Abstract
Introduction
Herlyn-Werner-Wunderlich syndrome is a rare congenital disorder that consists of a didelphic uterus, hemivaginal septum, and unilateral renal agenesis. Both diagnosis and management can be challenging in low-income countries.
Case presentation
a 13-year-old female who experienced recurrent pelvic pain, dysmenorrhea, and abdominal mass for one month. We could not obtain the MRI as it was unavailable in our hospital, and the patient cannot afford its expensive cost in a private center. Instead, US showed an absent right kidney and doubled uterus with a heterogeneous cystic formation. A pelvic CT scan revealed an absent right kidney, an enlarged left kidney, a double uterus, and a left hematocolpos. We established the diagnosis of Herlyn-Werner-Wunderlich syndrome and started planning for correcting the anomalies via laparotomy.
Discussion
ultrasound detects uterus didelphys, hematocolpos, hematometrocolpos, and renal agenesis but cannot identify the vaginal septum and the type of müllerian defect. The MRI is more convenient for a thorough assessment, but it is a high-priced diagnostic method.
Conclusion
although MRI is the gold standard for establishing the diagnosis and preoperative planning, ultrasound and CT scan can be an alternative, less expensive, and reliable approach. In addition, Laparoscopy or vaginoscopy may not be available in these countries. Therefore, correcting the anomalies can be achieved with laparotomy, which results in acceptable outcomes without any complications.
Keywords: Herlyn-Werner-Wunderlich syndrome, OHVIRA syndrome, Renal agenesis, Didelphic uterus, Müllerian anomalies, Background
Highlights
-
•
Herlyn-Werner-Wunderlich Syndrome is a rare müllerian anomaly.
-
•
Although MRI can implant the diagnosis, US and CT scan are a sufficient alternative approach.
-
•
Laparotomy can be used to correct the anomaly while preserving the hymen with minimal or no post-operative complications.
Herlyn Werner Wunderlich syndrome is a rare congenital disorder of müllerian ducts [1]. It is first reported in a 16-year-old patient in 1922 [2]. The etiology is unknown, but it implies a failure of the müllerian ducts to fuse during embryogenesis [1,3]. Furthermore, genetic and environmental factors may affect embryogenesis. Its incidence varies between 0.1 and 3% [3].Herlyn Werner Wunderlich syndrome is defined by the classic triad: a didelphic uterus, hemivaginal septum, and unilateral renal agenesis [1]. However, cases have been reported without renal agenesis [4].
MRI is the cornerstone for the diagnosis as it can provide a comprehensive appraisal of müllerian abnormalities and help in preoperative planning [5,6]. However, it is an expensive diagnostic method [6,7]. The 2D ultrasound and CT scan may present an alternative approach to confirm the diagnosis [1,8]. Ultrasound exposes uterus didelphys, hematocolpos, hematometrocolpos, and renal agenesis [5].Therefore, ultrasound may be sufficient to establish the correct diagnosis and begin treatment [9]. Management of Herlyn Werner Wunderlich syndrome based on drainage of the hematocolpos and resection vaginal septum, either through laparoscopy or vaginoscopy [7,10].
Herein, we present an alternative approach that depends on ultrasonographic and CT scan findings to diagnose Herlyn Werner Wunderlich syndrome in low-income countries. Moreover, while vaginoscopy or laparoscopy may be unavailable in these countries, we describe the management with laparotomy while preserving the hymen.
This manuscript has been reported in line with SCARE's 2020 Criteria [11].
1. Presentation of case
A 13-year-old girl is brought to our department by her parents complaining about periodical pelvic pain for the last month accompanied by dysuria and polyuria. She did not report any fever, vomiting, or diarrhea. Her first menstruation was at 12 years; since then, it was regular but lasted for two or three days with scanty menstrual blood; and was associated with abdominal discomfort. A previous doctor prescribed her some analgesics to relieve her symptoms, but recently the pain became more severe with no response to medications. She was born at term without any complications, had no family history of congenital diseases, and her medical and surgical history was unremarkable. Her developmental milestones and external reproductive organs were conventional.
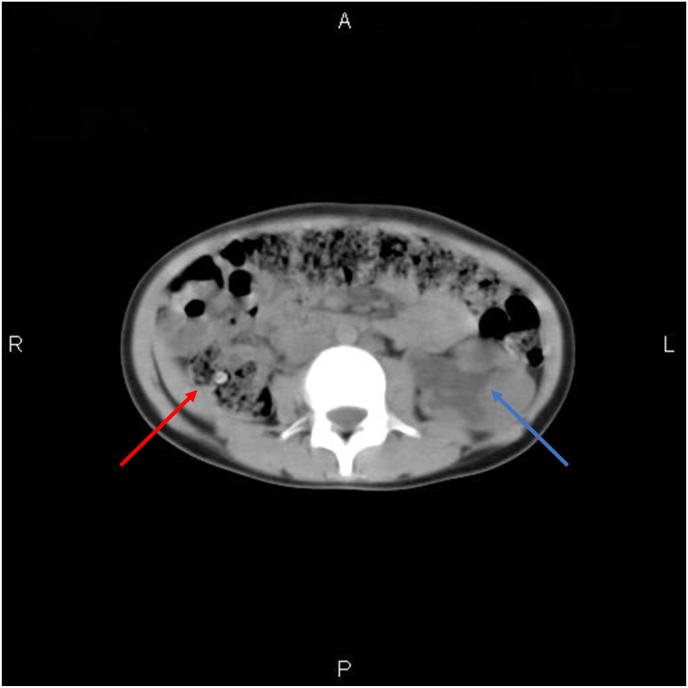
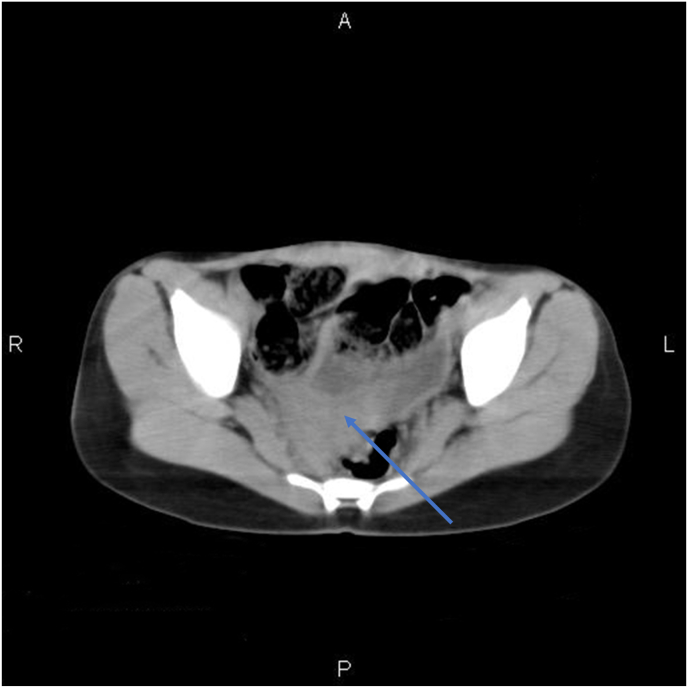
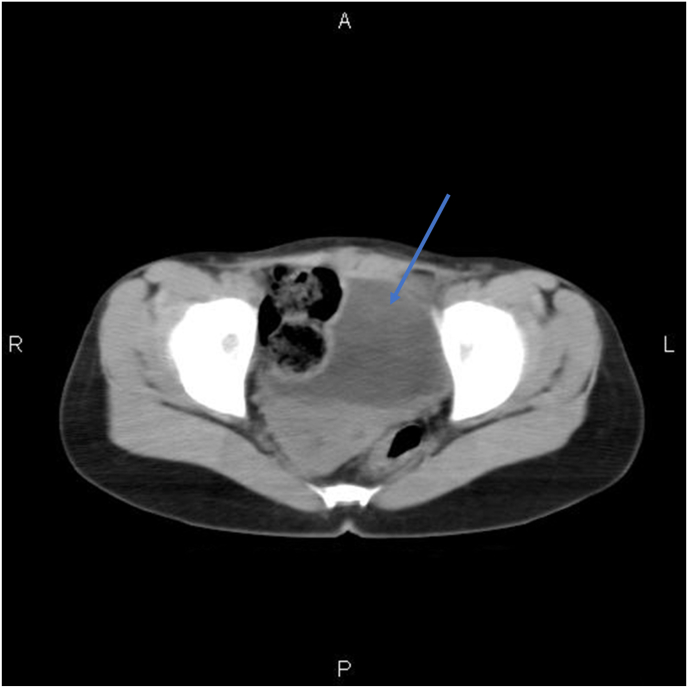
At admission, she was afebrile, and her vital signs were in the normal range. On physical examination, she had a mild pallor. We palpate a tender, mobile, painless mass on the left flank. Lab examination showed an elevated white blood cell count (13.3 × 103/μl: granulocytes: 93.6%; lymphocytes: 4.5%) and microcytic anemia (red blood cell: 4.86 × 106/μl, hemoglobin: 10.4 g/dl, hematocrit: 34.5%, MCV: 71.0 fl). Creatinine and urea levels were normal (1.1 mg/dl and 17 mg/dl, respectively). Albumin levels were within the reference range (4.9 g/dl). The 2D ultrasound showed an absent right kidney, a doubled uterus with a heterogeneous cystic formation measures 110 × 63 × 60 mm in the left cervix compressing the lower portion of the ureter resulting in second-degree left hydronephrosis; an enlarged left kidney (49.2 × 49.3 mm) with dilated renal pelvis and calyces; mild decreased in the cortical thickness (6.9 mm). We could not obtain the MRI as it was unavailable in our hospital, and the patient cannot afford its expensive cost in a private center. Instead, a pelvic CT scan was obtained and revealed an absent right kidney, an enlarged left kidney measures 49.2 × 49.3 mm (Fig. 1), and a double uterus (Fig. 2) with left cervical hematocolpos measures 110 × 63 × 60 mm in diameter (Fig. 3).
Fig. 1.
Shows a hydronephrosis of the left kidney (Blue arrow), and an absent right kidney (Red arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Exhibits the didelphic uterus (Blue arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
Shows the left hematocolpos (Blue arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Our final diagnosis was Herlyn Werner Wunderlich syndrome which is complicated with hydronephrosis. Although hysteroscopy is a less invasive approach, it was unavailable in our department. We explained to her parents that laparotomy is a more invasive procedure, and they gave their informed consent. She underwent a laparotomy under general anesthesia. We opened the abdomen with a Pfannenstiel incision. We observed severe adhesions between the intestines and the peritoneum and around the uterus, fallopian tubes, ovaries, and bladder. We excised the adhesions using electrocautery. Laparotomy showed two separate infantile vaginas. The entire left genital tract was constant, but the right one exposed a right, transverse vaginal septum with an enlarged vagina (20 × 9 cm) containing chocolate-colored blood. A mildly dilated left ureter was observed. We performed a longitudinal fissure between the two vaginas and drained the hematocolpos to reach the septum that separates the two vaginas. We made a longitudinal fissure between the distinct vaginas, removed a thin layer, and used simple interrupted sutures to establish a connection between the two cavities; by this approach, we maintain blood drainage via a right-to-left shunt (Fig. 4). The hymen remained intact. We infused a saline solution, put a drainage tube in Douglas's pouch, and closed the abdomen layers. None of the operation-related complications occurred (e.g., bladder or rectal injury). The patient did not need a blood transfusion, and she was discharged four days later in good general condition.
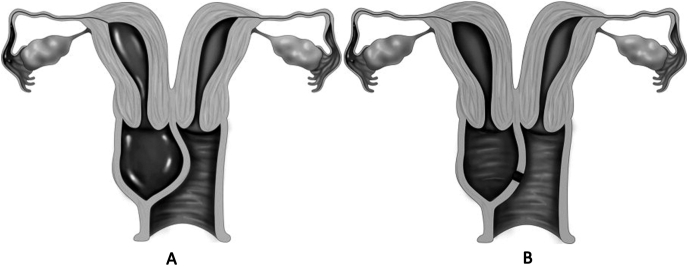
Fig. 4.
Illustrates the opening between the two vaginas that allows for blood passage.
Our patient experienced endometriosis, infections, and pelvic adhesions as the main complications of Herlyn Werner Wunderlich syndrome. Two months postoperatively, she came for a follow-up appointment. She was healthy and her menstruation improved within two cycles. Her anemia has also improved. Kidney function tests were normal. Ultrasound examination showed normal findings without any cystic or fluid formation or any signs of hydronephrosis.
2. Discussion
The reproductive system of both genders during the first six weeks is similar and consists of two sets of paramesonephric and mesonephric ducts. In females, the mesonephric ducts regress while the paramesonephric ducts fuse at their distal end to yield the uterus, cervix, and upper two-thirds of the vagina; and persist uncombined near its proximal part to generate the fallopian tubes. By the 12th week, the dividing septum had receded, exposing the uterine cavity [12]. Once the müllerian ducts fail to merge, the uterine horns, cervices, and endometrial cavities exist separately [12].
In 1981, Müllerian duct abnormalities were classified under three categories, agenesis/hypoplasia; defects of vertical fusion; defects of lateral fusion [13]. Herlyn Werner Wunderlich syndrome represents a failure of lateral and vertical fusion [9]. The etiology is unclear, but environmental and genetic factors may influence embryogenesis [3].
Uterus didelphys is a rare müllerian ducts anomaly developed in 5–7% of all cases [12]. Studies revealed that in 75% of cases, either a vertical or transverse vaginal septum exists [12], whereas another study has reported a 100% prevalence of a vertical septum [4]. In our case, the uterus didelphys is associated with a transverse vaginal septum.
Paramesonephric duct anomalies are usually associated with upper urinary tract defects; regarding the adjacent origin of both the mesonephric and paramesonephric ducts [9,12]. Renal abnormalities are twice as frequent on the right side as they are on the left. However, renal agenesis is the most frequent anomaly [8,12]. Horseshoe kidney, pelvic kidney, multicystic renal dysplasia, and ectopic ureters are uncommon [8]. A review of 49 patients reported renal anomalies in 10 patients; eight patients had renal agenesis with ipsilateral obstructed hemivagina; one patient had bilateral malrotated kidneys with complete obstructed hemivagina; one patient had lobulation of the kidney [4]. Only one study reported a patient who had bilateral kidneys in their normal position [14]. The ovaries and fallopian tubes have a distinct developmental process; therefore, their disorders are discrete from müllerian duct defects [12].
Most patients present during puberty on months up to one year after menarche [3,5]. Studies have shown that the mean age of menarche was 12.5 years [4], and the mean age of diagnosis is 14.5 years [7]. Therefore, many factors may postpone the accurate diagnosis; the patient has regular menstrual periods from the unobstructed horn; because this is a rare disorder, the physician would not include it in his differential diagnoses; the physician will usually prescribe an anti-inflammatory medication to alleviate the patient's symptoms. All of these factors have a role in our delayed diagnosis of Herlyn-Werner-Wunderlich syndrome [7].
The most frequent symptoms are periodical abdominal pain, dysmenorrhea, and pelvic mass subsequently due to the obstructed hemivagina [3,5]. A review of 49 patients reported that obstructed hemivagina was observed in nine (18%) patients, of which six had a total obstruction resulting in hematocolpos. The symptoms of complete obstruction were abdominal mass, lower abdominal pain, and dysmenorrhea, similar to our patient's. In contrast, incomplete obstruction exhibits intermittent mucopurulent discharge [4]. These data revealed that the obstructed hemivagina was associated with a didelphic uterus in 18% of cases and obstructed hemivagina and didelphic uterus report a 100% prevalence of renal agenesis to correlate to the side of obstruction [4], as in our case as well. Moreover, dysmenorrhea was the most frequent symptom and has arisen in 30 patients (71%) [4].
We used the US and CT scan as they can confirm the diagnosis [1,8]. Ultrasound detects uterus didelphys, hematocolpos, hematometrocolpos, and renal agenesis but cannot identify the vaginal septum and the type of müllerian defect [5]. The MRI is more convenient for a thorough assessment [5], but it is a high-priced diagnostic method [7]. Therefore, ultrasound may be sufficient to establish the correct diagnosis and begin treatment [9].
The cornerstone of management is to resect the vaginal septum and drain the hematocolpos via a vaginoplasty [5,7]. Scalpel, retractors, and sutures might be helpful during the surgery. Pervading fluid permits for thorough visualization of the obstructed vagina and the contralateral patent cervix. It is feasible to conduct resection while keeping the hymen intact. Some patients may have adhesions, abscesses, or endometriosis; endometriosis among these patients is related to retrograde menstruation [7,8]. The complications related to the procedure include bladder or rectum injury [7].
Among 45 patients who had undergone laparoscopy or laparotomy, seven had endometrioses. Endometriosis was spread on the pelvic serosa in four patients and located on the ovary in three, resulting in adhesions [4]. Furthermore, few cases have reported acute urinary retention and hydronephrosis as late complications for Herlyn Werner Wunderlich syndrome [15,16].
Patients with a didelphic uterus may have concerns about their fertility and pregnancy [4]. Data have shown that 34 (94%) out of 36 women who wanted to conceive had at least one pregnancy and 32 (89%) of them had at least one living infant. However, preterm delivery, spontaneous abortion, and Cesarean section are prevalent among these patients [4].
3. Conclusion
Diagnosis and management of Herlyn-Werner-Wunderlich syndrome are very challenging in low-income countries. Although MRI is the gold standard for establishing the diagnosis and preoperative planning, ultrasound and CT scan can be an alternative, less expensive, and reliable approach. They reveal the three elements of this syndrome (didelphic uterus; hemivaginal septum; unilateral renal agenesis). In addition, Laparoscopy or vaginoscopy may not be available in these countries. Therefore, correcting the anomalies can be achieved with laparotomy, which results in acceptable outcomes without any complications. Declarations.
Conflicts of interest
The authors declared that they have no conflict of interest.
Sources of funding
No funding is required.
Ethical approval
Ethical approval was not required.
Consent
Written informed consent was obtained from the patient's parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
SJ collected the patient's data. SJ, KT, and FR drafted the manuscript. NT and EA performed the procedure and revised the manuscript.
Registration of research studies
This is not an original research project involving human participants in an interventional or an observational study but a case report. This registration was not required.
Declaration of competing interest
The authors have no conflict of interest.
Acknowledgement
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102843.
Contributor Information
Sami Jomaa, Email: sami.jomaa1997@gmail.com.
Kenana Tawashi, Email: tawashikenana@gmail.com.
Fatima Alzhraa All Rass, Email: fatimahalzhraa6@gmail.com.
Eyad Abdallah, Email: eyad.abd.allah93@gmail.com.
Nazih Tawashi, Email: tawashnazih@gmail.com.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Grantor
Sami Jomaa.
Ethical approval
No ethical approval was required.
Sources of funding
No funding was required.
Author contribution
Sami Jomaa collected the patient's data. Sami Jomaa, Kenana Tawashi, and Fatima Alzhraa All Rass drafted the manuscript. Nazih Tawashi, and Eyad Abdallah performed the procedure and revised the manuscript.
Registry
Name of the registry:
Unique Identifying number or registration ID:
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Angotti R., Molinaro F., Bulotta A.L., Bindi E., Cerchia E., Sica M., Messina M. Herlyn-Werner-Wunderlich syndrome: an "early" onset case report and review of Literature. Int J Surg Case Rep. 2015;11:59–63. doi: 10.1016/j.ijscr.2015.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Purslow C.E. A case of unilateral hæmatokolpos, hæmatometra and hæmatosalpinx, BJOG. An International Journal of Obstetrics & Gynaecology. 1922;29(4) 643-643. [Google Scholar]
- 3.Nishu D.S., Uddin M.M., Akter K., Akter S., Sarmin M., Begum S. Herlyn-Werner-Wunderlich syndrome presenting with dysmenorrhea: a case report. J. Med. Case Rep. 2019;13(1):323. doi: 10.1186/s13256-019-2258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heinonen P.K. Clinical implications of the didelphic uterus: long-term follow-up of 49 cases. Eur. J. Obstet. Gynecol. Reprod. Biol. 2000;91(2):183–190. doi: 10.1016/s0301-2115(99)00259-6. [DOI] [PubMed] [Google Scholar]
- 5.Gungor Ugurlucan F., Dural O., Yasa C., Kirpinar G., Akhan S.E. Diagnosis, management, and outcome of obstructed hemivagina and ipsilateral renal agenesis (OHVIRA syndrome): is there a correlation between MRI findings and outcome? Clin. Imag. 2020;59(2):172–178. doi: 10.1016/j.clinimag.2019.11.013. [DOI] [PubMed] [Google Scholar]
- 6.Jomaa S., Ahmad A., Adwan D. Successful diagnosis and management of prerupture rudimentary horn pregnancy in the second trimester: a case report. Radiol Case Rep. 2021;16(10):3068–3071. doi: 10.1016/j.radcr.2021.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zurawin R.K., Dietrich J.E., Heard M.J., Edwards C.L. Didelphic uterus and obstructed hemivagina with renal agenesis: case report and review of the literature. J. Pediatr. Adolesc. Gynecol. 2004;17(2):137–141. doi: 10.1016/j.jpag.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 8.Aveiro A.C., Miranda V., Cabral A.J., Nunes S., Paulo F., Freitas C. Herlyn-Werner-Wunderlich syndrome: a rare cause of pelvic pain in adolescent girls. BMJ Case Rep. 2011;2011 doi: 10.1136/bcr.04.2011.4147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gholoum S., Puligandla P.S., Hui T., Su W., Quiros E., Laberge J.M. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome) J. Pediatr. Surg. 2006;41(5):987–992. doi: 10.1016/j.jpedsurg.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 10.Boyraz G., Karalok A., Turan T., Özgül N. Herlyn-Werner-Wunderlich Syndrome; laparoscopic treatment of obstructing longitudinal vaginal septum in patients with hematocolpos - a different technique for virgin patients. J. Turk. Ger. Gynecol. Assoc. 2020;21(4):303–304. doi: 10.4274/jtgga.galenos.2019.2019.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Miguel D., Pagano D., Millham F.H., Roy G., Kadioglu H., Nixon I.J., Mukhejree I., McCaul J.A., Chi-Yong Ngu J., Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., De Wilde R.L., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Karanth V.K.L., Kasivisvanathan V., Mei Z. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 12.Troiano R.N. Magnetic resonance imaging of mullerian duct anomalies of the uterus. Top. Magn. Reson. Imag. 2003;14(4):269–279. doi: 10.1097/00002142-200308000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Acién P., Acién M.I. The history of female genital tract malformation classifications and proposal of an updated system. Hum. Reprod. Update. 2011;17(5):693–705. doi: 10.1093/humupd/dmr021. [DOI] [PubMed] [Google Scholar]
- 14.Pinsonneault O., Goldstein D.P. Obstructing malformations of the uterus and vagina. Fertil. Steril. 1985;44(2):241–247. [PubMed] [Google Scholar]
- 15.Mandava A., Prabhakar R.R., Smitha S. OHVIRA syndrome (obstructed hemivagina and ipsilateral renal anomaly) with uterus didelphys, an unusual presentation. J. Pediatr. Adolesc. Gynecol. 2012;25(2):e23–e25. doi: 10.1016/j.jpag.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Selter J.H., Christianson M.S., Washington C.I., Resetkova N., Kolp L., Hydronephrosis A rare presentation of uterine didelphys with obstructed hemivagina and ipsilateral renal anomaly. J. Pediatr. Adolesc. Gynecol. 2016;29(3):e53–e55. doi: 10.1016/j.jpag.2015.12.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.