Abstract
Introduction
Violence is a major cause of death worldwide among youth. The highest mortality rates from youth violence occur in low and middle-income countries (LMICs). We sought to identify risk factors for violent re-injury and emergency centre (EC) recidivism among assault-injured youth in South Africa.
Methods
A prospective follow up study of assault injured youth and controls ages 14–24 presenting for emergency care was conducted in Khayelitsha, South Africa from 2016 to 2018. Sociodemographic and behavioral factors were assessed using a questionnaire administered during the index EC visit. The primary outcomes were return EC visit for violent injury or death within 15 months. We used multivariable logistic regression to compute adjusted odds ratios (OR) and 95% confidence intervals (CI) of associations between return EC visits and key demographic, social, and behavioral factors among assault-injured youth.
Results
Our study sample included 320 assault-injured patients and 185 non-assault-injured controls. Of the assault-injured, 80% were male, and the mean age was 20.8 years. The assault-injured youth was more likely to have a return EC visit for violent injury (14%) compared to the control group (3%). The non-assault-injured group had a higher mortality rate (7% vs 3%). All deaths in the control group were due to end-stage HIV or TB-related complications. The strongest risk factors for return EC visit were prior criminal activity (OR = 2.3, 95% CI = 1.1–5.1), and current enrollment in school (OR = 2.1, 95% CI = 1.0–4.6). Although the assault-injured group reported high rates of binge drinking (73%) at the index visit, this was not found to be a risk factor for violence-related EC recidivism.
Discussion
Our findings suggest that assault-injured youth in an LMIC setting are at high risk of EC recidivism and several sociodemographic and behavioral factors are associated with increased risk. These findings can inform targeted intervention programs.
Keywords: Violence, Prevention, Adolescent, Emergency medicine, Global health
African relevance
-
•
This is a prospective follow up study of assault injured youth and controls ages 14–24 presenting for emergency care in Khayelitsha, South Africa
-
•
Assault-injured youth are more likely to return for emergency care as compared to non-assault injured youth
-
•
Males, students, marijuana users, gang members, those with a criminal history, and an initial injury with penetrating trauma had a greater likelihood of emergency care recidivism
-
•
These novel findings from a low-and-middle income African country correspond to similar sociodemographic and behavioral risk factors for ED recidivism in high income countries
Introduction
Youth violence is a major societal health burden worldwide. Injuries as a result of youth violence have severe health consequences, including death. An estimated 200,000 homicides occur annually among youth, ages 10–29 years [1]. In addition to premature death and disability, violence among youth has a profound negative effect on psychological and social functioning and perpetuates violent behavior into the next generation 2., 3.. Given the destructive toll of violence, one of the United Nations' (UN) 2030 sustainable development goals is to “Significantly reduce all forms of violence and related death rates everywhere.” [4].
Unfortunately, low- and middle- income countries (LMICs) bear the greatest burden of youth violence, where 85% homicides among youth occur [1]. In South Africa, youth ages 15–29 years are at a significantly greater risk of violence with a reported homicide rate of 69.9/100,000, five times higher than the global average 5., 6.. The concentration of youth violence is particularly troubling in Khayelitsha, a post-apartheid township outside of Cape Town, South Africa. In this region, death rates due to violence in young men reach 451/100,000—25 times higher than the global average [7].
Younger patients commonly use the emergency centre (EC) as their primary source of care, especially for violence-related injuries 8., 9., 10., 11.. Further, assault is the most common cause of injury in youth evaluated in emergency centres surrounding Cape Town [12]. Therefore, the EC provides an ideal opportunity to explore risk factors for violence among youth and subsequently to deploy targeted interventions at the bedside (teachable moments) or provide linkages to community programs that seek to prevent future violence 13., 14., 15..
Understanding risk factors for assault injured youth who present to ECs is a pivotal first step for developing targeted interventions [15]. Youth violence mortality and morbidity is driven by sociodemographic factors and risky behaviors, such as alcohol use, exposure to violence on television, and negative peer pressure [16]. However, youth violence research, focused in EC settings, is typically conducted in high-income countries 17., 18., 19., while data from EC settings in LMICs is scarce. Our recent study, in an LMIC setting, found that binge drinking of alcohol, criminal history, and history of prior assault were associated with assault injuries in youth [20].
Of particular concern is that youth treated in the EC for assault are at higher risk for violent re-injury and death, representing a uniquely high risk group 21., 22.. Cunningham et al. found that assault-injured youth were twice as likely to return within 24 months of an index visit, and most within the first 6 months [21]. Understanding risk factors for EC recidivism or death in this higher risk population can better inform interventions to prevent future injury and mortality. There is an immediate need for more research in LMICs on risk factors, recidivism, and outcomes in assault injured youth who present to ECs.
In this study, we sought to describe the rates of EC recidivism and death among assault-injured youth and their non-assault-injured controls in the fifteen months after their index EC visit. We aimed to identify demographic and behavioral risk factors for violence-related EC recidivism among the assault- injured youth. Our hypothesis was that assault injured youth would have a higher rate of EC recidivism when compared to non-assault injured youth presenting to the same EC. We hope this data can be used in the future to identify high-risk youth and inform contextually appropriate and targeted violence prevention initiatives.
Methods
We conducted a prospective follow-up study of youth presenting to emergency care facilities in Khayelitsha township outside of Cape Town, South Africa. Initial cohort data was collected in 2016 and follow up data was collected in 2018. The study design and methods and baseline characteristics of participants have been previously described [20]. Approval of this human subject's research was obtained from the University of North Carolina at Chapel Hill Institutional Review Board, Stellenbosch University Health Research Ethics Committee, Western Cape Provincial Research Health Committee, and the Cape Town City Health Department.
We selected a convenience sample of adolescents and emerging adults (ages 14–24 years) presenting to two 24-hour public health facilities, Khayelitsha Hospital, a 240-bed district level hospital with an emergency centre and Site B Community Health Centre, a provincial primary health facility with a small trauma unit. On weekends and after hours, Khayelitsha township is served primarily by these two facilities [20].
All assault injured-youth between the ages of 14–24 were considered for inclusion. Exclusion criteria included suicide attempt or primary psychiatric complaint, sexual assault, child abuse as well as any patient with altered mental status related to head injury or intoxication. These latter patients could be included in the study if their treating physician deemed that they had returned to baseline during their stay in the EC [20].
Participants were divided into assault injured and “control” groups (seen for medical complaint or accidental injury) based on the reason of the index EC visit. We aimed to enroll assault injured patients and controls on a 1:1 gender-matched basis.
We enrolled participants between Friday 7 PM and Monday 7 AM when most assault injuries were seen, over a fifteen-week period. Paper, electronic charts as well as a system-wide death registry were then reviewed fifteen months later for return EC visits and/or documentation of death. Power calculations for our sample size were guided by provincial prevalence rates of baseline characteristics drawn from the Youth Risk Behavioral Survey(YRBS), but ultimately determined retrospectively, due absence of relevant data on the primary outcome [23].
The primary outcomes were return EC visit for violent injury or documentation of death within the fifteen-month follow-up period. We also analyzed a composite outcome of both EC recidivism and mortality. Sociodemographic and behavioral factors were assessed at the index visit using a questionnaire primarily derived from the South African National Youth Risk Behaviour Survey [23]. Participants completed an electronic questionnaire in the EC using a tablet provided to them by research staff.
Frequency counts and proportions of baseline characteristics and outcomes were computed for assault-injured youths. For comparison, these descriptive statistics were also produced for the control group. Kaplan-Meier survival curves comparing composite outcomes over fifteen months between the two groups were created. The log-rank test was used to test for a statistical difference between Kaplan-Meier curves. We used multivariable logistic regression to compute adjusted odds ratios (OR) and 95% confidence intervals (CI) of associations between return ED visits and key demographic, social, and behavioral factors among assault-injured youth. We decided a priori to include covariates of broad categories that could be used for potential risk stratification or screening for targeted interventions. Complete case analysis excluded observations with missing covariate data from the regression model. Statistical analyses were conducted in R 3.3.2 and SAS 9.4 (SAS Institute, Cary NC). A p value less than 0.05 was considered statistically significant. Since the study was not powered to test a specific risk factor, statistical testing was performed as an exploratory analysis. We also interpreted results based on the magnitude of the estimated OR and their precision as indicated by 95% CI.
Results
Of the 516 participants enrolled at baseline, 505 (97.8%) participants had complete follow-up data and were included in the analysis. Eleven participants without follow-up data were excluded from the analysis. Our study sample included 320 assault-injured and 185 non-assault-injured control patients. Among the assault-injured, 80% were male and the mean age was 20.8 years (Table 1). Assault-injured patients reported higher rates of substance abuse including binge-alcohol use (75% vs 29%) and marijuana use (39% vs 18%). They were also more likely than controls to report gang membership (13% vs 5%) or criminal history (33% vs 8%). The majority (79%) of assault injuries leading to the index EC visit were due to penetrating trauma.
Table 1.
Baseline characteristics for assault-injured and control (accidental injury, medical complaint) youth (N = 505).
| Characteristics | Assault-injured group (N = 320) |
Control groupa (N = 185) |
Missing |
||
|---|---|---|---|---|---|
| No. | % | No. | % | No. | |
| Age (in years) | |||||
| 14–17 | 38 | 12% | 56 | 30% | 0 |
| 18–20 | 85 | 27% | 36 | 19% | 0 |
| 21–24 | 197 | 62% | 93 | 50% | 0 |
| Male gender | 256 | 80% | 108 | 58% | 0 |
| Currently in school | 99 | 31% | 85 | 46% | 0 |
| Homeless in past 30 days | 39 | 12% | 10 | 5% | 2 |
| Difficulty with finances | 139 | 44% | 66 | 36% | 2 |
| Member of a religious group (any church or denomination) | 117 | 37% | 120 | 65% | 3 |
| Depressionb in past 6 months | 93 | 29% | 50 | 27% | 2 |
| Any tobacco use in past 30 days | 187 | 58% | 47 | 25% | 0 |
| Binge alcohol use in past 30 days | 238 | 75% | 53 | 29% | 3 |
| Any marijuana use in lifetime | 125 | 39% | 34 | 18% | 0 |
| Currently in a gang | 40 | 13% | 10 | 5% | 5 |
| Criminal historyc | 104 | 33% | 15 | 8% | 7 |
| Injured from a fight in past 6 months | 152 | 48% | 27 | 15% | 1 |
| Initial assault mechanism | 11 | ||||
| Penetrating | 243 | 79% | n/a | ||
| Blunt | 66 | 21% | |||
Accidental injury or medical complaint.
Ever felt so sad or hopeless that stopped doing usual activities for 2 or more weeks.
Ever been arrested, spent a night in jail, or been convicted.
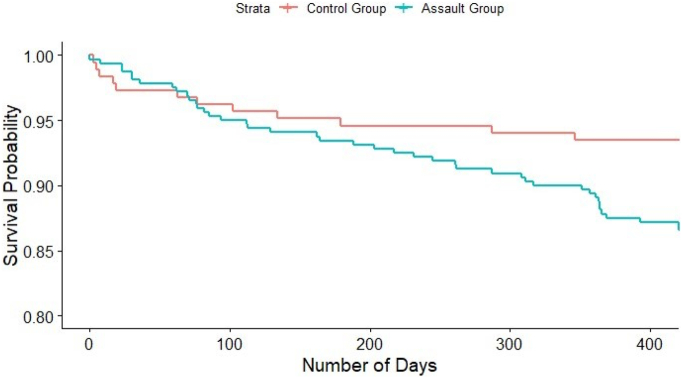
Overall, 12% of the study population experienced either a return EC visit for violent injury or died over the fifteen-month follow-up period (Table 2). We observed a higher percentage of assault-injured youth had a return EC visit (14%) compared to the control group (3%). However, mortality was greater among controls (4%) versus assault-injured youth (1%). All deaths in the control group were due to end-stage HIV or tuberculosis(TB)-related complications. Kaplan-Meier survival curves of the composite outcome illustrate the early mortality in the controls whereas the return EC visits occurred among the assault-injured youth at a steady rate over the first twelve months (Fig. 1). The log-rank test found a statistical difference between the curves (p = 0.016).
Table 2.
Frequency of return EC visits and deaths within 15 months.
| Outcomes | Overall N = 505 |
Group |
||||
|---|---|---|---|---|---|---|
| Assault-injured N = 320 |
Control N = 185 |
|||||
| No. | % | No. | % | No. | % | |
| Returned to ED for violent injury | 51 | 10% | 45 | 14% | 6 | 3% |
| Median (IQR), in days | 188 | 77–359 | 217 | 77–361 | 118 | 83–168 |
| Died | 10 | 2% | 3 | 1% | 7 | 4% |
| Median (IQR), in days | 18 | 6–150 | 71 | 36–124 | 17 | 6–153 |
| Composite Endpointa | 59 | 12% | 46 | 14% | 13 | 7% |
| Median (IQR), in days | 164 | 67–349 | 210 | 76–360 | 77 | 17–179 |
Composite Endpoint: returned to ED for violent injury or died within 15 months.
Fig. 1.
Kaplan-Meier survival curves for time until return EC visit or death between assault-injured and control groups.
The multivariable logistic regression model revealed meaningful risk factors for EC recidivism among assault-injured youth (Table 3). Males were more likely to return to the EC for a violent injury after initial presentation (OR = 1.9, 95% CI = 0.7–5.0) although the estimate was relatively imprecise due to the small number of females in the study sample. Criminal history was strongly associated (OR = 2.3, 95% CI = 1.1–5.1) whereas past injury from fighting was not (OR = 1.0, 95% CI = 0.5–2.1). While tobacco use and alcohol abuse did not appear to be associated (OR = 0.9, 95% CI = 0.4–2.0 and OR = 0.7, 95% CI = 0.3–1.6, respectively), lifetime marijuana use was modestly associated with return EC visit (OR = 1.6, 95% CI = 0.7–3.6). Penetrating trauma as the mechanism of index injury (OR = 1.7, 95% CI = 0.6–4.4) and gang membership (OR 1.7, 95% CI = 0.6–4.3) may be modestly associated. Those currently in school had a higher likelihood of return EC visit (OR = 2.1, 95% CI = 1.0–4.6).
Table 3.
Demographic, social, and behavioral risk factors for return EC visit among assault injured youth (N = 297).
| Returned to ED |
|
|---|---|
| OR (95% CI) | |
| Age group | |
| 14–17 years | 0.9 (0.3–2.7) |
| 18–20 years | 0.8 (0.3–1.8) |
| 21–24 years (ref) | 1 |
| Male gender | 1.9 (0.7–5.0) |
| Currently in school | 2.1 (1.0–4.6) |
| Homeless in past 30d | 0.7 (0.2–2.5) |
| Financial struggles | 0.9 (0.4–1.8) |
| Member of religious group | 1.0 (0.5–2.1) |
| Depression in past 6 m | 0.4 (0.2–1.0) |
| Any tobacco use, past 30d | 0.9 (0.4–2.0) |
| Any binge alcohol use, past 30d | 0.7 (0.3–1.6) |
| Any marijuana use, lifetime | 1.6 (0.7–3.6) |
| Currently in a gang | 1.7 (0.6–4.3) |
| Injured from fight in past 6 m | 1.0 (0.5–2.1) |
| Criminal history | 2.3 (1.1–5.1) |
| Assault mechanism (penetrating vs. non-penetrating) | 1.7 (0.6–4.4) |
Discussion
This is the first known study in a limited resource setting like South Africa, to evaluate risk factors for EC recidivism and death among assault injured youth presenting to an emergency centre. This study provides clarity for identification of high-risk individuals in order to develop targeted violence prevention initiatives. Overall, our findings suggest that 1) assault injured youth are more likely to return to the EC as compared to non-assault injured youth, 2) return ED visits occurred at a steady rate across the first twelve months following initial assault injury, and 3) males, students, marijuana users, gang members, those with a criminal history, and an initial injury with penetrating trauma trended towards a greater likelihood of EC recidivism. These findings are consistent with large scale studies conducted in HIC EC settings 21., 24., 25..
We found that youth in Khayelitsha who present for emergency care with assault-related injuries are more likely to die or experience a violent reinjury within fifteen months of their index visit, based on a statistically significant difference between Kaplan-Meier curves. While this represents a novel finding for an LMIC setting, it is not a finding unique only to these settings. Multiple studies in the United States (US) of youth following violent injury demonstrated EC recidivism or death rates between 27 and 37% at five years 22., 24. and nearly twice the odds of return compared to accidental injuries (OR 1.93, 95% CI 1.66–2.26) [22]. Our recidivism rate was lower at 14%, however, was measured at only fifteen months post-injury. In this shorter timeframe, we found a substantially greater likelihood of EC recidivism in assault-injured compared to no-assault-injured patients (14% vs. 3%). It is reasonable to assume, based on this trajectory of the Kaplan Meier curve, that our cohort's recidivism rate, at five years, would be similar or greater than prior studies conducted in HICs.
Our findings suggest that individuals with the highest risk for EC recidivism or death in our study were male, attended school, used marijuana, were currently in a gang, had a criminal history, and suffered an initial assault characterized by penetrating injury. Our findings correlate with general risk factors for youth violence in LMICs, based on a meta-analysis of over 480,000 individuals from 60 countries [16]. Similarities are also seen among risk factors specifically related to EC recidivism, although from a HIC setting. For example, a large study in Los Angeles, United States found that patients ages 10–30 years with the greatest risk for EC recidivism were male, used illicit drugs, and suffered from penetrating trauma [25].
One third of our study participants have engaged in criminal activity as defined as having “ever been arrested, spent a night in jail, or been convicted.” Criminal history was significantly associated with EC recidivism. Several studies in HICs have demonstrated reductions in violence and criminal activity as a result of participation in hospital-based interventions programs, among violent injured youth 26., 27.. Since youth involved in criminal activities have increased contact with the judicial system, this represents another opportunity where high risk youth could be assessed for appropriate court-ordered violence intervention. There is evidence that matching youth offenders with an intervention related to their unique criminogenic risk factors can reduce judicial recidivism [28].
Members of gangs were twice as likely to present to the EC for violent injury [20] and appear to have a higher EC recidivism. Reported gang membership was a minority of our sample (13%) but nonetheless, gangs are considered a leading cause of violence against and between children and youth in Khayelitsha [29]. An EC-based study with a brief therapist intervention (of which 8% of study participants were gang members), reported a reduction in the frequency of violent aggression and increased self-efficacy for avoiding fighting [14]. However, outcomes in the subset of youth with criminal histories or involvement with gangs were not reported. The role and efficacy of EC-based interventions in targeting criminal history and gang membership for screening and/or referral remains unclear.
Youth who use drugs and alcohol are more likely to engage in high-risk and violent behavior 17., 30., 31., 32., 33.. As reported in the Youth Risk Behavioral Survey (grades 8–11th), youth in Khayelitsha have twice the rate of binge drinking compared to other youth in the Western Cape Province [23]. The rate of binge drinking in our cohort of assault injured youth was much higher than non-assault injured youth, at 73% vs 29%, OR 6.74 (95% CI 4.52–10.05) [20] and higher than what has been reported in an urban HIC setting (23.5% vs 17.8% [OR 1.42]) [18]. In our study, alcohol abuse was not significantly associated with EC recidivism (at fifteen months). This result should be interpreted with the understanding that alcohol in general is a known risk factor for youth violence, and this population has a high baseline prevalence (75%) of alcohol use.
In a HIC setting, compared to non-assault injured controls, assault-injured youth have twice the odds of using marijuana [18]. Further, nearly all assault injured youth that return to the EC, for any type of injury, use marijuana [21]. Illicit drug use has been correlated with fighting and youth violence in LMICs [16], and between 0.5% to 37.6% of adolescents living in LMICs report using marijuana 34., 35.. Among all youth in the Western Cape, 13% reported a history of using marijuana [23] and 39% of our assault injured cohort reported using marijuana. Although not statistically significant, a modest association between use of marijuana and EC recidivism among assault injured youth was observed (OR 1.6, 95% CI: 0.7–3.6). The rates of both marijuana and alcohol use in this population are concerning given the known social and health risks of substance abuse, including violent behavior.
Our study found that youth returning to the EC in Khayelitsha for assault injury were more likely to be students than not to be students (OR 2.1, 95% CI: 1.0–4.6). Prior research demonstrates that lack of school attendance or failing school is a risk factor for future injury [36]. However, the role of school attendance as a risk or protective factor for perpetuating violence is more nuanced than simply “attending”. Youth violence in LMICs has been correlated with weak attachment to school, poor academic achievement, “not studying”, and public schools and location in an urban area [16]. However, positive school experiences, including good academic achievement, support by teachers, clear classroom rules and an overall positive school climate can be protective against violence [37]. Since we did not assess school experiences specifically, It is not clear how school attendance relates to a higher odds of assault in this population, although is likely multifactorial.
Our study was conducted on weekends and nights in the emergency centre and therefore represents “community violence” rather than violence occurring at school or en route to/from school. While the injuries in our study did not occur specifically at school, school violence and bullying is known to spill over into community settings [38]. Gang related violence may also be a factor, as a 2014 report about Khayelitsha cited concerns of gang activity and violence around schools [29]. It is likely that interconnected youth social networks between school and the community play a significant role in the violence among our study participants, especially since at least 55% of the conflicts among our cohort occurred between known individuals [20]. Regardless of the specific aspects of school attendance that confer risk of future violence in our cohort, it raises possible (although complex) possibilities for intervention.
There were no clear protective factors elucidated in this study. Variables have been proposed to be protective against future violence including, at the individual-level (anger control skills, nonaggression social beliefs), family-level (close relationship with a parent, low physical punishment, above average socioeconomic status of family), school factors (positive school affiliation, absence of gangs), peer factors (nondeviant friends, involvement in religious groups, being socially isolated) and neighborhood factors (non-violent and nondeprived neighborhood) 15., 37.. Only one factor, “feeling sad or hopeless within the past six months”, a screening question for depression, was negatively associated with EC recidivism, although a protective effect is unclear. This could potentially be related to social isolation; however, we did not assess this. Over 30% of our sample suffer from sadness/depression which is a concerning feature on its own. The complex interplay of depression and violence warrants further investigation to understand this high level of “sadness” among this population of youth.
This study utilized a convenience sample, enrolling on weekends when most assault injured patients present for care. However, this excludes assaults and non-assault injuries occurring during the weekdays and likely underestimates school-related violent injuries. Non-assault-injured males were underrepresented because there were relatively few non-assault-injured males presenting to the ECs during times of enrollment.
A relatively smaller number of females were enrolled (28%) [20], and while this is consistent with findings that males are more likely to present for injuries (WHO) [1], it limits the characterization of EC recidivism among females. Khayelitsha has dedicated clinical sites, separate from ECs, where sexual assault patients are evaluated. It is therefore likely that many assault-injured females who have sustained both sexual and physical violence were missed in our study. Additionally, since our study was not designed to characterize the nature of the injury among EC recidivists, we cannot conclude the type of violence (such as intimate partner violence) among females. The rate of Femicide (including intimate partner related) is disturbingly common in South Africa (12.9/100,000) [39] and EC visits are opportunities for screening and prevention of future violence against women. Most screening instruments used for intimate partner violence have been developed in HIC's and further work needs to be done to develop contextually appropriate tools for LMIC settings [40].
Our recidivism rate appears consistent among literature in HIC's. However, it is possible that we have underreported the true number of violent re-injuries, since we assessed only two locations for return (same EC or community health centre). Patients are encouraged by provincial health policy to seek care at local clinics and hospitals within their catchment area and the nearest medical facility outside of Khayelitsha is 8 km away. The majority of patients in this community rely on public transportation, which does not operate at night when most trauma presents to the hospital. While it is unlikely that youth traveled outside of the area to present for emergency care, it remains a possibility and we did not follow up with these participants directly. Additionally, the number of deaths could also be higher than we reported since we ascertained death from the patient's hospital chart. We did not cross reference death rates through follow up with family members, other hospitals, or local morgue data.
This was an observational study and was not designed to statistically test a specific risk factor. Instead, we focused on a pre-specified set of broad putative factors that could be relevant to risk stratification and screening in the EC. However, this study establishes a foundation for future research into modifiable factors among this high risk population. Finally, this study explores a single community in South Africa that is known to have high rates of violence. However, our results appear to correlate with findings from urban settings of HICs and general risk factors for youth violence in LMIC's, suggesting good generalizability of our results across similar settings.
It is possible to prevent future violence among assault injured youth [15]. Reasons that youth engage in violence are complex, multi-factorial and highly dependent on the environment in which they are born and live 41., 42.. Although addressing any single risk factor may not be sufficient to reduce future violence, utilization of screening tools in the EC may be a feasible option for identification and referral for effective intervention for high risk individuals 15., 43.. For example, EC based screening, (i.e. brief intervention and referral to treatment (SBIRT)) show that brief, face to face interventions by doctors, nurses and/or social workers who have specialized training, demonstrate reduction in alcohol abuse among patients 44., 45.. Given the prevalence of alcohol abuse by youth in Khayelitsha, an EC-based “SBIRT” may be a logistically and financially feasible approach for this specific risk factor. However, this approach may also be feasible for other risk factors for youth violence and EC recidivism. While in-hospital based intervention programs are successful at reducing EC recidivism for traumatic injuries 46., 47., patients discharged from the EC will miss that opportunity. A combination of EC-based screening for targeted risk factors (with linkage to community services) and in-hospital based intervention programs would likely provide the greatest benefit to this population.
Effective interventions for youth violence can be initiated during early childhood education and continue through all school ages, involve family, as well as community and public health programming 42., 48.. Additionally, the social determinants of health, which aggravate risk factors for violence, should be continually addressed within this community.
Our findings suggest that assault-injured youth in LMICs are at risk of EC recidivism and several sociodemographic and behavioral factors are associated with increased risk. While there are limited studies related to youth violence and EC recidivism in LMICs, our findings appear congruent with studies in HIC settings. Future research into risk factors and interventions to address them are needed for this vulnerable and high risk population.
Dissemination of results
Results from this study were presented to provincial authorities and have been informally shared with clinical staff at the data collection site.
Authors' contribution
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: SCL contributed 50%; MDP 10%, SL, ABG, PR, IM, and DVH 5% each; and JM 15%. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declare no conflicts of interest.
References
- 1.World Health Organisation Global status on violence prevention 2014 [Internet] 2014. https://www.who.int/violence_injury_prevention/violence/status_report/2014/en/ Available from:
- 2.World Health Organization . WHO library. 2015. Preventing youth violence: an overview of the evidence [Internet] p. 100.https://bit.ly/2IYPQLx Available from: [Google Scholar]
- 3.Black D.S., Sussman S., Unger J.B. A further look at the intergenerational transmission of violence: witnessing interparental violence in emerging adulthood. J Interpers Violence. 2010;25(6):1022–1042. doi: 10.1177/0886260509340539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowman B., Matzopoulos R., Butchart A., Mercy J.A. The impact of violence on development in low- to middle-income countries. Int J Inj Contr Saf Promot. 2008;15(4):209–219. doi: 10.1080/17457300802417911. [DOI] [PubMed] [Google Scholar]
- 5.Matzopoulos R., Prinsloo M., Pillay-Van Wyk V., Gwebushe N., Mathews S., Martin L.J. Injury-related mortality in South Africa: a retrospective descriptive study of postmortem investigations. Bull World Health Organ. 2015;93(5):303–313. doi: 10.2471/BLT.14.145771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations Office on Drugs and Crime . Unodoc; Vienna: 2019. Global study on homicide 2019 [internet]http://www.ncbi.nlm.nih.gov/pubmed/22057928 Available from: [Google Scholar]
- 7.Groenewald P., Bradshaw D., Daniels J., Matzopoulos R., Bourne D., Blease D. Cause of death and premature mortality in Cape Town, 2001-2006 [Internet] 2008. www.mrc.ac.za/bod.bod.htm%5Cnwww.capetown.gov.za/health%5Cnwww.capegateway.gov.za/health Available from:
- 8.Tang N., Stein J., Hsia R.Y., Maselli J.H., Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA - J Am Med Assoc. 2010;304(6) doi: 10.1001/jama.2010.1112. 664-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss A.L., D’Angelo L.J., Rucker A.C. Adolescent use of the emergency department instead of the primary care provider: who, why, and how urgent? J Adolesc Health. 2014;54(4):416–420. doi: 10.1016/j.jadohealth.2013.09.009. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 10.Fortuna R.J., Robbins B.W., Mani N., Halterman J.S. Dependence on emergency care among young adults in the United States. J Gen Intern Med. 2010;25(7) doi: 10.1007/s11606-010-1313-1. 663-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziv A., Boulet J., Slap G. Emergency department utilization by adolescents in the United States ment component of the 1994 National Hospital Ambula- Pediatrics. 1998;101(6) doi: 10.1542/peds.101.6.987. 987-94. [DOI] [PubMed] [Google Scholar]
- 12.Nicol A., Knowlton L.M., Schuurman N., Matzopoulos R., Zargaran E., Cinnamon J. Trauma surveillance in Cape Town, South Africa: an analysis of 9236 consecutive trauma center admissions. JAMA Surg. 2014;149(6):549–556. doi: 10.1001/jamasurg.2013.5267. [DOI] [PubMed] [Google Scholar]
- 13.Johnson S.B., Bradshaw C.P., Wright J.L., Haynie D.L., Simons-Morton B.G., Cheng T.L. Characterizing the teachable moment: is an emergency department visit a teachable moment for intervention among assault-injured youth and their parents? Pediatr Emerg Care. 2007;23(8):553–559. doi: 10.1097/PEC.0b013e31812c6687. [DOI] [PubMed] [Google Scholar]
- 14.Carter P.M., Walton M.A., Zimmerman M.A., Chermack S.T., Roche J.S., Cunningham R.M. Efficacy of a universal brief intervention for violence among urban emergency department youth. Acad Emerg Med. 2016;23(9):1061–1070. doi: 10.1111/acem.13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cunningham R., Knox L., Fein J., Harrison S., Frisch K., Walton M. Before and after the trauma bay: the prevention of violent injury among youth. Ann Emerg Med. 2009;53(4):490–500. doi: 10.1016/j.annemergmed.2008.11.014. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 16.de Ribera O.S., Trajtenberg N., Shenderovich Y., Murray J. Correlates of youth violence in low- and middle-income countries: a meta-analysis. Aggress Violent Behav. 2019;49(July):101306. doi: 10.1016/j.avb.2019.07.001. [Internet] Available from: [DOI] [Google Scholar]
- 17.Carter P.M., Cranford J.A., Buu A., Walton M.A., Zimmerman M.A., Goldstick J. Daily patterns of substance use and violence among a high-risk urban emerging adult sample: results from the Flint Youth Injury Study. Addict Behav. 2020;101 doi: 10.1016/j.addbeh.2019.106127. (September 2019) Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunningham R.M., Ranney M., Newton M., Woodhull W., Zimmerman M., Walton M.A. Characteristics of youth seeking emergency care for assault injuries. Pediatrics. 2014;133(1) doi: 10.1542/peds.2013-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng T.L., Schwarz D., Brenner R.A., Wright J.L., Fields C.B., O’Donnell R. Adolescent assault injury: risk and protective factors and locations of contact for intervention. Pediatrics. 2003;112(4):931–938. doi: 10.1542/peds.112.4.931. [DOI] [PubMed] [Google Scholar]
- 20.Leeper S., Lahri S., Myers J., Patel M., Reddy P., Martin I.B. Assault-injured youth in the emergency centres of Khayelitsha, South Africa: baseline characteristics & opportunities for intervention. Injury. 2019;50:2220–2227. doi: 10.1016/j.injury.2019.10.014. [cited 2019 Dec 17] Available from: [DOI] [PubMed] [Google Scholar]
- 21.Cunningham R.M., Carter P.M., Ranney M., Zimmerman M.A., Blow F.C., Booth B.M. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury a 2-year prospective cohort study. Vol. 48109. 2015. pp. 63–70. (1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCoy A.M., Como J.J., Greene G., Laskey S.L., Claridge J.A. A novel prospective approach to evaluate trauma recidivism: the concept of the past trauma history. J Trauma Acute Care Surg. 2013;75(1):116–121. doi: 10.1097/TA.0b013e31829231b7. [DOI] [PubMed] [Google Scholar]
- 23.Reddy S., James S., Sewpaul R., Sifunda S., Ellahebokus A., Kambaran N. South African Medical Research Council; Cape Town: 2013. Umthente Uhlaba Usamila - The 3rd South African National Survey, Youth Risk Behaviour 2011 [Internet]. Health Promotion Research and Development Unit of the Medical Research Council and the Population Health, Health Systems and Innovation (PHHSI)https://africacheck.org/wp-content/uploads/2018/10/3rd-Annual-Youth-Risk-Survey-2011.pdf 180 p. Available from: [Google Scholar]
- 24.Kao A.M., Schlosser K.A., Arnold M.R., Kasten K.R., Colavita P.D., Davis B.R. Trauma recidivism and mortality following violent injuries in young adults. J Surg Res. 2019;237:140–147. doi: 10.1016/j.jss.2018.09.006. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 25.Christopher Foran M.D., Damon Clark M.D., Kenji Inaba M.D., Morgan Schellenberg M.D., Niquelle Brown Wade M.S., Demetrios Demetriades M.D. Youth and young adult victims of interpersonal violence at La County USC Medical Center: a review of epidemiology and recidivism. Am Surg. 2019;85(10):1166–1170. [PubMed] [Google Scholar]
- 26.Cooper C., Eslinger D.M., Stolley P.D. Hospital-based violence intervention programs work. J Trauma - Inj Infect Crit Care. 2006;61(3) doi: 10.1097/01.ta.0000236576.81860.8c. 534-7. [DOI] [PubMed] [Google Scholar]
- 27.Shibru D., Zahnd E., Becker M., Bekaert N., Calhoun D., Victorino G.P. Benefits of a hospital-based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–689. doi: 10.1016/j.jamcollsurg.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 28.Vieira T.A., Skilling T.A., Peterson-Badali M. Matching court-ordered services with treatment needs: predicting treatment success with young offenders. Crim Justice Behav. 2009;36(4):385–401. [Google Scholar]
- 29.Kayelitsha Commission Towards a Safer Khayelitsha. 2014. http://www.saflii.org/khayelitshacommissionreport.pdf Available from:
- 30.Goldstick J.E., Lipton R.I., Carter P., Stoddard S.A., Newton M.F., Reischl T. The effect of neighborhood context on the relationship between substance misuse and weapons aggression in urban adolescents seeking ed care. Subst Use Misuse. 2015;50(5):674–684. doi: 10.3109/10826084.2014.998235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.RJR Blair. What role can cognitive neuroscience play in violence prevention? Aggress Violent Behav. 2019;46(February):158–164. doi: 10.1016/j.avb.2019.02.008. [Internet] [DOI] [Google Scholar]
- 32.Schulenberg J., Merline A., Johnston L., O’Malley P., Bachman J., Laetz V. Trajectories of marijuana use during transition to adulthood: the big picture based on national panel data. J Drug Issues. 2005;35(2) doi: 10.1177/002204260503500203. 255-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organisation Global status report on alcohol and health 2018 [Internet] 2018. https://www.who.int/substance_abuse/publications/global_alcohol_report/en/ Available from:
- 34.Ashdown-Franks G., Sabiston C.M., Vancampfort D., Smith L., Firth J., Solmi M. Cannabis use and physical activity among 89,777 adolescents aged 12-15 years from 21 low- and middle-income countries. Drug Alcohol Depend. 2019;205(August) doi: 10.1016/j.drugalcdep.2019.107584. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 35.Carvalho A.F., Stubbs B., Vancampfort D., Kloiber S., Maes M., Firth J. Cannabis use and suicide attempts among 86,254 adolescents aged 12–15 years from 21 low- and middle-income countries. Eur Psychiatry. 2019;56:8–13. doi: 10.1016/j.eurpsy.2018.10.006. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 36.Sege R., Stringham P., Short S., Griffith J. Ten years after: examination of adolescent screening questions that predict future violence-related injury. J Adolesc Health. 1999;24(6):395–402. doi: 10.1016/s1054-139x(98)00150-5. [DOI] [PubMed] [Google Scholar]
- 37.Lösel F., Farrington D.P. Direct protective and buffering protective factors in the development of youth violence. Am J Prev Med. 2012;43(2 SUPPL. 1) doi: 10.1016/j.amepre.2012.04.029. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 38.UNESCO School violence and bullying: global status and trends, drivers and consequences Current [Internet] 2017. http://www.ungei.org/global_status_on_school_violence(1).pdf 56 p. Available from:
- 39.Abrahams N., Mathews S., Martin L.J., Lombard C., Jewkes R. Intimate partner femicide in South Africa. PLoS Med. 2013;10(4) doi: 10.1371/journal.pmed.1001412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmad I., Ali P.A., Rehman S., Talpur A., Dhingra K. Intimate partner violence screening in emergency department: a rapid review of the literature. J Clin Nurs. 2017;26(21–22):3271–3285. doi: 10.1111/jocn.13706. [DOI] [PubMed] [Google Scholar]
- 41.Garbarino J. The context of youth violence: resilience, risk, and protection. Praeger Publishers; CT: 2001. Making sense of senseless youth violence. [Google Scholar]
- 42.David-Ferdon Corinne, Simon T. Preventing youth violence : opportunities for action. Natl Cent Inj Prev Control Centers Dis Control Prev. 2014:1–54. [Google Scholar]
- 43.Rogers S.C., Borrup K., Parikh C., Saleheen H., Lapidus G., Smith S. Can a youth violence screening tool be used in a pediatric emergency department setting? J Trauma Acute Care Surg. 2012;73(4 Suppl 3):243–247. doi: 10.1097/TA.0b013e31826b0040. [DOI] [PubMed] [Google Scholar]
- 44.Cunningham R.M., Chermack S.T., Ehrlich P.F., Carter P.M., Booth B.M., Blow F.C. Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatrics. 2015;136(4) doi: 10.1542/peds.2015-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barata I.A., Shandro J.R., Montgomery M., Polansky R., Sachs C.J., Duber H.C. Effectiveness of SBIRT for alcohol use disorders in the emergency department: a systematic review. West J Emerg Med. 2017;18(6):1143–1152. doi: 10.5811/westjem.2017.7.34373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aboutanos M.B., Jordan A., Cohen R., Foster R.L., Goodman K., Halfond R.W. Brief violence interventions with community case management services are effective for high-risk trauma patients. J Trauma - Inj Infect Crit Care. 2011;71(1):228–237. doi: 10.1097/TA.0b013e31821e0c86. [DOI] [PubMed] [Google Scholar]
- 47.Cordovilla-Guardia S., Fernández-Mondéjar E., Vilar-López R., Navas J.F., Portillo-Santamaría M., Rico-Martín S. Effect of a brief intervention for alcohol and illicit drug use on trauma recidivism in a cohort of trauma patients. PLoS One. 2017;12(8):1–17. doi: 10.1371/journal.pone.0182441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fagan A.A., Catalano R.F. What works in youth violence prevention: a review of the literature. Res Soc Work Pract. 2013;23(2):141–156. [Google Scholar]