ABSTRACT
Objective: The Theory of Planned Behavior (TPB) is one of the most robust models in explaining health-related behavior. In this study, we tested the extended TPB to predict university students’ intentions to uptake COVID-19 vaccination.
Methods: An online cross-sectional survey was developed to investigate students’ intention to uptake the COVID-19 vaccine based on the components of the TPB (i.e., attitude, subjective norms, and perceived behavioral control) and extended components (i.e., knowledge about COVID-19, risk perception of COVID-19, and past influenza vaccination behavior). Non-probability sampling was used to collect data from 3145 students from 43 universities in mainland China in January 2021. Structural equation modeling (SEM) was applied to examine the proposed model. Enrolled students were relatively young (mean age = 20.80 years; SD = 2.09), half of them are female (50.2%), and most of them were studying in undergraduate programs (n = 3026; 96.2%).
Results: The results showed that students’ knowledge of the COVID-19 vaccine and risk perception of COVID-19 positively influenced their attitude toward the uptake of a COVID-19 vaccine. Also, students’ attitude toward COVID-19 vaccination uptake and their past influenza vaccination uptake behaviors were positively associated with the intention to uptake COVID-19 vaccination. Subjective norm and perceived behavioral control were not significant predictors for the intention to uptake COVID-19 vaccination (R2 = 0.49).
Conclusions: The present study demonstrated that the extended TPB appears to be an efficient model with the focus on attitude, knowledge, risk perception, and past influenza vaccination uptake behaviors in explaining students’ intention for COVID-19 vaccination.
KEYWORDS: COVID-19, risk perception, theory of planned behavior, university students, vaccination uptake
The coronavirus disease 2019 (COVID-19) pandemic has deeply impacted multiple aspects of human lives since the end of 2019, including physical and mental health, social interactions, economy, education, and occupations.1–6 Vaccination against the virus has become the most important measure in tackling COVID-19 as most countries worldwide continue to struggle to control the spread of the virus. The development of COVID-19 vaccines worldwide has been accelerated in response to the urgent need to control the spread of the virus, and more than 60 candidate vaccines are under clinical evaluation.7 However, research has demonstrated that significant minority of individuals worldwide are still hesitant about the COVID-19 vaccine injection.8–15 Consequently, hesitancy and resistance to uptake vaccination may hamper the effectiveness of controlling the spread of the virus.16 Therefore, it is important to understand the factors predicting individuals’ intention to uptake COVID-19 vaccination.
Applying theory to real life practical situations is beneficial because theories provide a comprehensive consideration of behavior changes concerning critical factors.17 For example, the Theory of Planned Behavior (TPB) can be used as a practical framework to understand important factors for intention to uptake COVID-19 vaccination. Research has applied the TPB to analyze individuals’ attitudes toward (and uptake of) vaccination such as influenza18,19 and human papillomavirus (HPV).20 Therefore, the TPB may also work for COVID-19 vaccination uptake. Indeed, a meta-analysis of TPB studies showed that attitudes, subjective norm, and perceived behavioral control accounted for 39% variance in intentions to uptake vaccination in a previous study.21 According to the TPB,22 three core components, comprising attitude, subjective norm, and perceived behavioral control, together shape an individual’s intentions to uptake vaccination. Individuals’ attitudes toward a behavior refers to the degree to which an individual has a favorable or unfavorable evaluation toward a specific behavior.23 Perceived subjective norm regarding behavior refers to individuals’ perceptions of judgment from significant others (e.g., friends, family, and society members more generally) in engaging in a specific behavior.24 Perceived behavioral control refers to the confidence toward the likelihood of successfully engaging in a specific behavior.24
Based on the efficiency in explaining vaccination uptake for influenza and HIV, the TPB has been successfully used for predicting intentions to uptake COVID-19 vaccination.25 A recent study demonstrated that individuals who had a more positive attitude toward vaccination uptake, scored higher on subjective norms and self-efficacy had higher willingness to uptake vaccination against COVID-19.26 Another study showed that parents’ positive attitudes, perceived family members’ supporting COVID-19 vaccination for children, and perceived behavioral control of having the children uptake COVID-19 vaccination were associated with higher parental acceptability of COVID-19 vaccination for children.27 However, more evidence is needed to better understand how the TPB can be used to inform our understanding of the intention to uptake COVID-19 vaccination based on the following reasons.
First, COVID-19, a novel infectious disease, can cause death within a relatively short period among individuals in high-risk groups. Therefore, the vaccines for COVID-19 have been developed in an extremely short period. More specifically, compared to all previous human vaccines, the COVID-19 vaccines were developed in much shorter time periods. Consequently, individuals worldwide are being encouraged to have a COVID-19 vaccination based on much less scientific evidence compared to other vaccines. Second, since the beginning of the COVID-19 pandemic, there has been much misinformation and many conspiracy theories that may increase individuals’ hesitance and resistance to uptaking COVID-19 vaccination.28 Third, in addition to the original three core components of the TPB, further components (e.g., knowledge on COVID-19 vaccines, risk perception COVID-19, and past behaviors of vaccination uptake) that can amplify the efficacy of the TPB should be tested to construct an extended TPB to better predict behavioral intentions regarding the uptake of COVID-19 vaccination.
Knowledge about vaccines and risk perception of risk due to disease are two possible components that warrant examining in relation to the intention to uptake vaccination. These two important factors are also applicable to COVID-19 (i.e., knowledge about COVID-19 vaccines and risk perception of COVID-19 are important factors in relation to the intention to uptake COVID-19 vaccination). Knowledge concerning the benefits of COVID-19 vaccination have been positively associated with COVID-19 vaccination uptake intentions.26 Moreover, risk perception is associated with individuals’ health-related attitudes,29 and perceived high risk of contracting COVID-19 also increases the likelihood of preventive behaviors such as wearing a mask, washing hands, and keeping social/spatial distance.26,30 However, the role of knowledge concerning COVID-19 vaccines and risk of COVID-19 may contribute individuals’ favorable attitude toward COVID-19 vaccines and therefore increase intention to uptake.
Past influenza vaccine uptake is another component that warrants inclusion in the extended TPB explaining the intentions to uptake COVID-19 vaccination. A systematic review of influenza vaccination intention and behaviors identified past vaccination behaviors as one of factors predicting current intentions to influenza vaccination.18 However, whether past influenza vaccination behaviors predict the intentions to uptake COVID-19 vaccination is unknown. Therefore, the present study incorporated knowledge concerning COVID-19 vaccination, risk perception of COVID-19, and past influenza vaccination uptake with the TPB’s key factors (i.e., attitude, subjective norm, and perceived behavioral control) to predict the intentions to uptake COVID-19 vaccination among university students in China. University students are generally considered as low-risk groups and are not among the priority groups in getting vaccinated. Consequently, university students might not pay full attention to the vaccine information and may not be fully aware of the importance of vaccination. However, when fighting against COVID-19, vaccinating everyone is paramount. Therefore, it is extremely important to include university students and understand their intentions concerning vaccination. The following hypotheses were proposed:
H1: Knowledge concerning COVID-19 vaccination will be positively associated with attitude toward COVID-19 vaccination uptake.
H2: Risk perception of COVID-19 will be positively associated with attitude toward COVID-19 vaccination uptake.
H3: Attitude toward COVID-19 vaccination will be positively associated with the intentions toward COVID-19 vaccination uptake.
H4: Subjective norm will be positively associated with the intentions toward COVID-19 vaccination uptake.
H5: Perceived behavioral control will be positively associated with the intentions toward COVID-19 vaccination uptake.
H6: Past influenza vaccination uptake will be positively associated with the intentions toward COVID-19 vaccination uptake.
Methods
Participants and recruitment procedure
The Institutional Review Board of the Jianxi Psychological Consultant Association (IRB ref: JXSXL-2020-DE22) approved the study protocol. The study comprised an online survey method utilizing non-probability sampling. The data were collected between January 5 and 16, 2021, a period in which mainland China had begun COVID-19 vaccination uptake. However, university students are not the priority population in getting COVID-19 vaccination. Therefore, authorities have not promoted vaccination uptake for university students. However, the students can get vaccinated if they themselves go to a hospital.
To recruit the sample, college counselors in different universities were first approached by the research team to help launch the online survey and disseminate the study information to the target population (i.e., university students) via their respective online social communities. The present study recruited 3145 mainland Chinese students who were voluntarily willing to participate in the survey. All the students were clearly informed of their right in participation, including the confidentiality and the anonymity of their data, on the first page of the online survey. All participants provided informed consent and completed all the survey items given that the survey platform did not allow missing answers. Therefore, no missing data were observed in the present study. Moreover, there were only two inclusion criteria for participants. These were that they were (i) students studying in an undergraduate or a postgraduate university program in mainland China, and (ii) aged 18 years or over.
Measures
Theory of Planned Behavior (TPB) measures.
Attitudes in the TPB were assessed using six items rated on a seven-point scale from 1 (strongly disagree) to 7 (strongly agree). The scale had excellent internal reliability (0.93), average variance extracted (0.69), and composite reliability (0.93). A sample item is “Vaccination is a very effective way to protect myself against COVID-19”. A higher score indicates a more positive attitude toward COVID-19 vaccination uptake.
Subjective norms in the TPB were assessed using two items rated on a four-point scale from 1 (not important at all) to 4 (very important). The items had very good internal reliability (0.86), average variance extracted (0.76), and composite reliability (0.86). A sample item is “Is your family an important factor for you to get vaccinated against COVID-19?”. A higher score indicates a higher level of subjective norms.
Perceived behavioral control in the TPB was assessed using a single item (“I can choose whether to get a COVID-19 vaccination or not”) rated on a seven-point scale. A higher score indicates a higher level of self-efficacy in getting vaccinated against COVID-19.
The intention to get vaccinated against COVID-19 in the TPB was assessed using two items. One item (“When a COVID-19 vaccine becomes available, will you get vaccinated?”) was rated on a four-point scale from 1 (definitely unwilling) to 4 (definitely willing). The second item (“Please rate your current level of willingness to receive a COVID-19 vaccine”) was rated from 1 (very low) to 10 (very high) on a visual analogue scale. The internal reliability (0.72), average variance extracted (0.56), and composite reliability (0.72) of the two intention items were acceptable. A higher score indicates more willingness to get COVID-19 vaccinated.
Knowledge measure.
Knowledge concerning COVID-19 vaccination was assessed using two items rated on a seven-point scale from 1 (strongly disagree) to 7 (strongly agree). The two items had very good internal reliability (0.84), average variance extracted (0.72), and composite reliability (0.84). A sample item is “I know very well how vaccination protects me from COVID-19”. A higher score indicates a better level of knowledge concerning COVID-19 vaccination.
Risk perception measure.
Risk perception of COVID-19 infection was assessed using four items rated on a seven-point scale from 1 (not at all) to 7 (certain). The scale had acceptable internal reliability (0.75), average variance extracted (0.45), and composite reliability (0.75). A sample item is “What do you think are your chances of getting COVID-19 over the next one month compared to others outside your family?”. A higher score indicates a higher level of perceived COVID-19 infection.
Past influenza vaccine behavior measure.
Past influenza vaccine behavior was assessed using a single item (“Did you receive an influenza vaccination in the past few years?”). The item was rated on a four-point scale from 1 (never) to 4 (always). A higher score indicates a higher level of adherence to getting vaccinated against influenza.
Background information measures.
Several demographic questions (i.e., age, gender, major study in the university, and level of education [undergraduate vs. postgraduate]) were also asked in the survey.
Data analysis
Descriptive statistics were analyzed using the standard procedure such as means and frequencies to illustrate the participants’ characteristics, including their demographics and mean scores of the measures used in the proposed model (Figure 1; please see below for detailed information). Pearson correlation coefficients were calculated to understand the zero-order associations between the studied variables. Finally, the proposed model was examined using the structural equation modeling (SEM) method with the maximum likelihood estimator and bootstrapping method. More specifically, the proposed model is outlined in Figure 1, where knowledge and risk perception are the explanatory factors underlying attitude; attitude in turn is the explanatory factor underlying intention to have a COVID-19 vaccine; subjective norms, perceived behavioral control, and past behavior concerning influenza vaccination uptake are also the explanatory factors underlying intention to have a COVID-19 vaccination. All the explanatory factors were constructed latently, except for those variables assessed only using one item (i.e., perceived behavioral control and past behavior). Moreover, two indirect effects were examined in the model: (i) the path between knowledge and intention toward COVID-19 vaccination uptake via attitude, and (ii) the path between risk perception and intention toward COVID-19 vaccination uptake via attitude. For the two indirect effects, bootstrapping method with 5000 bootstrapping samples was used to examine whether the indirect effects were significant. A significant indirect effect is supported when its 95% confidence interval (i.e., the range between upper limit confidence interval [ULCI] and lower limit confidence interval [LLCI]) does not contain 0.31
Figure 1.
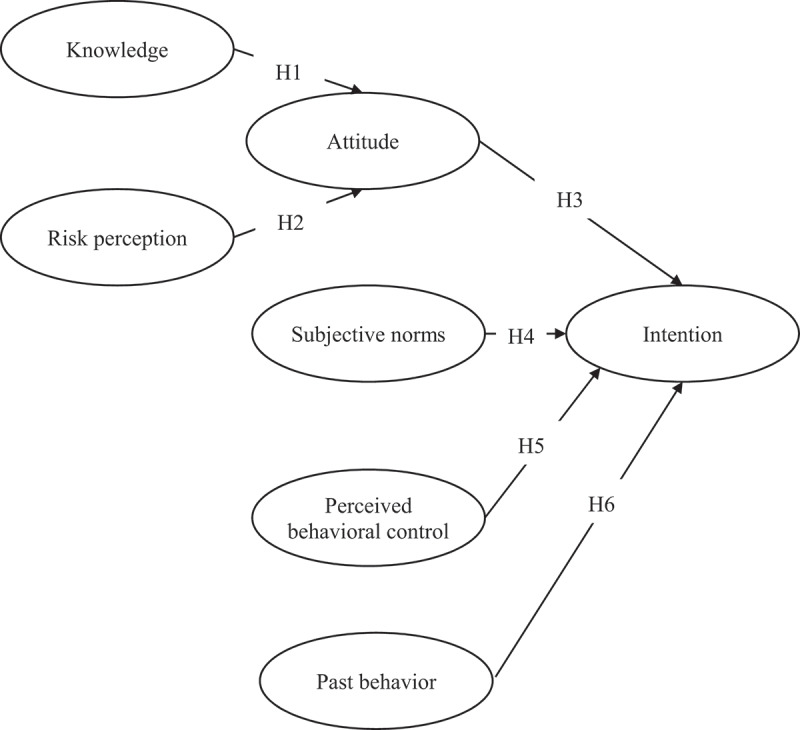
The proposed model in explaining COVID-19 vaccination uptake among mainland Chinese university students
Results
The participants came from 30 provinces in mainland China (covering 88% of the mainland China’s provinces). The participants’ characteristics are presented in Table 1. A relatively balanced gender distribution was found among the recruited participants (1578 females; 50.2%) and the participants were relatively young (mean age = 20.80 years; SD = 2.09) with most of them were studying on undergraduate programs (n = 3026; 96.2%). Less than 10% of the participants were studying a program related to health (n = 241; 7.7%). When comparing the demographics of the present sample and all mainland Chinese university students (https://www.wutongguo.com/report/223.html; https://job.hunnu.edu.cn/detail/student_source_info?menu_id=261; http://www.moe.gov.cn/s78/A03/moe_560/jytjsj_2019/qg/202006/t20200611_464803.html), no significant differences were found in gender distribution (χ2 = 0.08; p = .77), education level (χ2 = 1.42; p = .23), and the program studied at the university (χ2 = 0.31; p = .58). However, the present sample (mean age 20.8 years) was slightly older than the mainland Chinese university students, whose mean age was 20.0 years (t = 19.12; p < .001). Moreover, the participants’ scores in the measures that were used in the proposed model are presented in Table 1.
Table 1.
Participants’ characteristics (N = 3145)
| M (SD) or n (%) | Total range | |
|---|---|---|
| Gender (female) | 1578 (50.2%) | – |
| Age | 20.80 (2.09) | 18–40 |
| Education level (undergraduate) | 3026 (96.2%) | – |
| Professional (health-related) | 241 (7.7%) | – |
| Knowledge | 5.62 (1.15) | 1–7 |
| Risk perception | 3.06 (1.18) | 1–7 |
| Past behavior relating to influenza vaccination | 1.71 (0.84) | 1–4 |
| Attitude toward COVID-19 vaccination | 5.82 (0.94) | 1–7 |
| Vaccination is a very effective way to protect myself against COVID-19 | 5.76 (1.16) | 1–7 |
| It is important that I get the COVID-19 vaccination. | 5.93 (1.38) | 1–7 |
| Vaccination greatly reduces my risk of catching COVID-19. | 5.94 (1.08) | 1–7 |
| The contribution of the COVID-19 vaccination to my health and well-being is very important | 6.00 (1.06) | 1–7 |
| The COVID-19 vaccination plays an important role in protecting my life and that of others | 5.88 (1.14) | 1–7 |
| Getting the COVID-19 vaccination has a positive influence on my health | 5.42 (1.39) | 1–7 |
| Subjective norms toward COVID-19 vaccination | 2.87 (0.82) | 1–4 |
| Perceived behavioral control toward COVID-19 vaccination | 5.78 (1.24) | 1–7 |
| Intention toward COVID-19 vaccination | 5.31 (1.44) | 1–7 |
Table 2 shows the correlations between the studied variables used in the proposed model. The proposed model was supported by most of the SEM fit indices (RMSEA = 0.061, SRMR = 0.055, TLI = 0.974, and CFI = 0.980) and only the significant χ2 test (χ2 = 1544.648, df = 120; p < .001) did not support the data-model fit (Figure 2). Moreover, all the tested paths were significant, except for the path between subjective norms and intention toward COVID-19 vaccination uptake (p = .052) and that between perceived behavioral control and intention toward COVID-19 vaccination uptake (p = .778). More specifically, the standardized coefficients were 0.98 between knowledge and attitude (p < .001); 0.08 between risk perception and attitude (p < .001); 0.70 between attitude and intention toward COVID-19 vaccination uptake (p < .001); and 0.10 between past influenza vaccination uptake and intention toward COVID-19 vaccination uptake (p < .001) (Figure 2).
Table 2.
Correlation matrix between variables used in the proposed model
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Knowledge | 1 | ||||||
| 2. Risk perception | −.148** | 1 | |||||
| 3. Attitude | .775** | −.093** | 1 | ||||
| 4. Subjective norms | .013 | .075** | .004 | 1 | |||
| 5. Perceived behavioral control | .477** | −.096** | .558** | .017 | 1 | ||
| 6. Past behaviora | .024 | .112** | .011 | .030 | .016 | 1 | |
| 7. Intention | .367** | .096** | .487** | −.021 | .280** | .061** | 1 |
**p < 0.01.
aPast behavior relating to influenza vaccination.
Figure 2.
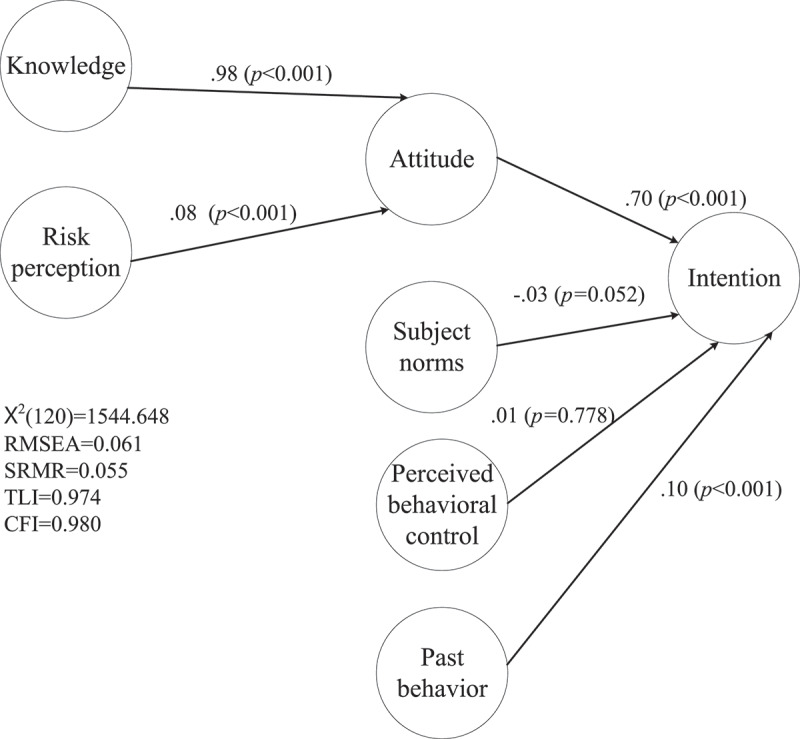
Results of the proposed model in explaining COVID-19 vaccination uptake among mainland Chinese university students
The indirect effects proposed in the model were both supported by the SEM results. More specifically, the unstandardized coefficient in the path between knowledge and intention toward COVID-19 vaccination uptake via attitude was 0.389 (bootstrap SE = 0.020; ULCI = 0.429; LLCI = 0.350); and the path between risk perception and intention toward COVID-19 vaccination uptake via attitude was 0.011 (bootstrap SE = 0.005; ULCI = 0.023; LLCI = 0.0002) (Table 3).
Table 3.
Direct and indirect effects in the proposed model
| Direct path | Coeff. | SE | t-value | p-value |
|---|---|---|---|---|
| Knowledge→Attitude | .983 | .019 | 49.96 | <0.001 |
| Risk perception→Attitude | .084 | .026 | 5.474 | <0.001 |
| Attitude→Intention | .698 | .030 | 23.045 | <0.001 |
| Subjective norms→Intention | −.035 | .019 | −1.946 | 0.052 |
| Perceived behavioral control→Intention | .008 | .022 | .281 | 0.778 |
| Past behaviora→Intention |
.097 |
.017 |
4.372 |
<0.001 |
| Indirect path |
Coeff. |
SE |
ULCI |
LLCI |
| Knowledge→Attitude→Intention | .389 | .020 | .429 | .350 |
| Risk perception→Attitude→Intention | .011 | .005 | .023 | .0002 |
Coeff. = coefficient (unstandardized coefficients 0029; SE = standard error; ULCI = upper limit of confidence interval at 95%; LLCI = lower limit of confidence interval at 95%.
The indirect paths were tested using bootstrapping methods (5000 bootstrapping samples).
aPast behavior relating to influenza vaccination.
Discussion
To the best of the present authors’ knowledge, the present study is the first large-scale study to examine university students’ intention toward getting a COVID-19 vaccine, and comprised 43 universities and 3145 participants across mainland China. The study used the key components in the TPB (i.e., attitude, subjective norms, and perceived behavioral control), and other relevant components (i.e., knowledge, risk perception, and the past vaccination behavior) to augment the efficacy of TPB in explaining intention toward COVID-19 vaccination uptake.
The results supported the hypotheses that students’ knowledge concerning COVID-19 vaccine (H1) and risk perception of COVID-19 (H2) would positively influence their attitude toward COVID-19 vaccination uptake. Additionally, students’ attitude (H3) toward COVID-19 vaccination as well as their past influenza vaccination uptake behavior (H6) were positively associated with the intentions toward COVID-19 vaccination uptake. On the other hand, two hypotheses were not supported. More specifically, subjective norm (H4) and perceived behavioral control (H5) were not significant predictors for the intentions toward COVID-19 vaccination uptake. Nevertheless, in general, the present study’s findings support the premise that the TPB can be used to understand university students’ intention toward COVID-19 uptake and explain health-related behavior,21 as well as extended TPB appearing to augment the efficacy of original TPB.32
Original TPB components in explaining intention to uptake COVID-19 vaccination
In the present study, Chinese university students were positive about the COVID-19 vaccine (an average score of 5.82 on a seven-point Likert scale), which is in line another Chinese study reporting that only 16.4% would definitely or probably decline getting the COVID-19 vaccine.33 Moreover, the finding that students’ attitude toward the COVID-19 vaccine was strongly associated with their vaccination intention is consistent with recent previous studies,34,35 including the one that found positive attitude toward the vaccine is a significant predictor of COVID-19 vaccine uptake intentions.26
However, subjective norm was not a significant predictor for COVID-19 vaccine intention. In other words, students’ perception of judgment from others was not a significant predictor for their own behavior and intention. This was in line with a previous study in which subjective norms did not predict physical activity behavior of patients on hemodialysis.36 However, the finding contradicts other studies. For example, Guidry et al.26 found that individuals who had a more positive attitude toward vaccination, scored higher on subjective norms and had higher COVID-19 vaccine uptake intention. Also, Lin et al.33 found in their study that knowing the vaccine has been taken by many individuals from the general public may serve as a cue in uptake of COVID-19 vaccination. One of the possible explanations is that both previous studies were conducted during the relatively early period of the COVID-19 pandemic. Guidry et al.26 completed their survey in July 2020, and Lin et al.33 completed their survey in May 2020. During that period, the information concerning COVID-19 was still unclear with arguments and debates on a variety of topics concerning COVID-19 coming from public officials, scientists, and stakeholders across various media platforms.37 It is possible that participants would lean more toward their family members or important others, which resulted in the subjective norm being much more important to their vaccination intention when the pandemic started. Instead, the present study completed data collection in January 2021, in which more open discussion and evidence were available and individuals were generally more clear concerning COVID-19 information. Therefore, participants in the present study may have already made up their own mind in relation to their personal intention toward COVID-19 vaccination uptake.
Perceived behavioral control was also not a significant predictor toward intention for COVID-19 vaccination uptake. This finding also contradicts with previous studies. For example, Zhang et al.27 found that perceived behavioral control of having children uptake COVID-19 vaccination was associated with higher parental acceptability of COVID-19 vaccination for children. Additionally, Guidry et al.26 found that high perceived behavioral control was a significant predictor of willingness to take a COVID-19 vaccine. Moreover, Xiao et al.25 found that perceived behavioral control was a significant predictor of vaccination intentions among 5149 participants from five databases. The difference in findings is likely explained by Chinese society’s expectation of who should receive a COVID-19 vaccination first More specifically, frontline healthcare workers who have a higher risk of exposure to COVID-19 and those aged 65 years have the highest priority in receiving a COVID-19 vaccination.38 In contrast, the present study’s participants were university students, a population that has a lower priority in COVID-19 vaccination uptake. Being low priority may have influenced the students’ confidence in COVID-19 vaccination uptake and further influenced the association between perceived control and intention toward COVID-19 vaccination uptake.
Other components in the extended TPB
The finding that knowledge concerning the COVID-19 vaccine was directly associated with attitude and indirectly with intention is consistent with previous studies.9,39–41 Concerns about vaccine safety is a commonly cited reason for being unsure about whether to get a vaccination.42 Therefore, when individuals have the safety knowledge concerning COVID-19 vaccination, their intention toward COVID-19 vaccination uptake is increased. Indeed, Fisher et al.9 indicated that their study participants wanted more information about the vaccine, such as its compatibility with personal health conditions and whether it is recommended by doctors or official organizations. Moreover, Grech and Gauci43 conducted an online survey with 852 participants from Health Sciences, Dentistry and Medicine departments and found that participants were most concerned about the potential long-term side effects of the COVID-19 vaccine.
Apart from knowledge, students’ risk perception of the COVID-19 vaccine was another significant factor directly associated with their attitude and was indirectly associated with intention. This result concurs with other studies.26,34,35,44 For example, a study of 1062 US college students34 found that perceived severity and fear of COVID-19 were positively associated with their attitude of vaccine acceptance. Moreover, similar findings have been reported in other populations, such as those in France and Israel.42,44,45 Therefore, the importance of risk perception in explaining an individual’s attitude toward vaccination uptake should not be ignored.
Past vaccination uptake behaviors were directly and strongly associated with intention toward COVID-19 vaccination uptake. This result is also consistent with other relevant studies. For instance, individuals who have received the seasonal influenza vaccine in the previous year report higher intention to get the COVID-19 vaccine across the world compared to those that have not.9,35,40,43,46 Similarly, a cross-sectional study from 32,361 UK adults found that individuals who had not received a past vaccine were twice as uncertain about the COVID-19 vaccine and 3.4 times more likely to refuse the COVID-19 vaccine than those who had previously received vaccines.40
Limitations
A few limitations should be noted when interpreting the present study’s results. First, although the study had a large sample size across 43 universities from China, the students comprised a convenience sample and voluntarily participated in the study. Therefore, the generalizability of the present findings is restricted. Additionally, the students who chose to take a part in this survey might share different characteristics than those who chose not to participate, which may have resulted in biased information. Second, this study used a cross-sectional design and had no long-term follow up. Given that information related to COVID-19 vaccines is released in a daily basis, students’ knowledge, risk perception, attitude, and subjective norms toward COVID-19 vaccination may potentially change over time. However, the cross-sectional design prevents the capturing of such changes. Additionally, recall bias commonly exists in cross-sectional studies and should be taken into consideration when interpreting the results. Some questions asked students to recall their past behaviors (e.g., “Did you receive an influenza vaccination in the past few years?”). Therefore, recall bias cannot be excluded. Third, students’ knowledge concerning COVID-19 vaccination was evaluated by their subjective perceptions, which cannot be used to represent the objective knowledge level. Therefore, the interpretation of the results should be treated with caution when taking subjective perspectives into consideration. Finally, the survey did not include quality control items to ensure the validity for every answer (e.g., asking what 1 + 1 is after item answers to ensure that the participants were paying attention to the survey items). Therefore, future studies are needed to consider using this type of quality control to ensure survey validity.
Conclusions
The present study used the extended TPB to provide useful guidance for tailored students’ perceptions to enhance intention of acceptance for new COVID-19 vaccines.
It demonstrated that the extended TPB appears to be an efficient model with the focus on attitude, knowledge, risk perception, and past influenza vaccination uptake behaviors in explaining students’ intention for COVID-19 vaccination. Groundwork for public acceptance of COVID-19 vaccines should be the foundation of vaccine distribution alongside public health campaigns that counter misinformation and conspiracy theories concerning the efficacy and safety of COVID-19 vaccines. Public health efforts to increase acceptability among student populations should start immediately.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Crayne MP.The traumatic impact of job loss and job search in the aftermath of COVID-19. Psychol Trauma. 2020;12(S1):S180–S182. doi: 10.1037/tra0000852. [DOI] [PubMed] [Google Scholar]
- 2.McIntyre RS, Lee Y.. Preventing suicide in the context of the COVID-19 pandemic. World J Psychiatry. 2020;19(2):250–51. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–93. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oksanen A, Kaakinen M, Latikka R, Savolainen I, Savela N, Koivula A. Regulation and trust: 3-month follow-up study on COVID-19 mortality in 25 European countries. JMIR Public Health Surveill. 2020;6(2):e19218. doi: 10.2196/19218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19 related school closings and risk of weight gain among children. Obesity. 2020;28(6):1008–09. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–20. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization . DRAFT landscape of COVID-19 candidate vaccines. 2021. [assessed 2021 Feb 23]. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines .
- 8.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35(8):781–83. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. Adults. Ann Intern Med 2020;173(12):964–73. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Setiawan AM, Rajamoorthy Y, Sofyan H, Mudatsir M. Acceptance of a COVID-19 vaccine in southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–82. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500–07. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams L, Gallant AJ, Rasmussen S, Brown Nicholls LA, Cogan N, Deakin K, Young D, Flowers P. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020;25(4):1039–54. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 15.Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccines Immunother. 2020;16(9):2204–14. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763–73. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prestwich A, Webb TL, Conner M. Using theory to develop and test interventions to promote changes in health behaviour: evidence, issues, and recommendations. Curr Opin Psychol. 2015;5:1–5. doi: 10.1016/j.copsyc.2015.02.011. [DOI] [Google Scholar]
- 18.Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PloS One. 2017;12(1):e0170550. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu AMS, Lau JTF, Ma YL, Cheng KM, Lau MMC. A longitudinal study using parental cognitions based on the theory of planned behavior to predict childhood influenza vaccination. J Infect Public Health. 2020;13(7):970–79. doi: 10.1016/j.jiph.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Catalano HP, Knowlden AP, Birch DA, Leeper JD, Paschal AM, Usdan SL. Using the theory of planned behavior to predict HPV vaccination intentions of college men. J Am Coll Health. 2017;65(3):197–207. doi: 10.1080/07448481.2016.1269771. [DOI] [PubMed] [Google Scholar]
- 21.Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(4):471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 22.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action control. SSSP Springer series in social psychology. Berlin (Heidelberg): Springer; 1985. p. 11–39. doi: 10.1007/978-3-642-69746-3_2. [DOI] [Google Scholar]
- 23.Ajzen I, Fishbein MA. Bayesian analysis of attribution processes. Psychol Bull. 1975;82(2):261–77. doi: 10.1037/h0076477. [DOI] [Google Scholar]
- 24.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 25.Xiao X, Wong RM. Vaccine hesitancy and perceived behavioral control: a meta-analysis. Vaccine. 2020;38(33):5131–38. doi: 10.1016/j.vaccine.2020.04.076. [DOI] [PubMed] [Google Scholar]
- 26.Guidry J, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, Ryan M, Fuemmeler BF, Carlyle KE. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–42. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang KC, Fang Y, Cao H, Chen H, Hu T, Chen YQ, Zhou X, Wang Z. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: cross-sectional online survey. JMIR Pediatr Parent. 2020;3(2):e24827. doi: 10.2196/24827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.French J, Deshpande S, Evans W, Obregon R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int J Environ Res Public Health. 2020;17(16):5893. doi: 10.3390/ijerph17165893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ho SS, Scheufele DA, Corley EA. Value predispositions, mass media, and attitudes toward nanotechnology: the interplay of public and experts. Sci Commun. 2011;33(2):167–200. doi: 10.1177/1075547010380386. [DOI] [Google Scholar]
- 30.Majid U, Wasim A, Bakshi S, Truong J. Knowledge, (mis-)conceptions, risk perception, and behavior change during pandemics: a scoping review of 149 studies. Public Underst Sci. 2020;29(8):777–99. doi: 10.1177/0963662520963365. [DOI] [PubMed] [Google Scholar]
- 31.Lin C-Y, Tsai M-C. Effects of family context on adolescents’ psychological problems: moderated by pubertal timing, and mediated by self-esteem and interpersonal relationships. Appl Res Qual Life. 2016;11(3):907–23. doi: 10.1007/s11482-015-9410-2. [DOI] [Google Scholar]
- 32.Conner M. Extending not retiring the theory of planned behaviour: a commentary on Sniehotta, Presseau and Araújo-Soares. Health Psychol Rev. 2015;9(2):141–45. doi: 10.1080/17437199.2014.899060. [DOI] [PubMed] [Google Scholar]
- 33.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP, Understanding COVID-19. vaccine demand and hesitancy: a nationwide online survey in China. PLOS Negl Trop Dis. 2020;14(12):e0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qiao S, Tam CC, Li X. Risk exposures, risk perceptions, negative attitudes toward general vaccination, and COVID-19 vaccine acceptance among college students in South Carolina. medRxiv. 2020. doi: 10.1101/2020.11.26.20239483. [DOI] [PubMed] [Google Scholar]
- 35.Pogue K, Jensen JL, Stancil CK, Ferguson DG, Hughes SJ, Mello EJ, Burgess R, Berges BK, Quaye A, Poole BD. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines. 2020;8(4):582. doi: 10.3390/vaccines8040582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pakpour AH, Zeidi IM, Chatzisarantis N, Molsted S, Harrison AP, Plotnikoff RC. Effects of action planning and coping planning within the theory of planned behaviour: a physical activity study of patients undergoing haemodialysis. Psychol Sport Exerc. 2011;12(6):609–14. doi: 10.1016/j.psychsport.2011.06.008. [DOI] [Google Scholar]
- 37.Bao H, Cao B, Xiong Y, Tang W. Digital media’s role in the COVID-19 pandemic. JMIR Mhealth Uhealth. 2020;8(9):e20156. doi: 10.2196/20156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang J, Zheng W, Shi H, Yan X, Dong K, You Q, Zhong G, Gong H, Chen Z, Jit M, et al. Who should be prioritized for COVID-19 vaccination in China? A descriptive study. BMC Med. 2021;19(1):45. doi: 10.1186/s12916-021-01923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Most BS.Americans would take coronavirus vaccine if deemed safe: reuters/Ipsos poll. Reuters Health News. 2020. [assessed 2021 March 8]. http://www.reuters.com/article/us-health-coronavirus-usa-pollmost-americans-would-take-coronavirus-vaccine-if-deemed-safe-reuters-ipsos-poll-idUSKBN22I019. [Google Scholar]
- 40.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg Health-Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Taylor S, Landry CA, Paluszek MM, Groenewoud R, Rachor GS, Asmundson GJG. A proactive approach for managing COVID-19: the importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front Psychol. 2020;19(11):575950. doi: 10.3389/fpsyg.2020.575950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Karafillakis E, Larson HJ, ADVANCE consortium . The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35(37):4840–50. doi: 10.1016/j.vaccine.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 43.Grech V, Gauci C. Vaccine hesitancy in the University of Malta faculties of health sciences, dentistry and medicine vis-à-vis influenza and novel COVID-19 vaccination. Early Hum Dev. 2020:105258. doi: 10.1016/j.earlhumdev.2020.105258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–06. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–79. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. medRxiv. 2020. doi: 10.1101/2020.12.20.20248587. [DOI] [PMC free article] [PubMed] [Google Scholar]


