingly being used [8,9].
However, previous surgical studies have shown that laparoscopic surgery causes more bleeding than open surgery [10]. It is also a challenge for doctors to perform laparoscopic surgery, and they must deal with hemostasis, which demands a long-term learning and practice process for them [11,12]. Based on this, this study compared the clinical effectiveness, the postoperative inflammatory response, and the endocrine statuses of patients with uterine fibroids who underwent laparoscopic surgery and open surgery, in order to provide more information for the clinical treatment.
Materials and methods
Data collection
Uterine myoma patients (n=126) admitted to the Department of Gynecology in our hospital from July 2018 to December 2019 were recruited as the cohort for this prospective study. They were 25-50 years old, with an average age of 33.2±3.1 years old. According to the different procedures each patient underwent, the patients were divided into the observation group (n=63), with an average age of 33.4±3.4 years old, and the control group (n=63), with average age of 33.0±3.1 years old. The patients in the observation group underwent laparoscopic myomectomies, while those in the control group underwent open surgeries. The protocol was approved by the ethics committee of our hospital, and written informed consents were signed by all the patients.
Inclusion criteria
(1) Patients who met the diagnostic criteria for uterine fibroids [13]. (2) Patients who had indications for surgery. (3) Patients who were between the ages of 18 and 75. (4) Patients with fewer than four fibroids ≤3 cm in size. (5) Patients able to cooperate with the treatment and the researchers.
Exclusion criteria
(1) Patients unable to tolerate the surgery. (2) Patients who had severe heart, liver, kidney, or other diseases. (3) Patients with gynecological malignant tumors. (4) Patients with severe coagulopathy. (5) Pregnant or lactating women.
Surgical techniques
The control group underwent open surgery and general anesthesia. Each patient was given a mask to inhale oxygen with a flow rate set at 6-8 L/min. Midazolam (0.05-0.10 mg/kg, Jiangsu Enhua Pharmaceutical Co., Ltd., China, H19990027), propofol (1.0-1.5 mg/kg, Xi’an Libang Pharmaceutical Co., Ltd., China, H20010368), sufentanil citrate (0.2-0.3 μg/kg, Yichang Renfu Pharmaceutical Co., Ltd., China, H20054171) and cisatracurium (0.15-0.20 mg/kg, Shanghai Hengrui Pharmaceutical Co., Ltd., China, H20060869) were given through intravenous infusion according to the patient’s body weight. General anesthesia was used to induce tracheal intubation after 3 minutes of assisted breathing. Sufentanil citrate (10-20 µg) was injected intravenously 5 minutes before the skin incision. After the anesthesia, the patient was put in the bladder lithotomy position. A transverse incision was made in the middle of the abdomen, the subcutaneous tissues were separated, and the pelvic cavity was exposed, and the adhesion of the fibroids to the surrounding tissues was observed. For those with adhesions of the surrounding tissues, the uterus was lifted out of the abdomen after the separation, and the most swollen parts of the fibroids were cut out and bluntly separated. The separated uterine fibroids were removed and an electric knife was used to stop the bleeding. Finally, the wound was sutured layer by layer.
The observation group underwent laparoscopic myomectomies. The anesthetic method and positions were the same as in the control group. After a 1 cm incision was made at the umbilicus, the pneumoperitoneum pressure was established at this incision and maintained at 12-15 mmHg. One 5 mm and one 10 mm trocar were inserted at the left and right McDonald’s points respectively. A 2 cm incision was made at 2 cm above the symphysis pubis, where a 5 mm trocar was placed.
The location of the fibroids was found, and a monopolar electrocoagulation hook (China, Jiangsu Yibo Leiming Medical Technology Co., Ltd., 20152251081) was used to cut the outer surfaces. Grasping forceps were used to clamp and fix for blunt separations. The wound was sutured to close the tumor cavity after the suturing.
To ensure the quality of the surgery, the following plans were carried out. All the operations were performed by experienced surgeons. The same patch and suture material were used for the same operations. The patients in the both groups were treated with uniform treatment and nursing plans before and after surgery. Intraoperative bleeding was stopped, and the postoperative incisions were routinely treated to prevent infections. The two groups shared the same follow-up plans.
Outcome measures
Main outcome measures: The operation completion time was recorded from the incision to the end of suturing. The amount of bleeding was recorded from the beginning of the operation to the end of the suturing. The hospital stays referred to the number of days from the initial hospitalization to the discharge. The time from the completion of the operation to the first exhaust was defined as the exhaust time.
The Tr cell and inflammatory factor levels in the peripheral blood were measured before the surgery and at 14 days after the surgery. Within 24 hours before each surgery and 14 days after each surgery, 5 mL of venous blood was collected from each patient at 8 o’clock in the morning, and a FACSCanto II flow cytometer (USA, BD Company) was used to measure the FITC-labeled anti-human CD3, CD4 levels, and the CD8 monoclonal antibody expressions were compared with the CD3+%, CD4+%, CD8+% and CD4+%/CD8+% T cell subsets. The serum and plasma were separated using a centrifuge (Shanghai Jumu Medical Instruments Co., Ltd., China) at a speed of 3,300 rpm/min and centrifuged for 15 minutes. The separated plasma was added to 40 μL of a protease inhibitor phosphate buffer solution (Xiamen Hai Standard Technology Co., Ltd., China), and stored in a freezer at -80°C. An automatic multifunctional microplate reader (American Thermo Company) and ELISA (Shanghai Bairui Biotechnology Co., Ltd., China) were used to measure the IL-6, C-reactive protein and TNF-α levels.
The FSH, LH, and E2 levels were measured before the surgery at and 1 month after surgery.
Secondary outcome measures: The postoperative complications included intestinal obstructions, celiac adhesions, urinary retention, bleeding, urinary tract infections, and incision infections. The occurrences of each complication were recorded. Incidence of complications = number of complications/total cases * 100%.
The normal uterine morphology, normal menstrual cycle, and recurrences were observed at 1 year after the surgery. The occurrence rate = number of occurrences/total cases * 100%.
Statistical analysis
SPSS 17.0 was used for the statistical analysis. The measurement data were expressed as the mean ± standard deviation (x̅±sd). t-tests were used for the data following a normal distribution and a homogeneity of variance, and represented by t. Rank sum tests were used for the data following a non-normal distribution and with a uniformity of variance, represented by Z. The count data were represented as number/percentage (n/%). Pearson’s chi-square tests and Fisher’s exact probability method were applied, expressed in chi-square. P<0.05 meant that the results were significantly different.
Results
General data
There were no significant differences in the two groups’ general data (P>0.05). See Table 1.
Table 1.
The general data (n, x̅±sd)
| Items | Observation group (n=63) | Control group (n=63) | χ2/t | P |
|---|---|---|---|---|
| Age (years) | 33.4±3.4 | 33.0±3.1 | 0.690 | 0.491 |
| Average size of fibroids (cm) | 3.96±0.46 | 4.05±0.52 | 1.029 | 0.306 |
| Number of fibroids (n) | 3.21±0.84 | 3.25±0.86 | 0.264 | 0.792 |
| Location of fibroids (n) | 0.129 | 0.720 | ||
| Subserosal fibroids | 34 | 36 | ||
| Intermural fibroids | 29 | 27 | ||
| Occurrence of fibroids (n) | 0.131 | 0.717 | ||
| Single fibroids | 25 | 27 | ||
| Multiple fibroids | 38 | 36 | ||
| Body mass index (kg/m2) | 23.28±2.22 | 23.63±2.44 | 0.842 | 0.401 |
Postoperative indicators
The observation group had shorter hospital stays, lower intraoperative blood loss volumes, and shorter postoperative exhaust times (all P<0.001). No difference was found in the completion times (P>0.05). See Table 2.
Table 2.
The postoperative indicators (x̅±sd)
| Items | Observation group (n=63) | Control group (n=63) | t | P |
|---|---|---|---|---|
| Hospital stays (d) | 6.9±1.2 | 10.3±1.5 | 14.051 | <0.001 |
| Completion time (min) | 56.36±18.63 | 58.74±19.27 | 0.705 | 0.482 |
| Intraoperative blood loss volume (mL) | 63.75±9.74 | 140.14±18.74 | 28.710 | <0.001 |
| Postoperative exhaust time (h) | 16.47±2.23 | 25.74±4.58 | 14.441 | <0.001 |
Peripheral blood Tr cell subsets
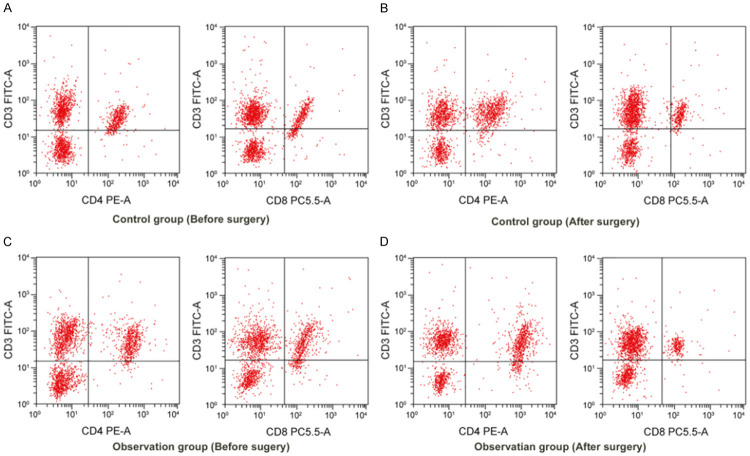
There were no significant differences in the CD3+%, CD4+%, CD8+% or CD4+%/CD8+% between the two groups before the surgery (all P>0.05). After the surgery, the CD3+%, CD4+%, and CD4+%/CD8+% were decreased, and the CD8+% was increased in the two groups (all P<0.01). The observation group had higher CD3+%, CD4+% and CD4+%/CD8+%, and lower CD8+% than the control group (all P<0.001). See Table 3 and Figure 1.
Table 3.
Peripheral blood Tr cell subsets (x̅±sd)
| Items | Observation group (n=63) | Control group (n=63) | ||
|---|---|---|---|---|
|
|
|
|||
| Before surgery | After surgery | Before surgery | After surgery | |
| CD3+% | 49.63±9.74 | 45.36±8.74**,### | 48.42±9.21 | 39.75±8.78*** |
| CD4+% | 43.56±6.25 | 39.54±7.93***,### | 44.69±6.74 | 34.67±7.39*** |
| CD8+% | 26.76±3.14 | 29.78±4.12**,### | 27.69±3.34 | 34.63±5.32*** |
| CD4+%/CD8+% | 1.62±0.31 | 1.37±0.32***,### | 1.63±0.32 | 1.05±0.27*** |
Note: Compared with before the surgery in the same group;
P<0.01;
P<0.001.
Compared with the control group after the surgery;
P<0.001.
Figure 1.
CD3, CD4, and CD8 flow graphs in the two groups before and after the surgery. A: Control group (before surgery); B: Control group (after surgery); C: Observation group (before surgery); D: Observation group (after surgery).
Inflammatory factors
After the surgeries, the C-reactive protein, TNF-α, and IL-6 levels were higher in the two groups (all P<0.001), but the observation group had lower levels (all P<0.001). See Table 4.
Table 4.
The inflammatory factors (x̅±sd)
| Items | Before surgery | After surgery | ||
|---|---|---|---|---|
|
|
|
|||
| Observation group (n=63) | Control group (n=63) | Observation group (n=63) | Control group (n=63) | |
| CRP (mg/L) | 6.98±1.74 | 6.81±1.71 | 24.39±9.41***,### | 38.54±13.54*** |
| TNF-α (µg/mL) | 123.74±18.58 | 124.25±18.76 | 154.63±22.74***,### | 188.69±24.69*** |
| IL-6 (µg/mL) | 352.98±36.73 | 351.98±36.12 | 410.25±48.93***,### | 432.58±50.39*** |
Note: Compared with before the surgery in the same group;
P<0.001.
Compared with the control group after the surgery;
P<0.001.
Sex hormone levels
After the surgery, the follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels were higher, but the estradiol (E2) level was lower in the observation group (all P<0.001). The FSH and LH levels in the observation group were lower than they were in the control group, but the E2 level was higher than it was in the control group (all P<0.001). See Table 5.
Table 5.
The sex hormone levels (x̅±sd)
| Items | Before surgery | After surgery | ||
|---|---|---|---|---|
|
|
|
|||
| Observation group (n=63) | Control group (n=63) | Observation group (n=63) | Control group (n=63) | |
| Follicle-stimulating hormone (m IU/mL) | 17.63±2.94 | 17.84±2.99 | 21.39±2.69***,### | 24.98±3.69*** |
| Luteinizing hormone (pg/mL) | 18.69±3.97 | 19.06±3.85 | 23.69±4.22***,### | 29.63±5.74*** |
| Estradiol (m IU/mL) | 282.98±19.68 | 281.98±20.36 | 246.35±20.76***,### | 198.65±18.74*** |
Note: Compared with before the surgery in the same group;
P<0.001.
Compared with the control group after the surgery;
P<0.001.
Postoperative complications
The total number of complications in the observation group was significantly lower than the total number of complications in the control group (P<0.05). See Table 6.
Table 6.
The postoperative complications (n, %)
| Items | Observation group (n=63) | Control group (n=63) | χ2 | P |
|---|---|---|---|---|
| Intra-abdominal adhesions | 1 (1.59) | 3 (4.76) | 1.033 | 0.310 |
| Intestinal obstructions | 0 (0.00) | 1 (1.59) | 1.008 | 0.315 |
| Urinary retention | 2 (3.17) | 3 (4.76) | 0.208 | 0.648 |
| Bleeding | 1 (1.59) | 3 (4.76) | 1.033 | 0.310 |
| Urinary tract infections | 1 (1.59) | 2 (3.17) | 0.341 | 0.559 |
| Incision infections | 1 (1.59) | 3 (4.76) | 1.033 | 0.310 |
| Total number of cases | 6 (14.29) | 15 (23.81) | 4.629 | 0.031 |
Prognosis
No significant differences were found between the two groups in their normal uterine morphology, normal menstrual cycle, or recurrence rates (all P>0.05). See Table 7.
Table 7.
The prognoses (n, %)
| Items | Observation group (n=63) | Control group (n=63) | χ2 | P |
|---|---|---|---|---|
| Normal uterine morphology (n%) | 58 (92.06) | 57 (90.48) | 0.100 | 0.752 |
| Normal menstrual cycle (n%) | 60 (95.24) | 58 (92.06) | 0.465 | 0.534 |
| Recurrence (n%) | 2 (3.17) | 4 (6.35) | 0.700 | 0.403 |
Discussion
Uterine myomectomy is the most widely used surgical method, as it has little effect on the uterus and preserves the uterus’ fertility function [14,15]. It is necessary to perform uterine myomectomy under open conditions. Although open surgery has a significant surgical effect, it is confronted with large surgical trauma, heavy bleeding, and a slow recovery [16]. With the development of minimally invasive surgery technology, laparoscopic myomectomy has become a new direction.
Laparoscopic myomectomy has the advantages of fast postoperative recovery, short hospital stays, and fewer complications [17]. Compared with open surgery, laparoscopic myomectomy has some difficulty in the peeling and suturing of uterine fibroids [12,18]. It is suggested that serious hemorrhaging is more likely to occur under laparoscopic surgery and that open surgery needs to be used as a remedial measure [19]. Laparoscopic myomectomy often takes a long time due to the difficulty of operation and the time needed for establishing the pneumoperitoneum. However, with technological advances and equipment improvements, the time needed for laparoscopic myomectomy has been greatly shortened, so it is roughly the same as the time needed for open surgery [20]. In this study, the hospital stays and postoperative exhaust times in the observation group were lower than they were in the control group, indicating that laparoscopic myomectomy had faster postoperative recoveries and shorter hospital stays, which is consistent with the results of the above study. The amount of bleeding in the observation group was less than it was in the control group, and this may be related to the routine use of ultrasonic scalpels and electrocoagulation knives in laparoscopic surgery to effectively stop the bleeding during the operation [21]. In terms of the operating times, it didn’t increase in the laparoscopic surgery [22].
Both methods in this study caused damage and immune inflammation in the body, resulting in postoperative inflammation and immunosuppression, but the laparoscopic myomectomy had better outcomes. Previous studies have shown that the inflammatory factors and immune statuses would change in the case of body damage, mainly manifested by decreased immunity and increased secretions of the inflammatory factors [23]. It has been demonstrated that postoperative inflammation and the severity of oxidative stress are related to patient prognosis [24]. In this study, both laparoscopic surgery and open surgery caused damage to the body, resulting in a postoperative inflammatory response and decreased immune function, but the open surgery had worse outcomes, leading to longer postoperative hospital stays and recovery times for the patients. This may be related to the declined postoperative inflammation and immune function, which is consistent with the above-mentioned research results. Laparoscopic myomectomy is safe and effective, and causes less damage to the human body. It can promote postoperative recovery, and it can effectively reduce the incidence of inflammation, immunosuppression, and complications [25]. Laparoscopic myomectomy has little effect on the immune or the inflammatory response, which may be because it causes less damage to the surrounding tissues [26].
In this study, the changes in the sex hormone levels before and at 1 month after the surgery were monitored. After the surgery, the FSH and LH in the the observation group were lower than they were in the control group, but the E2 level was higher than it was in the control group. It has been reported that uterine fibroids mostly occur in women of childbearing age, and uterine fibroid atrophy occurs after menopause; thus, some scholars believe that the occurrence and development of uterine fibroids are closely related to female hormone levels [27]. A Chinese clinical study found that open surgery reduces the blood supply of the anastomotic branches of the uterine and ovarian arteries, which decreases the negative feedback regulation of the ovaries at the hormonal levels, causing hormone secretion disorders [25]. However, laparoscopic myomectomy has less impact on the level of sex hormones due to its limited surgical site and its lower amount of damage caused to the surrounding tissues [28].
The laparoscopic surgery complication rate was lower than the open surgery complication rate. The most common complications after the open surgeries were abdominal adhesions and incision infections, which are related to the large incision and the slow healing of open surgery. Due to the improvement in the equipment and the small wounds, the laparoscopic myomectomies had a lower incidence of incision infections. In this study, the incidence of complications in the observation group was lower than it was in the control group, with a significant difference. In the 1-year follow-up after surgery, the two groups had the same outcomes, suggesting that laparoscopic and open surgeries had similar rates of clinical effectiveness for uterine fibroids, which is consistent with previous research [29].
However, there are still some shortcomings to this study. It was a single-center study with a small study cohort. A multi-center study with a large study cohort is expected for clinical research.
In summary, laparoscopic myomectomy has the advantages of quick recovery and short hospital stays, a reduced postoperative inflammatory response and immunosuppression, a small effect on the postoperative sex hormone levels as well as a low incidence of complications. It is worthy of clinical application.
Disclosure of conflict of interest
None.
References
- 1.Zhang YX, Gu XL, Meng YJ, Guo HZ, Du JH, Xing W. Analysis of the effect of laparoscopy and hysteroscopy on ovarian function, immune function and quality of sexual life of patients with hysteromyoma at different ages. Oncol Lett. 2018;15:2929–2934. doi: 10.3892/ol.2017.7631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rafnar T, Gunnarsson B, Stefansson OA, Sulem P, Ingason A, Frigge ML, Stefansdottir L, Sigurdsson JK, Tragante V, Steinthorsdottir V, Styrkarsdottir U, Stacey SN, Gudmundsson J, Arnadottir GA, Oddsson A, Zink F, Halldorsson G, Sveinbjornsson G, Kristjansson RP, Davidsson OB, Salvarsdottir A, Thoroddsen A, Helgadottir EA, Kristjansdottir K, Ingthorsson O, Gudmundsson V, Geirsson RT, Arnadottir R, Gudbjartsson DF, Masson G, Asselbergs FW, Jonasson JG, Olafsson K, Thorsteinsdottir U, Halldorsson BV, Thorleifsson G, Stefansson K. Variants associating with uterine leiomyoma highlight genetic background shared by various cancers and hormone-related traits. Nat Commun. 2018;9:3636. doi: 10.1038/s41467-018-05428-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ning GC, Zhang XR, Zhang Q, Wang ZB, Liao HE. Real-time and multimodality image-guided intelligent HIFU therapy for uterine fibroid. Theranostics. 2020;10:4676–4693. doi: 10.7150/thno.42830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jorgensen EM, Modest AM, Hur HC, Hacker MR, Awtrey CS. Hysterectomy practice patterns in the postmorcellation era. Obstet Gynecol. 2019;133:643–649. doi: 10.1097/AOG.0000000000003181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kazachkov EL, Voropaeva EE, Kazachkova EA, Zatvornitskaya AV, Dub AA, Miroshnichenko LE. Endometrial morphological characteristics in patients with hysteromyoma and chronic endometritis in infertility. Arkh Patol. 2019;81:41–48. doi: 10.17116/patol20198106141. [DOI] [PubMed] [Google Scholar]
- 6.Mangano A, Valle V, Bustos R, Gruessner S, Masrur M, Aguiluz G, Bianco F, Giulianotti PC. Robotic resection of a large ovarian leiomyoma. Minerva Chir. 2020;75:121–124. doi: 10.23736/S0026-4733.20.08253-X. [DOI] [PubMed] [Google Scholar]
- 7.Martin A, Tranoulis A, Sayasneh A. Uterine inversion secondary to a large prolapsed leiomyoma: diagnostic and management challenges. Cureus. 2020;12:e7168. doi: 10.7759/cureus.7168. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.Hashim HA, Al Khiary M, El Rakhawy M. Laparotomic myomectomy for a huge cervical myoma in a young nulligravida woman: a case report and review of the literature. Int J Reprod Biomed (Yazd) 2020;18:135–144. doi: 10.18502/ijrm.v18i2.6421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang M, Kim J, Kim TJ, Lee JW, Kim BJ, Bae DS, Choi CH. Long-term outcomes of single-port laparoscopic myomectomy using a modified suture technique. Obstet Gynecol Sci. 2020;63:164–172. doi: 10.5468/ogs.2020.63.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan JK, Gardner AB, Taylor K, Thompson CA, Blansit K, Yu XH, Kapp DS. Robotic versus laparoscopic versus open surgery in morbidly obese endometrial cancer patients - a comparative analysis of total charges and complication rates. Gynecol Oncol. 2015;139:300–305. doi: 10.1016/j.ygyno.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Shi X, Shi L, Zhang S. A comparative study on the short-term clinical efficacy of the modified laparoscopic uterine comminution technique and traditional methods. Mol Clin Oncol. 2020;12:237–243. doi: 10.3892/mco.2020.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trivedi PH, Trivedi S, Patil S. Laparoscopic in-bag morcellation compared with conventional morcellation of myomas and uterus with myomas. J Obstet Gynaecol India. 2020;70:69–77. doi: 10.1007/s13224-019-01273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ye F, Xu YP. Obstetrics and gynecology. In: Ye F, Xu YP, editors. Chongqing: Chongqing University Press; 2016. pp. 281–285. [Google Scholar]
- 14.Friedman JA, Wong JMK, Chaudhari A, Tsai S, Milad MP. Hysteroscopic myomectomy: a comparison of techniques and review of current evidence in the management of abnormal uterine bleeding. Curr Opin Obstet Gynecol. 2018;30:243–251. doi: 10.1097/GCO.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 15.Sleiman Z, Baba RE, Garzon S, Khazaka A. The significant risk factors of intra-operative hemorrhage during laparoscopic myomectomy: a systematic review. Gynecol Minim Invasive Ther. 2019;9:6–12. doi: 10.4103/GMIT.GMIT_21_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chao AS, Chang YL, Yang LY, Chao A, Chang WY, Su SY, Wang CJ. Laparoscopic uterine surgery as a risk factor for uterine rupture during pregnancy. PLoS One. 2018;13:e0197307. doi: 10.1371/journal.pone.0197307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alharbi AA, Alshadadi F, Alobisi A, Alsobai A, Felimban O, Hudairi H, Ammar S, Alzahrani S, Abuzaid A Sr, Oraif A Sr. Intraoperative and postoperative complications following open, laparoscopic, and hysteroscopic myomectomies in Saudi Arabia. Cureus. 2020;12:e7154. doi: 10.7759/cureus.7154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi X, Shi L, Zhang S. A comparative study on the short-term clinical efficacy of the modified laparoscopic uterine comminution technique and traditional methods. Mol Clin Oncol. 2020;12:237–243. doi: 10.3892/mco.2020.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao H, Zhang Z. Laparoscopy versus laparotomy in the treatment of high-risk endometrial cancer: a propensity score matching analysis. Medicine. 2015;94:e1245. doi: 10.1097/MD.0000000000001245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruan XC, Wong WL, Yeong HQ, Lim YKT. Comparison of outcomes following laparoscopic and open hysterectomy with pelvic lymphadenectomy for early stage endometrial carcinoma. Singapore Med J. 2018;59:366–369. doi: 10.11622/smedj.2018088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Danilyants N, Mamik MM, MacKoul P, van der Does LQ, Haworth L. Laparoscopic-assisted myomectomy: surgery center versus outpatient hospital. J Obstet Gynaecol Res. 2020;46:490–498. doi: 10.1111/jog.14197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chu Y, Zhao X, Han J, Su Y. Physiological signal-based method for measurement of pain intensity. Front Neurosci. 2017;11:279. doi: 10.3389/fnins.2017.00279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bryniarski P, Kasperczyk S, Rajwa P, Stelmach P, Cisowska-Babraj M, Paradysz A. The comparison of oxidative stress effect in classic and tubeless percutaneous nephrolithotomy. Int Urol Nephrol. 2018;50:2145–2152. doi: 10.1007/s11255-018-2003-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yao CA, Lin CH. Treatment with the herbal formulation eefooton slows the progression of chronic kidney disease: a case report. Medicine (Baltimore) 2019;98:e17573. doi: 10.1097/MD.0000000000017573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang R, Wu W, Xu FX, Li J, Gao HP. The effect of laparoscopic myomectomy and open surgery on the endocrine status, immune function and prognosis of patients with uterine fibroids. Adv Mod Biomed. 2020;20:3160–3163. [Google Scholar]
- 26.Wu X, Jiang W, Xu H, Ye XP, Xu CJ. Characteristics of uterine rupture after laparoscopic surgery of the uterus: clinical analysis of 10 cases and literature review. J Int Med Res. 2018;46:3630–3639. doi: 10.1177/0300060518776769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ciebiera M, Wrzosek M, Wojty a C, Łoziński T, Nowicka G, Jakiel G, Głowala M, Włodarczyk M. Oestrogen receptor alpha pvu ii polymorphism and uterine fibroid incidence in Caucasian women. Prz Menopauzalny. 2018;17:149–154. doi: 10.5114/pm.2018.81735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boudová B, Mára M, Dundr P, Gregová M, Lisá Z, Kužel D. Uterine leiomyomas with bizarre nuclei: analysis of 37 cases after laparoscopic or open myomectomy. Ceska Gynekol. 2019;84:324–330. [PubMed] [Google Scholar]
- 29.Zhu R. Comparison of the efficacy of laparoscopic myomectomy and open myomectomy in the treatment of uterine fibroids. J Xinxiang Med Coll. 2018;35:1094–1096. [Google Scholar]