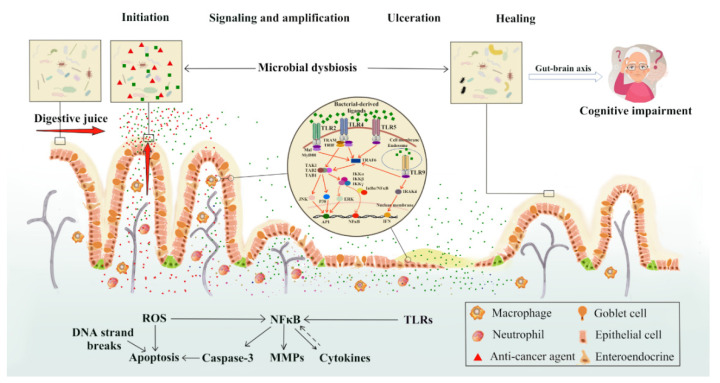
Figure 1.
New perspectives on impacts of chemotherapy-induced intestinal microbial dysbiosis on pathogenesis of mucositis and the non-intestinal manifestations of mucositis. On the basis of the five-phase model for chemotherapy-induced mucositis put forward by Sonis in 2004, this review proposed the possible roles of intestinal microbial dysbiosis at various phases of mucositis pathogenesis and in the cognitive impairment of patients/survivors. Chemotherapy drugs or their metabolites may percolate into intestinal mucosa and may also be secreted along with various digestive fluids, directly destroying the bacteria in the gut lumen, altering their total numbers and compositions. Cell wall components of the killed bacteria are recognized by toll-like receptors (TLRs), such as peptidoglycan through TLR-2, lipopolysaccharide (LPS) through TLR-4, flagelin through TLR-5 and non-methylated DNA (CpG DNA) through TLR-9. All TLRs recruit adaptor proteins via the myeloid differentiation factor 88 (MyD88)-dependent pathway and/or adaptor-inducing interferon-β (TRIF)-dependent pathway to activate NF-κB and/or ERK/JNK/p38 kinases, which further lead to increased expression of inflammatory mediators. Intestinal microbial dysbiosis may further affect the mental health of patients/survivors through the microbiota-gut-brain axis. MAL: MyD88-adaptor like protein; IRAK: interleukin-1 receptor associated kinase; TRAF6: TNF-α receptor association factor 6; TAK: thylakoid associated kinase; TAB: TAK-binding protein; NF-κB: nuclear factor-κB; IκB: NF-κB inhibitor; IKK: IκB kinase; ERK: extracellular signal-regulated kinase; JNK: c-Jun N-terminal kinase; AP-1: activator protein 1; IFN: interferon.