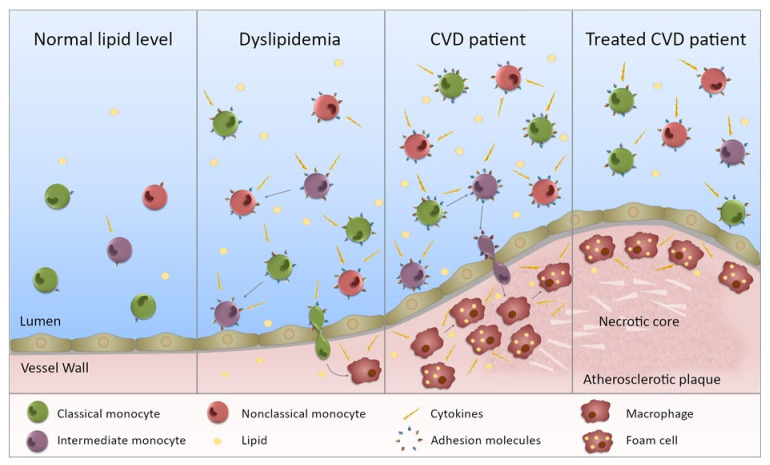
Figure 2.
Monocytes in dyslipidemia and CVD. This figure illustrates the state of monocytes in CVD. Normal lipid levels: in individuals with normal lipid levels, inflammation is low and the different monocyte subsets preferentially express specific adhesion molecules and chemokine receptors. Dyslipidemia: in individuals with dyslipidemia, the monocyte subset proportion is altered with increased intermediate and nonclassical monocytes, presumably through maturation of monocytes from one subset to the next. In addition, all subsets are more inflammatory (not just one) with increased ability to produce inflammatory cytokines. The subsets also express an increased level, and range of, adhesion molecules (and chemokine receptors) giving them a greater potential to bind to the endothelium. Entering the vessel wall, they become macrophages and upon lipid uptake, transform into foam cells. CVD patient: in CVD patients, the inflammatory state of the monocytes is further exacerbated and subset proportions further perturbed. Monocytes are more able to enter the vessel wall and to adopt an inflammatory macrophage phenotype once there. The chronic inflammatory state will contribute to plaque development. Treated CVD patient: upon treatment, the monocyte subsets become less inflammatory, but they do not necessarily return to levels equivalent to controls. Any lipid-associated functional changes of monocyte derived macrophages in the atherosclerotic plaque that have been induced by trained immunity may persist. Thus, plaque progression could continue despite a drop in lipid levels.