Abstract
Objective
To evaluate sleep characteristics of parents and their children during the COVID-19 pandemic and predictors for sleep disturbances.
Methods
Cross-sectional web-based study using an online survey made available for dyads of parents and their children during the 7th week of quarantine in southern Brazil. Parents' and adolescents’ sleep were characterized using the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale. For children aged 0-3 years parents completed the Brief Infant Sleep Questionnaire, for those aged 4-12 years the Sleep Disturbance Scale for Children. Parents also informed, subjectively, their perception about sleep habits during social distancing. Multiple regression was run to predict sleep disturbances in adults using independent variables: sex, income, education, children age, and children with sleep disturbances.
Results
Data from 577 dyads showed sleep alterations in 69,8% of adults, in 58,6% of children aged 0-3 years, 33,9% in the 4-12 years range (with a predominance of disorders of initiating or maintaining sleep), and 56,6% in adolescents. Sex (female) and children with sleep disturbances were significant predictors of a sleep problem in parents (p < 0.005). Subjective perception revealed complaints related to emotional concerns such as anxiety and fear in adults and due to alterations in routine in children and adolescents.
Conclusion
The present study's data showed an increased rate of sleep problems among families during quarantine both measured by validated instruments and also based on personal perception.
Keywords: COVID 19, Sleep, Children, Adolescents, Social isolation
Introduction
At the end of December 2019, a series of pneumonia cases with unknown etiology affected 41 patients in the city of Wuhan, China.1 Quickly, it was discovered that the cause was the contamination by a new type of coronavirus called COVID-19. Based on the rapid increase in the number of infections WHO declared the outbreak of COVID-19 as a pandemic.2
To reduce transmission, classical public health measures to contain the advance in the number of contaminations were applied, and to prevent the spread of the virus from person to person social isolation was adopted.3 Based on the increased number of cases and the rapid transmission among the population, the government adopted a ‘stay-at-home’ order, closing all schools, universities, and non-essential activities since March, 16th, 2020. This order forced several drastic lifestyle changes such as remote working and home-schooling. In addition, the imposed social distancing and a lack of social interaction caused by stay-at-home order, together with the separations of loved ones, loss of freedom of movement, uncertainty, and fear about the disease were associated with behavioral and psychological consequences.4
Prolonged home confinement affects physical and mental health with families being forced to promote sudden alterations in daily-life activities, together with reduced levels of physical activity, altered pattern of food consumption, and consequently weight gain.5 In addition, the uncertainty about the future, with financial and health concerns promotes a very stressful situation that could likely impact sleep habits. Sleep is an essentially biological process for life and health and plays an important role in the regulation of brain function, metabolism, immune system, hormonal secretion, and cardiovascular system.6
All of a sudden, children and adolescents were challenged by substantial lifestyle changes that include online lessons and altered routine habits. Also, home confinement reduced substantially social interaction and outdoor activities, resulting in increased screen time.7 Previous studies already showed that home confinement during the COVID-19 outbreak promoted altered sleep habits, resulting in sleep disturbances in both children and adolescents. An Italian survey with 4312 subjects showed that younger children had an increased prevalence of difficulty falling asleep and night awakenings.8 Also, another European survey showed acute worsening in the sleep of babies and children 0-6 years old.9 To date, a big Brazilian online survey was previously published with 45,161 adults and assessed sleep quality in the population, describing a 44.9% increase in sleep problems during the COVID-19 outbreak.10 Data regarding sleep quality in children and adolescents in Brazil are lacking. It is reasonable to hypothesize that the ‘stay-at-home’ order could impact the sleep quality of families living together in a regimen 24/7, without regular routines due to work or school duties. Chronic sleep disturbances might have an impact on public health, considering that individuals exposed to sleep disorders can have several changes in behavior and peripheral signaling systems.6
Considering that sleep quality is closely linked to overall health, it is important to investigate the impact of social distancing measures on the sleep characteristics of the population. Thus, this study aimed to investigate sleep characteristics of dyads (parents and their children) as well as predictors for poor sleep quality during social distancing caused by the COVID-19 pandemic.
Methods
This is a cross-sectional web-based study. Data were collected using an online survey (Qualtrics® online survey software (www.qualtrics.com) during the “stay-at-home” order. Participants were invited through social media (Instagram, Facebook, and Whatsapp advertisements) and via the internet, radio, and TV calls between the 27th of April, and the 30th of July 2020). The present study was approved by the institutional Ethical Committee and is registered on Plataforma Brasil under the number 30748320.5.0000.5336. Consent was obtained via a consent form found at the start of the online questionnaire and respondents were only able to proceed with the survey if they clicked on “I agree to participate in this study”. This survey was designed for parents and their children but the authors cannot completely rule out the possibility of an under-age to access the survey and take part without their parent's approval. Unfortunately, this is a common issue that applies in online, web-based surveys. However, the authors took great care to make sure that the survey did not include any question that would elicit a negative influence or represent any risk.
Parents were asked to provide sociodemographic data and directed to complete the “Pittsburgh Sleep Quality Index” and the “Epworth Sleepiness Scale”. The educational level and income were evaluated and ranked following Brazilian Statistics Institute, a public institution responsible for collect and publish all the geographical data in Brazil. Afterward, were asked to answer if, during home confinement caused by COVID-19, their sleep changed, with the following options: 1) Improved; 2) Worsened; 3) Not changed/Don't know. To qualitatively evaluate the participant's perception regarding the reason for such a change, the following open question was made: “If you have experienced any changes, describe in a short sentence what you believe is the reason”. Upon completing the first section, adults were asked whether or not they have kids living together and then directed to the appropriate instruments. For analysis, the authors have included only questionnaires with full answers completed.
For adults, the Brazilian version of the “Pittsburgh Sleep Quality Index (PSQI)”, was applied.11 A global score of equal or greater than five distinguishes poor and good sleepers. In addition, the Brazilian version of the “Epworth Sleepiness Scale”, a 6-item survey where the participants score, in a 0-3 Likert Scale the probability of nap or fall asleep in daily-life activities was also applied. From a total of 24 points, a score >10 indicates mild or excessive daytime sleepiness.12
For children aged 0 to 3 years and 11 months, parents were asked to respond to the “Brief Infant Sleep Questionnaire (BISQ),13 for children aged 4 to 12 years and 11 months, parents were asked to respond to the Brazilian version of the “Sleep Disturbance Scale for Children (SDSC)14 and for adolescents (under 18 years old) it was also used the PSQI. To calculate sleep disturbances rates, the authors used previously standardized cut-off scores for each of the previously mentioned instruments. For BISQ, the cut-off score was one (or more) of the following: more than 3 nocturnal awakenings, nocturnal wakefulness greater than 1h, and/or total sleep time lower than 9 hours.13 For SDSC scores were calculated as follow: Disorders of initiating and maintaining sleep (sum of items 1, 2, 3, 4, 5, 10, and 11, cut-off ≥ 17 points); Sleep breathing disorders (sum of items 13, 14, and 15, cut-off ≥ 7 points; Disorders of arousal (sum of items 17, 20 and 21, cut-off ≥ 6 points); Sleep-wake transition disorders (sum of items 6, 7, 8, 12, 18 and 19, cut-off ≥ 14 points); Excessive daytime sleepiness (sum of items 22, 23, 24, 25 and 26, cut-off ≥ 13 points); Sleep hyperhidrosis (sum of items 9 and 16, cut-off ≥ 7 points). A cut-off score ≥ 52 points were used regarding the total score. For adolescents, the PSQI cut-off score ≥ 5 points were used.11
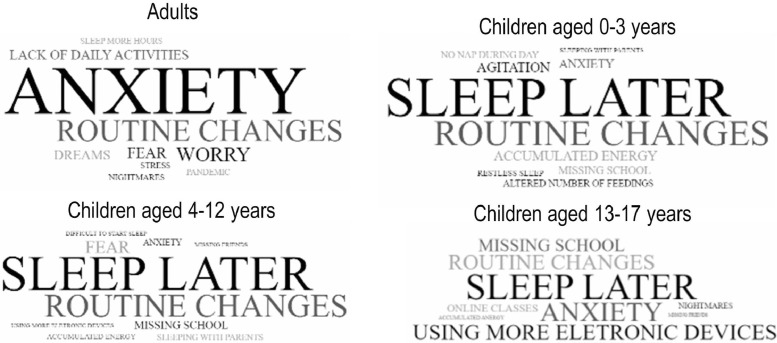
Tag clouds are a text-based visual depiction of words used to display the relative word frequency, popularity or importance by font size and tag clouds can also serve as a summary of the content. To create the tag clouds, data derived from the open question “If you have experienced any changes, describe in a short sentence what you believe is the reason” was organized and the most cited terms were sorted and selected for visual depiction.
Considering that Brazil has continental proportions and public policies to contain COVID-19 spread were heterogeneous, for this study the authors have included only responders that live in southern Brazil, at the Rio Grande do Sul state, during the period between April 27th and May 6th (7th week of quarantine) because there was a homogeneous control of social distancing policies established based on colored flags and all the region was under red flag alert system.
Data analysis
The primary objective of this study was to analyze the sleep quality of both parents and their children during COVID-19 lockdown. The authors further choose to analyze possible predictors of sleep disturbances of parents such as sex, income, education, children's age, and children with sleep disturbances. Finally, exploratory analysis of sleep scores between subjects that have children compared to subjects with no children.
Data were analyzed using the software SPSS, version 20.0. Mean value, standard deviation, and frequency was calculated, as well as the difference between groups, using t test and chi-square test. A student's t test was used to compared PSQI global between parents with kids and parents with no kids. In addition, the authors used a one-way ANOVA to analyze the differences between groups in the PSQI sub scores and global scores using the overall subjective perception of sleep quality (improved, worsened, and no change/don't know as an independent variable. The authors also analyzed PSQI sub scores and global scores using the child's age as an independent variable (0-3 years old, 4-12 years old and adolescents). For all one-way ANOVA, a Bonferroni multiple comparisons were used to detect between groups' differences.
A multiple regression model was adopted with PSQI scores as a dependent variable and the following independent variables (predictor): sex, income, education, children's age, and children with sleep disturbances. All analyses were two-tailed and the significance level was set at p < 0.05.
This sample size was calculated using the Brazilian population (22 million) with an error of 2% and significance of 5%, leading to a sample size of 2401 respondents. From there, the authors selected a sub-sample of respondents that reported having children and compared it to a random sample of respondents that reported not having children.
Results
Sleep characteristics among parents and their children
A total of 2484 adults completed the online survey to investigate sleep quality in the Brazilian population during the COVID-19 pandemic (unpublished data). From these, 577 participants completed the survey during the 7th week of quarantine, living in the Rio Grande do Sul state and reported having children under 18 years old (173 from 0-3 years; 254 aged 4-12 years and 150 aged 13-17 years old). Sex distribution showed an increased percentage of women (81,7%) as respondents. The distribution of the adult sample regarding income and education level is presented in Table 1. The authors found a significant amount of respondents with poor sleep quality with education level “with some college, no degree” (X² = 14,484, p < 0,001) and “advanced degree” (X² = 15,382, p < 0.001).
Table 1.
General characteristics of the adult sample (n = 577).
| Variable | PSQI Score |
Statistics | p | |
|---|---|---|---|---|
| Normal Global Score <5 n = 172 |
Poor Sleep Quality Global Score ≥ 5 n = 405 |
|||
| Age | 38,60±7,23 | 38,04±6,45 | t(576) = 0,191 | ,540 |
| Sex (male/female) | 38/134 | 70/335 | X² = 1,386 | 0,268 |
| Education | ||||
| High School or less | 20 | 48 | X² = 0,729 | 0,393 |
| Some college, no degree | 8 | 29 | X² = 14,484 | <0,001 |
| Bachelor's degree | 47 | 106 | X² = 0,006 | ,940 |
| Advanced degree | 97 | 228 | X² = 15,382 | <0,001 |
| Socioeconomic Status | ||||
| Lower | 6 | 7 | X² = 1,203 | ,273 |
| Lower middle | 11 | 33 | X² = 6,148 | ,013 |
| Middle | 73 | 173 | X² = 0,001 | ,981 |
| Upper high | 20 | 64 | X² = 1,645 | ,200 |
| High | 62 | 130 | X² = 4,992 | ,025 |
Age (continuous variable) was compared using a student's t test. Sex, Education and Socioeconomic Status were compared using chi-squared test. Significance was defined was p < 0.05.
Table 2 presents the general sleep characteristics of the sample. In parents, 405 (70,1%) had PSQI scores that indicate poor sleep quality. Among PSQI domains, 78,6% had poor sleep latency and 31,5% had poor sleep efficiency. Poor sleep duration was observed in 42,9%. For children aged 0-3 years, 126 (58,6%) have abnormal BISQ scores and among children, 4-12 years old, 99 (33,9%) children have scores that indicate disorders of initiating and maintaining sleep, and 54 (18,5%) children presented sleep-wake transition disorders. For adolescents, 85 (56,6%) had poor sleep quality (PSQI global score ≥ 5).
Table 2.
Sleep characteristics from adults and children.
| Variable | N (%) |
|---|---|
| Adults (n = 577) | |
| Poor Sleep Quality (PSQI global score ≥ 5) | 405 (70,1%) |
| Poor sleep quality | 86 (14,9%) |
| Poor sleep latency | 454 (78,6%) |
| Poor sleep duration | 248 (42,9%) |
| Poor sleep efficiency | 182 (31,5%) |
| Difficulty falling asleep | 398 (68,9%) |
| Use of sleeping medication | 76 (13,1%) |
| Daytime dysfunction | 340 (58,9%) |
| Abnormal ESS | |
| Mild or excessive daytime sleepiness | 14 (2,4%) |
| 0-3 years (n = 215) | |
| Abnormal BISQ | 126 (58,6%) |
| More than 3 nocturnal awakenings | 50 (23,1%) |
| Nocturnal wakefulness | 85 (39,4%) |
| Total sleep time <9h | 66 (30,7%) |
| 4-12 years (n = 292) | |
| Abnormal SDSC | 81 (27,7%) |
| Disorders of initiating and maintaining sleep | 99 (33,9%) |
| Sleep breathing disorders | 15 (5,1%) |
| Disorders of arousal | 27 (9,2%) |
| Sleep-wake transition disorders | 54 (18,5%) |
| Excessive daytime sleepiness | 29 (9,9%) |
| Sleep hyperhidrosis | 30 (10,3%) |
| 13-17 years (n = 150) | |
| Poor Sleep Quality (PSQI global score ≥ 5) | 85 (56,6%) |
BISQ, Brief Infant Sleep Questionnaire; ESS, Epworth Sleepiness Scale; PSQI, Pittsburgh Sleep Quality Index; SDSC, Sleep Disturbance Scale for Children.
Sleep quality auto perception and PSQI scores in parents
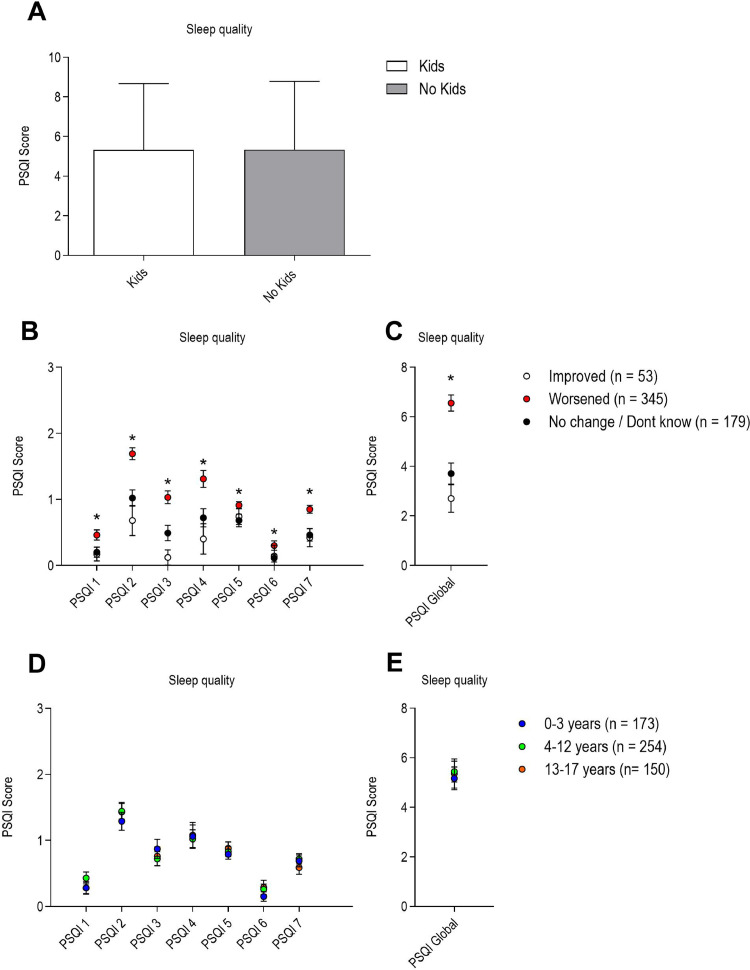
A student t-test showed that PSQI scores between parents and adults without kids did not differ significantly. It is important to note that both groups score higher than 5, which indicates poor sleep quality (Fig. 1A).
Figure 1.
A) Sleep quality comparison between parents and adults without kids showed no significant difference between groups [t(1152) = 0.050, p = 0.96]. B) Sleep perception (number of people self-reporting an improvement, worsening or no changes/Don't know in sleep quality) and PSQI scores. PSQI domains comparison among groups using one-way ANOVA. PSQI-1, Subjective sleep quality: [F(2, 575) = 14.746, p < 0.001). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p = 0.003, mean difference: -0.23, CI: -0.39 to -0.06); PSQI-2, Sleep latency [F(2, 575) = 24.121, p < 0.001). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p < 0.001, mean difference: -1.00, CI: -1.41 to -0.59); PSQI-3, Sleep duration [F(2, 575) = 18.404, p < 0.001). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p < 0.001, mean difference: -0.93, CI: -1.36 to -0.51); PSQI-4, Sleep efficiency [F(2, 575) = 18.150, p < 0.001). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p < 0.001, mean difference: -0.91, CI: -1.46 to -0.37); PSQI-5, Difficulty falling asleep [F(2, 575) = 2.438, p < 0.001). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p < 0.001, mean difference: -0.11, CI: -0.33 to -0.09); PSQI-6, Use of sleeping medication [F(2, 575) = 1.253, p = 0.01). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p < 0.001, mean difference: -0.19, CI: -0.44 to -0.06); PSQI-7, Daytime dysfunction [F(2, 575) = 7.448, p < 0.001). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p < 0.001, mean difference: -0.45, CI: -0.71 to -0.18); D) PSQI-Global: [F(2, 575) = 390.538, p < 0.001). Bonferroni post hoc test revealed statistically significant difference between worsened and improved (p < 0.001, mean difference: -3.84, CI: -5.11 to -2.58); C) Sleep quality comparison (PSQI scores) between parents with kids from different age groups. PSQI domains comparison between groups using one-way ANOVA revealed no significant differences between groups; PSQI-1, Subjective sleep quality: [F(2, 575) = 2.350, p = 0.097); PSQI-2, Sleep latency [F(2, 575) = 0.952, p = 0.387); PSQI-3, Sleep duration [F(2, 575) = 1.088, p = 0.338); PSQI-4, Sleep efficiency [F(2, 575) = 0.075, p = 0.928); PSQI-5, Difficulty falling asleep [F(2, 575) = 0.475, p = 0.622); PSQI-6, Use of sleeping medication [F(2, 575) = 1.585, p = 0.206); PSQI-7, Daytime dysfunction [F(2, 575) = 1.092, p = 0.337); E) PSQI-Global: [F(2, 575) = 0.238, p = 0.789). * Represents p < 0.05.
To analyze the agreement between subjective perception of overall sleep quality during the COVID-19 pandemic and the scores of PSQI, the authors conducted a one-way ANOVA that showed a statistically significant difference in all PSQI subscores between parents who perceived an improvement in sleep quality when compared to parents who perceive a worsening in sleep quality during home confinement (Fig. 1B).
Later, the authors also compared the PSQI score of parents based on the children's age, to investigate if parents who have babies, younger children, or adolescents present differences across PSQI sub scores. The authors found no statistically significant differences between groups, suggesting that the child's age does not alter the parents’ PSQI sub-scores (Fig. 1C).
Predictors of sleep disturbances during home confinement
Another goal of this study was to test which variables could be associated with the sleep disturbances of parents during home confinement. Thus, a multiple regression was run to predict sleep disturbances in adults from sex, income, education, children's age, and children with sleep disturbances. A significant regression equation was found F(5,576) = 2,681, p < 0.05. In the present study's model, sex (female) and children with sleep disturbances were significant predictors of a sleep problem in parents (Table 3).
Table 3.
The results of multiple regression analysis of sleep disturbances in adulthood. Dependent variable: Abnormal PSQI (score ≥ 5).
| Unstandardized coefficient | Standardized coefficient | t | p value | ||
|---|---|---|---|---|---|
| Variable | B | Std Error | Beta | ||
| (constant) | 0,496 | 0,153 | 3,248 | 0,001 | |
| Sex | -0,143 | 0,052 | 0,121 | 2,337 | 0,020a |
| Income | ,0121 | 0,038 | -0,031 | -0,599 | 0,550 |
| Education | 0,031 | 0,027 | -0,092 | -1,546 | 0,123 |
| Children Age | -0,022 | 0,020 | 0,093 | 1,533 | 0,119 |
| Children w/ Sleep Disturbances | -0,042 | 0,067 | -0,112 | -2,149 | 0,032a |
Indicate statistical significance at 5% level.
Qualitative aspects of sleep during home confinement
Finally, to analyze the qualitative data, the authors selected the 10 most cited terms in the opened questions to be visually depicted in Supplementary Material - Fig. S1. Among adults, the word “Anxiety” appeared 169 times, followed by “Routine changes” (76), “Worry” (51), “Fear” (40), “Lack of daily activities” (36), “Dreams” (35), “Pandemic” (21), “Sleep more hours” (20), “Stress” (19) and “Tiredness” (18). Among children aged 0-3 years, the 10-most cited terms that appeared were “Sleep Later” (52), “Routine Changes” (34), “Accumulated energy” (11), “Agitation” (11), “Anxiety” (10), “Missing school” (9), “No nap during the day” (7) and “altered number of feeding” (7). For children 4-12 years old, the terms were “Sleep later” (52), “Routine changes” (38), “Fear” (21), “Missing school” (13), “Anxiety” (11), “Sleeping with parents” (11), “Accumulated Energy” (9), “Using more electronic device” (8), “Missing friends” (7) and “Difficulty to start sleep” (7). For adolescents, the 10-most cited terms were “Sleep Later” (23), “Anxiety” (17), “Routine changes” (13), “Using more electronic device” (13), “Missing School” (10), “Online classes” (6), “Lack of physical activity” (4), “Nightmares” (4) and “Accumulated energy” (2) (Fig. 2).
Figure 2.
Tag-cloud with 10-most cited terms regarding participant's reason for altered sleep habits.
Discussion
The study showed that almost 70% of the present study's adult sample have poor sleep quality, with higher sleep latency (amount of time it takes to fall asleep) and poor efficiency (amount of time a person sleeps in relation to the amount of time spent in bed). For children aged 4-12 years the main problem was initiating and/or maintaining sleep, and for the 0-3 years group increased nocturnal awakenings. The authors have also found that sex and having a child with sleep disturbances significantly predicted parents' sleep problems.
Different from previous studies that addressed sleep in adult samples of health workers, much more exposed to stressful situations, or adults with other comorbidities such as mental disorders or obstructive sleep apnea,15, 16, 17 this study focused on families from a general population at a time-limited period of quarantine. Further, no previous studies have associated parents and their children's sleep habits during the lockdown. Although the present study's data do not allow a direct cause-effect association of stay-at-home order and an increased rate of poor sleep quality in adults, the authors can hypothesize that the stressful context of pandemic confinement is leading to alterations in sleep quality. It was already been shown that other stressful contexts such as work overload and occupational stress were positively associated with the frequency of poor sleep quality. In addition, a recent report by Coiro et al (2021) found higher rates of depression and anxiety, as well as poor sleep quality in the United States and Israel respondents.18
The percentage of altered sleep observed in the adult population analyzed in this study was superior to what was reported in similar ones developed in Greece (sleep problems were detected in 37.6%) and the USA (25%).19,20 The Italian study showed an increase in sleep disorders from 40.5% previous to lockdown to 52.4% in the second week of isolation, but the population studied had also a high incidence of behavioral and mood disorders.21 However, those studies analyzed data collected around the second week of lockdown. The present study's increased rates might be explained by the timing of the questionnaire, during the 7th week of quarantine, and by the feeling of elongation of time in a longer period of isolation.
Interestingly, the most cited word among parents in the open question was “Anxiety”. The relationship between anxiety and sleep problems is known for a long time.15 It is hard to distinguish if people are anxious and therefore, they have trouble sleeping or sleeping problems that make people anxious. Nevertheless, anxiety and sleep are strictly related and affect which other in a two-way manner. Recent studies during the COVID 19 pandemic showed this association in different sectors and populations.15,16,20, 21, 22, 23 In addition, it is important to note that a quarter of this study's sample reported the use of medication to sleep once or twice a week (PSQI item 7) which could be related to increased latency to sleep and anxiety.
Data regarding children also showed the impact of isolation on sleep. Approximately one-third of the 4-12 years group had scores that indicate potential disorders of initiating and maintaining sleep. In addition, routine changes were frequently reported by participants as a factor that could contribute to altered sleep. According to previous work from the present study's group, a population-based study that evaluated sleep in Brazilian children and adolescents,24 the overall prevalence of sleep disturbance was 25.5%, using the same instruments according to age groups (0-3 years: BISQ, 4-12 SDSC and PSQI for adolescents). Also, the prevalence of sleep problems among children aged 0-3 years (58.6%) found in this study was a striking difference, when compared to the previous (20%) with a very similar methodological approach (online-based survey with same instruments). Overall, in a very narrow window of time, the authors found an increase in the prevalence of sleep disturbances in children, and this might be due to the changing of habits during quarantine. Although there is not yet much data available regarding the effects of the COVID quarantine on sleep in children, in a national survey developed in Canada, 1/3 of the families were not following the recommendations for sleep hygiene and a significant decrease in physical activity was also observed.25 These findings might have important public health implications as in a recent study published by Morales-Muñoz and collaborators,26 it was observed that some behavioral sleep problems early in childhood are associated with psychosis and borderline personality disorder in adolescence. Further, depression at 10 years of age was associated with frequent night awakenings at 18 months of age and irregular sleep routines at 5.8 years of age.27 Additionally, another recent paper that investigated psychological symptoms, non-suicidal self-injury, and suicidal (ideation, plans, and attempts) among a cohort of Chinese children and adolescents before the outbreak of COVID and 3 months later, after school reopening, demonstrated a significant increase in the rates of mental health problems.25
Although the authors have not longitudinally followed this cohort, a limitation of this study, the present study's data showed an impressive rate of poor sleep quality, during a period with a homogeneous regulation of social restrictions. Another limitation of this study is a high prevalence of higher educated respondents, which could impair the generalization of these findings to lower educated populations, considering that the COVID-19 pandemic could have a different impact on people from different socioeconomic statuses. In addition, the authors configure the survey to allow adults to respond regarding only one child and the authors cannot control or ensure what was the criteria for parents to choose from which kids they were responding (the younger, the worst sleeper, etc).
In conclusion, the authors have observed a great overall perception of worsening in sleep quality during stay-at-home orders either in adults and children in southern Brazil. The more frequent complaints about irregular sleep in parents were emotional concerns such as anxiety and fear and alterations in routine and sleep habits for children.
Funding
Magda Lahorgue Nunes MD, PhD is a researcher 1D supported by CNPq-Brazil, PQ grant number 306338/2017-3.
Luis Eduardo Wearick-Silva PhD and Samanta Andresa Richter MsC - This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nivel superior – Brazil (CAPES) – Finance Code 001.
COVID 19-Sleep Research Group (Misses Nathália Fornari Fernandes, Melissa Rogick Guzzi Taurisano, Nathália Fritsch Camargo and Luísa Basso Schilling receive scholarship from our institutional Junior Research Fellow Program the BPA- PUCRS).
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jped.2021.07.002.
Appendix. Supplementary materials
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou T, Liu Q, Yang Z, Liao J, Yang K, Bai W, et al. Preliminary prediction of the basic reproduction number of the Wuhan novel coronavirus 2019-nCoV. J Evid Based Med. 2020;13:3–7. doi: 10.1111/jebm.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27:taaa020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . World Heal Organ; 2020. Mental health and psychosocial considerations during COVID-19 outbreak. [Google Scholar]
- 6.Al Dabal L, Bahammam AS. Metabolic, endocrine, and immune consequences of sleep deprivation. Open Respir Med J. 2011;5:31–43. doi: 10.2174/1874306401105010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt SCE, Anedda B, Burchartz A, Eichsteller A, Kolb S, Nigg C, et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. 2020;10:21780. doi: 10.1038/s41598-020-78438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oliviero B, Emanuela M, Mattia D, Elena F, Karen S, Grazia MM, et al. Changes In sleep patterns and disturbances in children and adolescents in Italy during the Covid-19 outbreak. Sleep Med. 2021;S1389-9457(21):00094-0. [DOI] [PMC free article] [PubMed]
- 9.Markovic A, Mühlematter C, Beaugrand M, Camos V, Kurth S. Severe effects of the COVID-19 confinement on young children's sleep: a longitudinal study identifying risk and protective factors. J Sleep Res. 2021:e13314. doi: 10.1111/jsr.13314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lima MG, Malta DC, Werneck AO, Szwarcwald CL, Souza DB, Gomes CS, et al. Effect of chronic non-communicable diseases (CNCDs) on the sleep of Brazilians during the COVID-19 pandemic. Sleep Med. 2021;S1389-9457(21):00155-6. [DOI] [PMC free article] [PubMed]
- 11.Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, da Silva Miozzo IC, de Barba ME, et al. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med. 2011;12:70–75. doi: 10.1016/j.sleep.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Bertolazi AN, Fagondes SC, Hoff LS, VD Pedro, Barreto SSM, Johns MW. Portuguese-language version of the Epworth sleepiness scale: validation for use in Brazil. J Bras Pneumol. 2009;35:877–883. doi: 10.1590/s1806-37132009000900009. [DOI] [PubMed] [Google Scholar]
- 13.Nunes ML, Kampff J de la PR, Sadeh A. BISQ questionnaire for infant sleep assessment: translation into Brazilian Portuguese. Sleep Sci. 2012;5:89–91. [Google Scholar]
- 14.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113:e570–e577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 15.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine (Baltimore) 2020;99:e20769. doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu CH, Stevens C, Conrad RC, Hahm HC. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among U.S. young adults with suspected and reported psychiatric diagnoses. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coiro MJ, Asraf K, Tzischinsky O, Hadar-Shoval D, Tannous-Haddad L, Wolfson AR. Sleep quality and COVID-19-related stress in relation to mental health symptoms among Israeli and U.S. adults. Sleep Heal. 2021;7:127–133. doi: 10.1016/j.sleh.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Batool-Anwar S, Omobomi OS, Quan SF. Impact of the novel coronavirus disease on treatment adherence and sleep duration in patients with obstructive sleep apnea treated with positive airway pressure. J Clin Sleep Med. 2020;16:1917–1920. doi: 10.5664/jcsm.8746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gao C, Scullin MK. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020;73:1–10. doi: 10.1016/j.sleep.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29:e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 24.de Almeida GM, Nunes ML. Sleep characteristics in Brazilian children and adolescents: a population-based study. Sleep Med X. 2019;1 doi: 10.1016/j.sleepx.2019.100007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17:85. doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morales-Muñoz I, Broome MR, Marwaha S. Association of parent-reported sleep problems in early childhood with psychotic and borderline personality disorder symptoms in adolescence. JAMA Psychiatry. 2020;77:1256–1265. doi: 10.1001/jamapsychiatry.2020.1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang L, Zhang D, Fang J, Wan Y, Tao F, Sun Y. Assessment of mental health of Chinese primary school students before and after school closing and opening during the COVID-19 Pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21482. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.