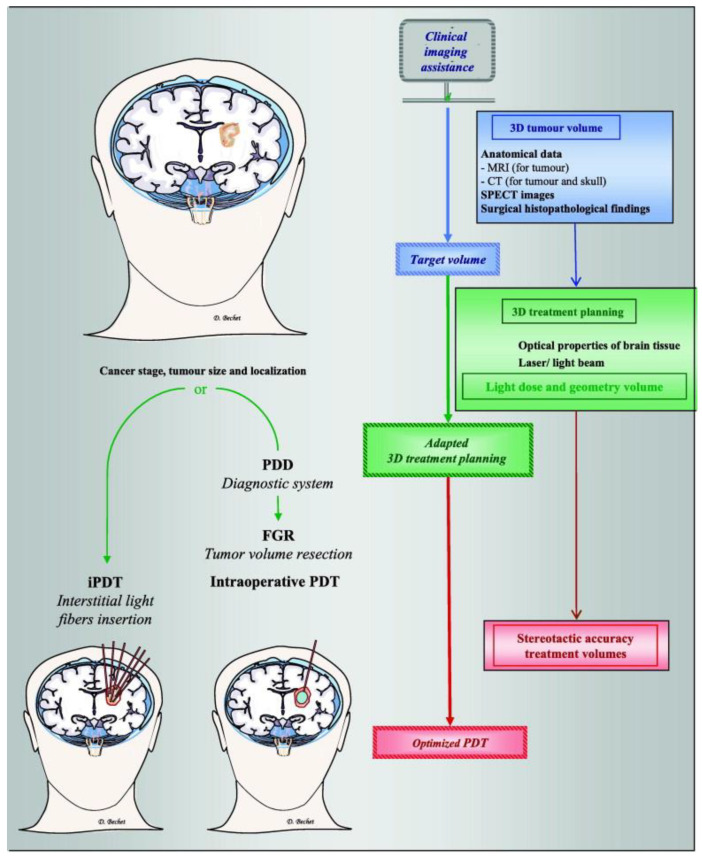
Figure 3.
Clinical imaging assistance as an essential step in therapeutic planning. Left side: Two strategies suggested depending on the stage, size, and localization of the tumour. An interstitial PDT (iPDT) or, after a minimally invasive craniotomy, a photodiagnosis (PD) followed by a fluorescence-guided resection (FGR) and completed by an intraoperative PDT. Right side: Clinical imaging assistance plays an essential role in brain tumour PDT, including estimating the initial tumour volume, 3D treatment planning (light dose according to the volume geometry), and outcome assessment. Computed 3D image-based treatment planning provided reproducible data-based tumour volumes, stereotactic accuracy for tumour volume resection, and interstitial light fibre insertion for iPDT. Optical fibres for PDT can be placed under contrast-enhanced computed tomography (CT) guidance, and the surgical approach and trajectories can be planned using preoperative diffusion magnetic resonance imaging (MRI), CT imaging, and/or single-photon emission computed tomography (SPECT) images to achieve precise tumour localization, realize a minimally invasive craniotomy, and minimize controlateral brain injury. Reproduced with permission from D. Bechet, Cancer Treat. Rev. 2014 [88].