Abstract
The COVID-19 pandemic has rapidly emerged as one of the biggest public health concerns of the 21st century. Although it was initially reported as a cluster of pneumonia cases, it quickly became apparent that COVID-19 is not merely a respiratory tract infection. Its clinical course is often complicated by cardiovascular manifestations including venous and arterial thrombosis, electrical disturbances, and myocardial damage. In addition, the cardiovascular system is involved not only during infection but also preceding the contraction of the virus; having cardiovascular comorbidities indicates significant vulnerability to the pathogen. As longer-term data continue to accumulate, we now have concerns over its lasting cardiovascular effects after recovery. Moreover, there have been substantial collateral effects on the epidemiology of cardiovascular diseases. Reports of adverse cardiovascular events from vaccination have emerged as new hurdles to our efforts to bring an end to the pandemic. As such, the association between COVID-19 and the cardiovascular system and cardiovascular practice in general is expansive. In this review, we provide an overview of the knowledge and considerations in this field, based on the evidence available at the time of this writing.
Keywords: COVID-19, Venous thrombosis, Myocardial infarction, Arrhythmia, Myocarditis
Graphic abstract Effects of COVID-19 on the Cardiovascular System and Practice
Graphic abstract
Effects of COVID-19 on the Cardiovascular System and Practice
Introduction
Since the first case was identified in Wuhan, China in December 2019, coronavirus 2019 (COVID-19) has rapidly spread across the globe, representing the largest pandemic humanity has faced since the Spanish flu a century ago. As of September 2021, there have been at least 218 million confirmed cases of COVID-19 worldwide [1]. Approximately 2.8% of the world's population have been infected. Besides posing direct health consequences to the patients, COVID-19 has influenced our daily lives, leading to unforeseen secondary effects both within and outside healthcare.
The bidirectional relationship between infectious diseases and the cardiovascular system has been well established in previous literature. However, we have come to realize that our current understanding is insufficient to effectively manage severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. In addition, the pandemic has resulted in secondary effects to cardiovascular practice. As COVID-19 becomes more common in daily clinical practice, every cardiovascular professional must keep up to date with the latest findings in this broad field. Here in this review, we will summarize potential cardiovascular problems in each phase of illness: preceding contraction of the virus, during acute infection, and after recovery. In addition, we will broaden our scope outside of COVID-19 infection itself to collateral consequences of the pandemic, touching briefly on the vaccines as well. In each of the topics, we will focus on the cardiovascular aspects and summarize what has been made clear and what needs further investigation.
Role of cardiovascular comorbidities on the clinical course
Pre-existing cardiovascular disease, along with older age and other non-cardiovascular comorbidities, is an established risk for adverse outcomes in COVID-19 patients. An early prospective cohort study of 5279 infected people in New York revealed that patients with cardiovascular disease were more likely to take a severe clinical course. Heart failure was one of the most substantial risks for critical illness (odds ratio 1.9, CI 1.4 to 2.5) [2]. Also, in a multicenter cohort study from the UK of 20,133 inpatients, chronic cardiac disease was the most prevalent comorbidity and was associated with mortality [3]. Similar findings have been reported from many other regions of the world [4], [5], [6], [7]. More recently, a large meta-analysis that included 51 studies with a total of 48,317 patients suggested that the increased risk is consistent across all ages [8]. Although younger patients had a lower prevalence of cardiovascular diseases, they were at a higher risk for morbidity from COVID-19 compared to elderly patients with similar conditions.
Although evidence on severe illness in COVID-19 patients with cardiovascular comorbidities is abundant, many of these early studies did not distinguish between different heart conditions. According to data currently available, heart failure, although the term itself incorporates a broad spectrum of etiologies and severity, appears to pose the highest risk. Surprisingly, based on an analysis of a large, multicenter database of 8383 American COVID-19 patients with heart failure, nearly one in four died during hospitalization [9]. In a large multi-national cohort study of 20,954 patients, the adjusted risk ratio for in-hospital mortality was 1.19 for heart failure and 1.41 for severe (i.e. New York Heart Association III/IV) heart failure [10]. Of note, after adjustment for age, sex, body mass index, diabetes, hypertension, chronic kidney disease, and chronic obstructive pulmonary disease, the increased risk was not significant for other heart disease subtypes, including ischemic heart disease, arrhythmias, and valvular heart diseases. Further studies to determine the association across different heart disease subtypes are warranted.
Given the profound influence that cardiovascular comorbidities have on the clinical trajectory of COVID-19, a thorough review of the patient's medical history must be conducted. By doing so, the risk for progressive disease would be better estimated, which would in turn enable timely escalation of therapeutic interventions. Also, efforts to encourage patients with cardiac comorbidities to get vaccinated must be continued. In areas of the world where vaccines are in short supply, priority needs be determined based on different cardiovascular conditions and their severity [11].
Cardiovascular complications during acute infection
In the wake of the pandemic in Wuhan, China, SARS-CoV-2 infections were reported as a cluster of pneumonia cases, mainly affecting the lungs. However, it quickly became evident that the infection has far-reaching effects on other parts of the body as well. Since then, both basic and clinical researchers have re-explored the close connection between the immune system and the cardiovascular system [12].
Previous investigations have suggested that various types of cardiovascular complications may occur in COVID-19 patients. According to a meta-analysis of 17 cohort studies with a total of 5815 patients, the most common cardiovascular complications were heart failure, myocardial injury, cardiac arrhythmia, and acute coronary syndrome [13].
The true incidence for each complication is difficult to estimate. There is significant heterogeneity in disease severity and treatment among various studies. Therefore, it is a matter of ongoing debate which, if any, cardiovascular complications are particularly frequent in COVID-19 compared to other types of infections. Interestingly, a recent multi-national cohort study of 16,511 patients pointed out that besides pulmonary embolism, serious cardiac complications including myocarditis, myocardial infarction, and new-onset heart failure were rare, occurring in only 2.0% of hospitalized patients [10] (Table 1 ).
Table 1.
Prevalence and Mechanism of Cardiovascular Complications Caused by COVID-19.
| Prevalence | Common mechanism | COVID-specific mechanism | |
|---|---|---|---|
| Venous Thrombosis Pulmonary Embolism |
High | • Immunothrombosis • Reduced mobility • Hypoxia |
• Endothelial damage • Prominent NET formation |
| Myocardial Infarction | Low | • Immunothrombosis | • Prominent NET formation |
| Arrhythmia | Intermediate | • Inflammatory electrophysiological disturbance • Sympathetic activation • Volume / electrolyte imbalance |
Unlikely |
| Myocardial Injury | High | • O2 supply-demand ischemia | Unlikely |
| Myocarditis Endocarditis Pericarditis | Low | Insufficient data | Insufficient data |
NET, neutrophil extracellular trap.
Venous thrombosis and pulmonary embolism
The presence of venous thrombosis in COVID-19 patients is common, particularly in those with a critical illness [14], [15], [16]. According to a recent systematic review of 16 studies, the estimated incidence of venous thromboembolism was 7.4% [17]. Another systematic review analyzed 27 studies and concluded that the pooled incidence rate was 16.5% [18]. This large deviation demonstrates the presence of substantial heterogeneity among various studies. Contributing factors may include differences in the study population (e.g. disease severity and patient demographics) and clinical practices [e.g. anticoagulation prophylaxis and accessibility of computed tomography pulmonary angiography (CTPA) testing].
The development of venous thrombosis in COVID-19 patients probably involves etiologies familiar to other respiratory infections, such as hypoxia and reduced mobility [19,20]. However, the incidence of venous thrombosis is significantly higher in COVID-19 compared to seasonal influenza, suggesting that mechanisms exclusive to COVID-19 may also be present [21]. Here, the angiotensin-converting enzyme 2 (ACE2) receptor may play a unique role in the process. Via the ACE2 receptor, the SARS-CoV-2 virus enters the vascular endothelium, triggering endothelial inflammation and the exposure of von Willebrand factor (vWF) [22], [23], [24]. vWF plays a role in adhesion and aggregation of platelets and contributes to thrombosis [25]. In addition, neutrophils, which also express ACE2 receptors, are activated by the virus and release neutrophil extracellular traps (NETs) [12]. NETs are key mediators of immunothrombosis that activate factor XII and trigger the coagulation cascade [26]. In fact, studies on blood neutrophils and lung specimens of COVID-19 patients have suggested that prominent NET formation was a distinguishing feature in COVID-19 [27,28].
The establishment of an optimal anticoagulation strategy to prevent thrombotic complications continues to be a work in progress. During the early days of the pandemic, clinicians experimentally began administering prophylactic anticoagulation to COVID-19 patients upon hospital admission. Meanwhile, a retrospective analysis of 449 severe COVID-19 patients in China showed that anticoagulant therapy with low molecular weight heparin (LMWH) was associated with a better prognosis [29]. Following this trend, several academic institutions recommended routine prophylactic anticoagulation with LMWH in all hospitalized COVID-19 patients without contraindications [30,31]. The strategy was later justified by a large nationwide cohort study of 4297 COVID-19 patients in the USA [32]. The research revealed that early prophylactic administration of heparin was associated with a 34% increased chance of survival without an increased risk of serious bleeding. Still, even with the routine administration of prophylactic-dose anticoagulation, venous thrombosis remained a major question [33]. Whether higher doses of anticoagulation prophylaxis would be more effective and still be safe remained a mystery among clinicians.
The most recent randomized clinical trials (RCT) hint against routine therapeutic-dose anticoagulation. The INSPIRATION RCT compared the effects of intermediate-dose and standard-dose prophylactic anticoagulation in 562 COVID-19 patients treated in the intensive care unit (ICU) [34]. The trial revealed that intermediate-dose anticoagulation showed no improvement in the composite outcome of thrombosis, extracorporeal membrane oxygenation (ECMO) treatment, or mortality. Instead, it resulted in more bleeding. Similar findings came from the ACTION RCT, where 615 COVID-19 patients with elevated D-dimer were randomized to receive either therapeutic-dose or prophylactic-dose anticoagulation [35]. The study also failed to show improvement in clinical outcomes with therapeutic-dose anticoagulation. Again, therapeutic-dose anticoagulation was associated with a significant increase in bleeding compared to prophylactic-dose. In contrast to the two RCTs, the REMAP-CAP, ACTIV-4a, and ATTACC multi-platform RCT suggested that benefits of therapeutic-dose anticoagulation might depend on disease severity [36,37]. The study suggested that therapeutic-dose anticoagulation improved survival rate in the noncritically ill patients but not in critically ill patients. Within the noncritically ill patients, although therapeutic-dose anticoagulation improved outcomes regardless of the patient's D-dimer level at baseline, the benefit was more prominent in those with high D-dimer levels. Altogether, the three RCTs have reemphasized that individualized adjustments based on disease severity, D-dimer levels, and bleeding risks are crucial.
In addition, the development of a diagnostic algorithm for pulmonary embolism (PE) in COVID-19 patients also continues to be a work in progress. In particular, the appropriate D-dimer threshold for selecting patients for CTPA is still controversial. CTPA is the golden diagnostic standard for PE in general. However, it is often overused, leading to unnecessary risks of radiation exposure and contrast nephropathy [38]. In the case of COVID-19, it also poses the risk of viral transmission to the medical staff. Some studies argue that the conventionally used cut-off value (500 or 1000 ng/mL) is too low, while others argue that setting a higher cut-off value would reduce the sensitivity of the test [18,39,40]. To further complicate the problem, the efficacy of pre-test prediction scores such as the Well criteria has been questioned in COVID-19 patients [41,42]. Given the high prevalence of PE, it may be reasonable to maintain a low threshold for conducting CTPA until reliable evidence becomes available.
Myocardial infarction
Since the early phases of the pandemic, multiple cohort studies have shown that COVID-19 might trigger acute myocardial infarction (AMI) [15,43]. In addition to cohort studies, the self-controlled case series (SCCS) method has been used to evaluate the risk of AMI associated with COVID-19. An SCCS compares incidence rates of an outcome (i.e. AMI) relative to an exposure (i.e. COVID-19) in one person at different time periods. Using the method, a Danish study of 5119 patients diagnosed with COVID-19 estimated that the incidence rate of AMI was five times higher during the 14 days after COVID-19 diagnosis [44]. In a recent nationwide study from Sweden that analyzed 86742 patient records, the incidence rate ratio for AMI was 2.9 for the first week following COVID-19 onset, compared with control intervals [45]. The researchers simultaneously conducted a matched cohort study to compare the risk with the background population. Compared to matched controls, COVID-19 patients had an odds ratio of 3.4 for the two weeks following COVID-19. The studies have confirmed that COVID-19 patients are at an increased risk for AMI, particularly within the first two weeks of onset.
The detailed mechanism of AMI onset in COVID-19 is unclear. Infections and subsequent inflammation may trigger coronary thrombosis through multiple mechanisms, including inflammatory cell infiltration into the atherosclerotic plaques, systemic platelet activation, coronary vasoconstriction, and endothelial dysfunction [46]. Indeed, it has been validated in previous literature that acute respiratory infections in general increase the risk of acute coronary syndromes [47], [48], [49]. According to a meta-analysis of 16 case-control studies, recent respiratory tract infection, including influenza, was significantly associated with AMI [50]. In COVID-19 patients, NET formation may also be playing a specific role. A small case series study compared the coronary thrombus aspirates of 5 AMI patients with COVID-19 and 50 control patients without COVID-19 [51]. NETs were detected in all COVID-19 patients, whereas in the control group, only 68% were positive. The median density of NETs was significantly higher in COVID-19 patients as well (61% vs. 19%).
The treatment algorithm of AMI for COVID-19 patients is the same as that for non-COVID-19 patients [52]. For suspected ST-elevation myocardial infarction, the patient should undergo emergent coronary angiography (CAG) plus an ad-hoc percutaneous intervention if the diagnosis is confirmed. One thing to keep in mind though, is the need to limit exposure with the patient. Unless the patient is proven COVID-19-negative, emergent CAG procedures should be conducted with minimal staff members with proper personal protective equipment.
COVID-19-triggered AMI in individuals with high coronary risks may become a public health concern in the coming days. Interestingly, authors of the meta-analysis mentioned above also analyzed the benefits of influenza vaccination in preventing AMI and estimated that the effectiveness of flu vaccines in AMI prevention was 29%, comparable to that of other preventative measures such as statins (36%) and antihypertensives (15-18%) [50]. The merits of vaccination go beyond preventing the original viral infection to its possible cardiovascular complications.
Arrhythmia
A wide variety of arrhythmias are reported in the acute phase of COVID-19. In a global survey of electrophysiology professionals, atrial fibrillation was the most common arrhythmia, reported by 142 out of 683 respondents (21%) [53]. On the other hand, life-threatening arrhythmias were rarely reported. For instance, malignant ventricular tachycardia and ventricular fibrillation were reported by only 4.8% of respondents. In a worldwide case series of 4526 COVID-19 patients, 18% had an arrhythmia during hospitalization, most of which were newly discovered [54]. Of those who developed an arrhythmia, the incidence of atrial tachycardia was 81.8%, and the incidence of ventricular tachycardia was 20.7%. Drug-induced QT prolongation and Torsade de Pointes once used to be a clinical issue in the early days of the pandemic when hydroxychloroquine and azithromycin were experimentally used as COVID-19 treatment [55]. With solid evidence against their effectiveness, these drugs are no longer recommended. As such, the initial retrospective studies may have overestimated the actual burden of arrhythmias in COVID-19 patients, especially for ventricular tachycardias.
Although the pathophysiology of arrhythmias in COVID-19 patients remains uncertain, it is likely precipitated by systemic immunoinflammatory response. Inflammatory cytokines prolong the action potential duration (APD) of the myocardium, hence a prolonged QT interval on electrocardiogram. Combined with sympathetic activation, they may trigger ventricular arrhythmias. Also, the cytokines also induce delayed after depolarizations (DADs), increasing the frequency of ectopic activities and subsequent atrial arrhythmias [56], [57], [58]. Other underlying factors may include electrolyte disturbances and intravascular volume imbalances in severely ill COVID-19 patients.
Based on such assumptions, it is no surprise that the frequency of arrhythmia is associated with disease severity. In the aforementioned case series study, 43% of patients who developed arrhythmias were mechanically ventilated [54]. Furthermore, an analysis of 700 COVID-19 patients showed that patients treated in the ICU were 10 times more likely to develop atrial fibrillation, bradycardia, or non-sustained ventricular tachycardia compared to those in the general ward [59]. Myocardial injury, an indicator of poor prognosis, was also associated with malignant arrhythmias in patients receiving intensive care [60].
Management of arrhythmias does not differ significantly in the context of COVID-19 infection and should be based on evidence-based guidelines. For instance, in the case of atrial fibrillation, treatment should address rate control, rhythm control, and anticoagulation.
Other complications
Other reported cardiovascular complications of COVID-19 include heart failure, endocarditis, pericarditis, and myocarditis. The definition of heart failure is often ambiguous and inconsistent among studies, making it difficult to determine its significance in COVID-19 patients. According to a large multi-national cohort study of 20954 patients, new-onset heart failure occurred in only 1.2%, more frequently in patients with pre-existing heart conditions [10]. Reports of endocarditis and pericarditis are limited to case reports [61,62]. Although myocardial injury is a common finding in COVID-19 patients, other clinical features of myocarditis, such as electrocardiographic and echocardiographic abnormalities, are relatively rare [17,63].
Myocardial injury and cardiovascular biomarkers
In the context of COVID-19, myocardial injury usually refers to the elevation of cardiac troponin regardless of its etiology. Previous studies have shown that it is a common finding in COVID-19 patients. The reported incidence of elevated troponin varies widely, from 4.8% in patients with only mild symptoms to 54% in critically ill patients [17].
The level of troponin is shown to be closely related to disease severity and mortality of COVID-19. In an initial report from China, myocardial injury was more prevalent among ICU patients compared to non-ICU patients (22.2% vs. 2.0%) [64]. Furthermore, troponin elevation was not only associated with mortality but also with a greater risk of non-cardiovascular complications such as sepsis, acute kidney failure, and major bleeding [65]. Another multicenter study reported that although troponin-I was only mildly elevated (e.g. <0.03-0.09 ng/ml) in a majority of patients, even subtle elevations were significantly associated with mortality [66]. Surprisingly, patients exhibiting myocardial injury without prior cardiovascular disease had worse outcomes compared to those with a history of cardiovascular disease, but no myocardial injury [60].
The association between myocardial injury and critical illness is not unique to COVID-19; It has been previously demonstrated in other infections, including community-acquired pneumonia and seasonal influenza [67,68]. In a retrospective cohort study of 321 hospitalized patients with H7N9 influenza, 45.8% showed elevated troponin, and myocardial injury was associated with in-hospital mortality [68]. Moreover, troponin has been proposed as a prognostic marker for critically ill patients with early sepsis [69] and other acute respiratory diseases [70].
Myocardial injury in COVID-19 is usually a result of supply-demand ischemia from immune-mediated systemic inflammation. Some studies suspect myocardial damage caused by direct invasion of SARS-CoV-2, but this notion lacks quality evidence. Several in vitro studies have supported that human iPS-derived cardiomyocytes are susceptible to direct infection by SARS-COV-2 [71,72]. On the contrary, in histopathological analysis of 39 autopsy cases of COVID-19 patients, a high viral load of SARS-CoV-2 in the cardiac tissue was present in 16 (41%) patients, but it was detected in the interstitial cells rather than the cardiomyocytes [73]. Furthermore, none of them had concomitant infiltrates of inflammatory cells.
Other parameters routinely used in daily cardiovascular practice may also be effective in predicting prognosis. One of such biomarkers is D-dimer. In an early study of 191 Chinese patients with COVID-19, D-dimer greater than 1 μg/mL was associated with increased in-hospital mortality [74]. Of note, levels of D-dimer and cardiac troponin rose progressively in non-survivors as the condition deteriorated, while these values stayed around the normal range in survivors. N-terminal prohormone of brain natriuretic peptide (NT-proBNP) is another biomarker that is under investigation. In a large cohort study of 3080 patients in Spain, NT-proBNP was independently associated with mortality even after adjusting for relevant confounders, including chronic heart failure and acute decompensated heart failure during hospitalization [75].
Routine examination of these biomarkers as a prognostic marker in COVID-19 patients is controversial, as it may result in over-testing. In the case of cardiac troponin, other than relative ischemia from oxygen supply-demand imbalance from severe inflammatory response, its elevation may also involve other mechanisms such as acute coronary syndrome, pre-existing heart disease, renal impairment, and various cardiomyopathies. As such, biomarker tests are often difficult to interpret in clinical practice, requiring comprehensive review of the patient with physical examinations and other diagnostic tools. If biomarker tests are to be conducted for prognosis prediction, pre-test assessment of the patient's broader clinical picture is essential to avoid being misled by the result.
Long-term cardiovascular consequences
Patients who have successfully recovered from COVID-19 may experience persistent symptoms after the infection. The complications of COVID-19 in the chronic phase are referred to as “long COVID syndrome” and have been a focus of research. According to a study of 179 individuals who recovered from COVID-19, 87.4% reported persistence of at least one symptom on a standardized questionnaire [76]. The most frequent manifestations were fatigue (53%), dyspnea (43%), arthralgia (27%), and chest pain (21%).
Within the scope of cardiology, ongoing myocardial inflammation is an area of an emerging issue. According to a large cohort study of 1597 young athletes with prior COVID-19 infection, 2.3% were suspected of having myocarditis on cardiovascular magnetic resonance (CMR) imaging, although only 0.31% were symptomatic [77]. Other imaging studies have also suggested an ongoing myocardial inflammation months after the acute infection. In one cohort study, 100 individuals who recovered from COVID-19 were scanned with CMR imaging approximately two to three months after infection [78]. Up to 78% showed abnormal T1 and/or T2 findings, and this finding was independent of pre-existing cardiac conditions or the clinical severity of COVID-19 infection. In another cohort study of 148 COVID-19 recovered patients who were troponin-positive during admission, 26% exhibited myocarditis-like pattern on CMR imaging, and a third of those showed signs of ongoing inflammation [79]. In the two studies, left ventricular ejection fraction was preserved or only mildly reduced. However, a recent study suggested that left ventricular global longitudinal strain (LVGLS), a more sensitive marker of subclinical myocardial dysfunction, might be reduced even in patients who were only mildly ill [80].
Previous studies have suggested that the after-effects of infection are not unique to COVID-19. For instance, in patients with community-acquired pneumonia, the resolution of symptoms require more than a month [81]. However, symptoms aside, they may also be at an increased risk for cardiovascular diseases 10 years after recovery [82]. Further studies with more extended follow-up periods are critical to determine whether outpatient monitoring should be continued in the convalescent phase of COVID-19.
Secondary effects on cardiovascular practice
Epidemiological changes to cardiovascular diseases
The ongoing pandemic has altered people's lifestyles and attitudes toward healthcare, affecting the distribution and presentation patterns of all types of disorders [83,84]. Cardiovascular diseases are no exception. The epidemiology of acute cardiovascular diseases was drastically affected particularly in the first wave of the pandemic when strict social distancing measures were implemented in many countries.
It appears that patients with acute cardiovascular events have been unable to or have hesitated to seek medical help during waves of the pandemic. In a nationwide retrospective study from Austria, following the outbreak at the beginning of March 2020, there was a 39.4% reduction in admissions for acute coronary syndromes [85]. Similar findings have been observed in the UK, Italy, and the USA [86], [87], [88]. In contrast, other studies have revealed that overall cardiovascular deaths increased despite the reduction in hospital presentations. In New York, deaths caused by ischemic heart disease from January to June 2020 were 2.39 times that of the same period in 2019 [89]. According to a large study using national statistics data of all adult deaths in the UK, the pandemic caused an excess acute cardiovascular mortality of 2085 (+8%), mostly occurring at home [90]. Another study from the UK confirmed that thromboembolic deaths increased outside the hospitals despite a decrease in in-hospital deaths [91]. These observed increases in out-of-hospital mortality from acute cardiovascular events may be due to 1. fear of catching the virus during hospital visits, and 2. overwhelmed healthcare system in the initial phase of the pandemic.
Lifestyle alterations, especially sedentary behavior, may also result in epidemiological changes to cardiovascular conditions. The importance of physical activity is well documented in all kinds of cardiovascular conditions [92]. Amidst the pandemic, acute venous thromboembolism (VTE i.e. PE and deep venous thrombosis) in the non-COVID-19 population is particularly concerning. A multi-center Chinese study of 3358 VTE patients compared the population before and during the pandemic and evaluated changes in VTE risk factors. Compared to the control period, proportion of trauma and surgery-induced VTE was lower during the pandemic period, whereas the proportion of VTE from inactivity was significantly higher during the pandemic period (30.7% vs. 22.6%) [93]. Similar observations were seen in other areas with different COVID-19 containment policies [91,94,95].
Stringent social distancing measures, such as lockdowns and stay-at-home orders, are still necessary in many parts of the world where vaccination distribution is inadequate. However, physical inactivity leads to development and progression of multiple cardiovascular conditions. It also increases the infection risk of COVID-19 and is associated with severe outcomes [96,97]. Especially when such policies are being implemented, emphasizing the risk of sedentary lifestyles, and promoting regular exercise is crucial.
Changes to outpatient cardiovascular care
The long-term consequences of changes in patient behavior are of growing concern [98]. First, patients with chronic cardiovascular conditions have avoided medical care visits during the pandemic [99]. Close outpatient follow-up enables optimal cardiovascular risk factor control through timely prescription adjustments and is associated with an improved prognosis of cardiovascular diseases [100,101]. The shift away from regular in-person visits poses a great risk to continuity of care. Second, fewer health checkups and testing are conducted, resulting in delays in diagnoses and interventions [84]. The importance of appropriate healthcare visits must be more widely recognized by the public.
Some clinicians see the pandemic not as a public health crisis but rather as a chance for digital transformation in healthcare. As an example, information and communication technology (ICT) has been promoted in cardiovascular outpatient care to avoid direct patient-physician contact [102]. However, as some people are unfamiliar with newer technologies, accessibility issues need to be resolved. A study conducted during the pandemic analyzed the demographics of 2940 patients with cardiovascular conditions who were scheduled for a telemedicine encounter [103]. Those who completed video telemedicine visits were significantly more likely to be male and had higher incomes than those who did not use video. The ongoing trend toward ICT-based healthcare will continue, but the issue of digital divide may be the rate-determining step in its widespread use.
Cardiovascular adverse reactions of vaccination
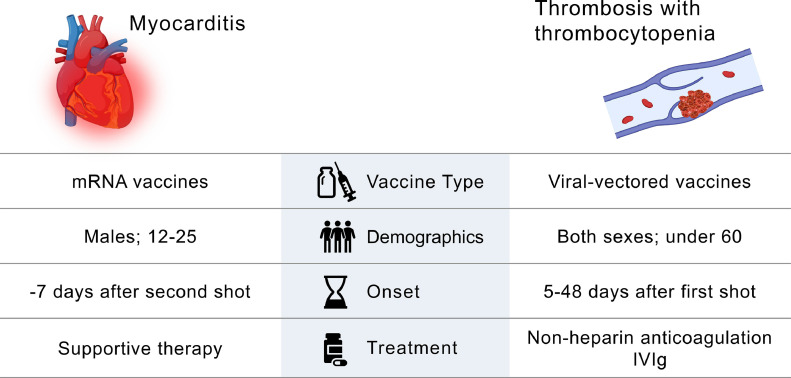
COVID-19 vaccines have been rapidly developed and are being distributed around the globe to tackle the pandemic. Even with increased prevalence of new, potentially more transmissible variants such as Delta, the vaccines continue to offer protection against severe disease [104]. The four vaccines predominantly distributed in the USA and Europe are commonly referred to by the manufacturer name: Pfizer-BioNTech, Moderna, AstraZeneca, and Johnson & Johnson/Janssen. These vaccines adopted fairly new technologies to achieve rapid development and large-scale production [105]. They introduce the genetic information (either mRNA or DNA) of the antigen to the immune system, instead of the antigen itself. Although the incidence is presumably extremely low, cardiovascular side effects of the vaccines are of growing concern: myocarditis and thrombosis (Fig. 1 ).
Fig. 1.
Possible cardiovascular adverse reactions of COVID-19 vaccination.
Cases of acute myocarditis have been reported in individuals who were vaccinated with mRNA vaccines, namely Pfizer-BioNTech and Moderna. According to an analysis based on Centers for Disease Control and Prevention's (CDC) vaccine safety monitoring system, as of June 2021, there have been 1226 reports of myocarditis after vaccination [106]. It occurred most frequently in young males (highest in age range 12–24 years) after the second shot. Ninety-two percent of them manifested within one week, and the median time until onset was two days. The patient typically presented with acute chest pain and substantially elevated troponin levels [107,108]. The clinical course was usually mild and none had died. Although the incidence of this adverse event is still under investigation, the benefits still clearly outweigh the risks. The Advisory Committee on Immunization Practices estimated that even in younger individuals, for every one million second-dose of vaccination, 560 hospitalizations and 138 ICU admissions from COVID-19 might be avoided, compared to only 40 cases of myocarditis [106].
Rare thrombotic events and thrombocytopenia have occurred after first doses of vaccination with viral-vectored vaccines. Vaccine classified in this type are Oxford-AstraZeneca vaccine and Johnson & Johnson/Janssen's single-shot vaccine. Some refer to the syndrome as vaccine-induced immune thrombocytopenia and thrombosis (VITT) [109]. In many ways, the reported manifestations resembled heparin-induced thrombocytopenia (HIT). Even though it occurs without exposure to heparin, the patients exhibited positive anti-platelet factor 4 (PF4) antibodies, the very antibodies detected in HIT. According to a recent cohort study of 294 VITT cases, the patients were relatively young (85% were <60 years old) and presented 5 to 48 days after the first dose of vaccination [110]. Overall mortality was 22%, and death occurred more frequently in patients with cerebral venous sinus thrombosis and severe coagulation abnormality. While optimal treatment remains unclear, based on deduction from HIT, intravenous immunoglobulins and/or non-heparin-based anticoagulants are recommended [111,112]. Plasma exchange may also be considered for those with poor responses to initial therapy [113]. As is the case with mRNA vaccines, the World Health Organization (WHO) concluded that benefits of vaccination clearly outweigh the potential risks [112].
Safety monitoring is undoubtedly critical in this global vaccination campaign of an unprecedented scale. However, based on reports thus far, the vaccines' benefits are much greater than their risks. In fact, newest studies have shown that the risks for developing the cardiovascular events (myocarditis and thrombosis) are higher after SARS-CoV-2 infection itself than after vaccination [114,115]. Keeping up with the latest safety guidance from reliable sources such as the CDC and the WHO, rather than the lay press, is critical to enable rational decision-making regarding vaccination.
Conclusion
We have described multiple topics of interest with regards to the close relationship between COVID-19 and the cardiovascular system/practice. We have seen that COVID-19 is associated with cardiovascular disorders in every step of its infection. In addition, we have demonstrated that the pandemic has had significant secondary impacts on cardiovascular care. Due to the fast-moving nature of this field, the recommendations made in this review are subject to change quickly. We must continue to keep a close eye on the latest findings. Accumulation of new knowledge and experience will enable us to emerge stronger from this pandemic.
Declaration of Competing Interest
None.
References
- 1.WHO COVID-19 Dashboard. Available from: https://covid19.who.int/[Accessed: 1st September 2021]
- 2.Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsunaga N, Hayakawa K, Terada M, Ohtsu H, Asai Y, Tsuzuki S, et al. Clinical epidemiology of hospitalized patients with coronavirus disease 2019 (COVID-19) in Japan: Report of the COVID-19 Registry Japan. Clin Infect Dis. 2020:ciaa1470. doi: 10.1093/cid/ciaa1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen J, Qi T, Liu L, Ling Y, Qian Z, Li T, et al. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect. 2020;80:e1–e6. doi: 10.1016/j.jinf.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Souza WM, Buss LF, Candido D da S, Carrera J-P, Li S, Zarebski AE, et al. Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil. Nature Hum Behav. 2020;4:856–865. doi: 10.1038/s41562-020-0928-4. [DOI] [PubMed] [Google Scholar]
- 7.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bae S, Kim SR, Kim M-N, Shim WJ, Park S-M. Impact of cardiovascular disease and risk factors on fatal outcomes in patients with COVID-19 according to age: a systematic review and meta-analysis. Heart. 2021;107:373–380. doi: 10.1136/heartjnl-2020-317901. [DOI] [PubMed] [Google Scholar]
- 9.Bhatt AS, Jering KS, Vaduganathan M, Claggett BL, Cunningham JW, Rosenthal N, et al. Clinical outcomes in patients with heart failure hospitalized with COVID-19. JACC Heart Fail. 2021;9:65–73. doi: 10.1016/j.jchf.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CAPACITY-COVID collaborative consortium and LEOSS Study Group. Linschoten M, Uijl A, Schut A, Jakob CEM, Romão LR, et al. Clinical presentation, disease course and outcome of COVID-19 in hospitalized patients with and without pre-existing cardiac disease – a cohort study across sixteen countries. medRxiv. 2021 doi: 10.1093/eurheartj/ehab656. 2021.03.11.21253106. [DOI] [PubMed] [Google Scholar]
- 11.Driggin E, Maddox TM, Ferdinand KC, Kirkpatrick JN, Ky B, Morris AA, et al. ACC health policy statement on cardiovascular disease considerations for COVID-19 vaccine prioritization. J Am Coll Cardiol. 2021;77:1938–1948. doi: 10.1016/j.jacc.2021.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stark K, Massberg S. Interplay between inflammation and thrombosis in cardiovascular pathology. Nat Rev Cardiol. 2021;18:666–682. doi: 10.1038/s41569-021-00552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kunutsor SK, Laukkanen JA. Cardiovascular complications in COVID-19: a systematic review and meta-analysis. J Infect. 2020;81:e139–e141. doi: 10.1016/j.jinf.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020;324:799. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, et al. Pulmonary embolism in patients with COVID-19. Circulation. 2020;142:184–186. doi: 10.1161/CIRCULATIONAHA.120.047430. [DOI] [PubMed] [Google Scholar]
- 17.Pellicori P, Doolub G, Wong CM, Lee KS, Mangion K, Ahmad M, et al. COVID-19 and its cardiovascular effects: a systematic review of prevalence studies. Cochrane Database Syst Rev. 2021;3 doi: 10.1002/14651858.CD013879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suh YJ, Hong H, Ohana M, Bompard F, Revel M-P, Valle C, et al. Pulmonary embolism and deep vein thrombosis in COVID-19: a systematic review and meta-analysis. Radiology. 2021;298:E70–E80. doi: 10.1148/radiol.2020203557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gupta N, Zhao Y-Y, Evans CE. The stimulation of thrombosis by hypoxia. Thromb Res. 2019;181:77–83. doi: 10.1016/j.thromres.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 20.Pottier P, Hardouin JB, Lejeune S, Jolliet P, Gillet B, Planchon B. Immobilization and the risk of venous thromboembolism. A meta-analysis on epidemiological studies. Thromb Res. 2009;124:468–476. doi: 10.1016/j.thromres.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Piroth L, Cottenet J, Mariet A-S, Bonniaud P, Blot M, Tubert-Bitter P, et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Resp Med. 2021;9:251–259. doi: 10.1016/S2213-2600(20)30527-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruggeri ZM. The role of von Willebrand factor in thrombus formation. Thromb Res. 2007;120(Suppl. 1):S5–S9. doi: 10.1016/j.thromres.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Brühl M-L, Stark K, Steinhart A, Chandraratne S, Konrad I, Lorenz M, et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med. 2012;209:819–835. doi: 10.1084/jem.20112322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Veras FP, Pontelli MC, Silva CM, Toller-Kawahisa JE, de Lima M, Nascimento DC, et al. SARS-CoV-2–triggered neutrophil extracellular traps mediate COVID-19 pathology. J Exp Med. 2020;217 doi: 10.1084/jem.20201129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicolai L, Leunig A, Brambs S, Kaiser R, Joppich M, Hoffknecht M, et al. Vascular neutrophilic inflammation and immunothrombosis distinguish severe COVID-19 from influenza pneumonia. J Thromb Haemost. 2021;19:574–581. doi: 10.1111/jth.15179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moores LK, Tritschler T, Brosnahan S, Carrier M, Collen JF, Doerschug K, et al. Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019. Chest. 2020;158:1143–1163. doi: 10.1016/j.chest.2020.05.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rentsch CT, Beckman JA, Tomlinson L, Gellad WF, Alcorn C, Kidwai-Khan F, et al. Early initiation of prophylactic anticoagulation for prevention of coronavirus disease 2019 mortality in patients admitted to hospital in the United States: cohort study. BMJ. 2021;372:n311. doi: 10.1136/bmj.n311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Llitjos J, Leclerc M, Chochois C, Monsallier J, Ramakers M, Auvray M, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;18:1743–1746. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mazloomzadeh S, Khaleghparast S, Ghadrdoost B, Mousavizadeh M, Baay MR, Noohi F, et al. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit. JAMA. 2021;325:1620. doi: 10.1001/jama.2021.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lopes RD, de Barros E, Silva PGM, Furtado RHM, Macedo AVS, Bronhara B, Damiani LP, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet. 2021;397:2253–2263. doi: 10.1016/S0140-6736(21)01203-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.REMAP-CAP Investigators; ACTIV-4a Investigators; ATTACC Investigators. Goligher EC, Bradbury CA, McVerry BJ, et al. Therapeutic anticoagulation with heparin in critically ill patients with Covid-19. N Engl J Med. 2021;385:777–789. doi: 10.1056/NEJMoa2103417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.ATTACC Investigators; ACTIV-4a Investigators; REMAP-CAP Investigators. Lawler PR, Goligher EC, Berger JS, et al. Therapeutic anticoagulation with heparin in noncritically ill patients with Covid-19. N Engl J Med. 2021;385:790–802. doi: 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kline JA, Garrett JS, Sarmiento EJ, Strachan CC, Courtney DM. Over-testing for suspected pulmonary embolism in American emergency departments. Circ Cardiovasc Qual Outcomes. 2020;13:1–10. doi: 10.1161/CIRCOUTCOMES.119.005753. [DOI] [PubMed] [Google Scholar]
- 39.Korevaar DA, Aydemir I, Minnema MW, Azijli K, Beenen LF, Heijmans J, et al. Routine screening for pulmonary embolism in COVID-19 patients at the emergency department: impact of D-dimer testing followed by CTPA. J Thromb Thrombolysis. 2021 doi: 10.1007/s11239-021-02508-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kwee RM, Adams HJA, Kwee TC. Pulmonary embolism in patients with COVID-19 and value of D-dimer assessment: a meta-analysis. Eur Radiol. 2021;9:1–19. doi: 10.1007/s00330-021-08003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kirsch B, Aziz M, Kumar S, Burke M, Webster T, Immadi A, et al. Wells score to predict pulmonary embolism in patients with coronavirus disease 2019. Am J Med. 2021;134:688–690. doi: 10.1016/j.amjmed.2020.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Silva B, Jorge C, Rigueira J, Rodrigues T, Silverio Antonio P, Morais P, et al. Wells and Geneva decision rules to predict pulmonary embolism: can we use them in Covid-19 patients? EHJ Cardiovasc Imaging. 2021;22 jeab111.009. [Google Scholar]
- 43.Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, et al. ST-segment elevation in patients with covid-19 — a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Modin D, Claggett B, Sindet-Pedersen C, Lassen MCH, Skaarup KG, Jensen JUS, et al. Acute COVID-19 and the incidence of ischemic stroke and acute myocardial infarction. Circulation. 2020;142:2080–2082. doi: 10.1161/CIRCULATIONAHA.120.050809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Katsoularis I, Fonseca-Rodríguez O, Farrington P, Lindmark K, Fors Connolly A-M. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. Lancet. 2021;398:599–607. doi: 10.1016/S0140-6736(21)00896-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Corrales-Medina VF, Madjid M, Musher DM. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10:83–92. doi: 10.1016/S1473-3099(09)70331-7. [DOI] [PubMed] [Google Scholar]
- 47.Clayton TC, Thompson M, Meade TW. Recent respiratory infection and risk of cardiovascular disease: case-control study through a general practice database. Eur Heart J. 2007;29:96–103. doi: 10.1093/eurheartj/ehm516. [DOI] [PubMed] [Google Scholar]
- 48.Musher DM, Rueda AM, Kaka AS, Mapara SM. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis. 2007;45:158–165. doi: 10.1086/518849. [DOI] [PubMed] [Google Scholar]
- 49.Meier CR, Jick SS, Derby LE, Vasilakis C, Jick H, Meier C, et al. Acute respiratory-tract infections and risk of first-time acute myocardial infarction. Lancet. 1998;351:1467–1471. doi: 10.1016/s0140-6736(97)11084-4. [DOI] [PubMed] [Google Scholar]
- 50.Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR. Acute myocardial infarction and influenza: a meta-analysis of case–control studies. Heart. 2015;101:1738–1747. doi: 10.1136/heartjnl-2015-307691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blasco A, Coronado M-J, Hernández-Terciado F, Martín P, Royuela A, Ramil E, et al. Assessment of neutrophil extracellular traps in coronary thrombus of a case series of patients with COVID-19 and myocardial infarction. JAMA Cardiol. 2021;6:469. doi: 10.1001/jamacardio.2020.7308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mahmud E, Dauerman HL, Welt FGP, Messenger JC, Rao SV, Grines C, et al. Management of acute myocardial infarction during the COVID-19 pandemic. Catheter Cardiovasc Interv. 2020;96:336–345. doi: 10.1002/ccd.28946. [DOI] [PubMed] [Google Scholar]
- 53.Gopinathannair R, Merchant FM, Lakkireddy DR, Etheridge SP, Feigofsky S, Han JK, et al. COVID-19 and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies. J Interv Card Electrophysiol. 2020;59:329–336. doi: 10.1007/s10840-020-00789-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, et al. Worldwide survey of COVID-19–associated arrhythmias. Circ Arrhythm Electrophysiol. 2021;14:285–295. doi: 10.1161/CIRCEP.120.009458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chorin E, Wadhwani L, Magnani S, Dai M, Shulman E, Nadeau-Routhier C, et al. QT interval prolongation and torsade de pointes in patients with COVID-19 treated with hydroxychloroquine/azithromycin. Heart Rhythm. 2020;17:1425–1433. doi: 10.1016/j.hrthm.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lazzerini PE, Capecchi PL, Laghi-Pasini F. Systemic inflammation and arrhythmic risk: lessons from rheumatoid arthritis. Eur Heart J. 2017;38:1717–1727. doi: 10.1093/eurheartj/ehw208. [DOI] [PubMed] [Google Scholar]
- 57.Lazzerini PE, Laghi-Pasini F, Acampa M, Srivastava U, Bertolozzi I, Giabbani B, et al. Systemic inflammation rapidly induces reversible atrial electrical remodeling: the role of interleukin-6–mediated changes in connexin expression. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.011006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aviles RJ, Martin DO, Apperson-Hansen C, Houghtaling PL, Rautaharju P, Kronmal RA, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003;108:3006–3010. doi: 10.1161/01.CIR.0000103131.70301.4F. [DOI] [PubMed] [Google Scholar]
- 59.Bhatla A, Mayer MM, Adusumalli S, Hyman MC, Oh E, Tierney A, et al. COVID-19 and cardiac arrhythmias. Heart Rhythm. 2020;17:1439–1444. doi: 10.1016/j.hrthm.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Amir M, Djaharuddin I, Sudharsono A, Ramadany S. COVID-19 concomitant with infective endocarditis: a case report and review of management. Int J Infect Dis. 2020;98:109–112. doi: 10.1016/j.ijid.2020.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kumar R, Kumar J, Daly C, Edroos SA. Acute pericarditis as a primary presentation of COVID-19. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-237617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Deng Q, Hu B, Zhang Y, Wang H, Zhou X, Hu W, et al. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int J Cardiol. 2020;311:116–121. doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lombardi CM, Carubelli V, Iorio A, Inciardi RM, Bellasi A, Canale C, et al. Association of troponin levels with mortality in Italian patients hospitalized with coronavirus disease 2019. JAMA Cardiol. 2020;5:1274. doi: 10.1001/jamacardio.2020.3538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 Infection. J Am Coll Cardiol. 2020;76:533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Frencken JF, van Baal L, Kappen TH, Donker DW, Horn J, van der Poll T, et al. Myocardial injury in critically ill patients with community-acquired pneumonia. a cohort study. Ann Am Thorac Soc. 2019;16:606–612. doi: 10.1513/AnnalsATS.201804-286OC. [DOI] [PubMed] [Google Scholar]
- 68.Gao C, Wang Y, Gu X, Shen X, Zhou D, Zhou S, et al. Association between cardiac injury and mortality in hospitalized patients infected with avian influenza A (H7N9) virus. Crit Care Med. 2020;48:451–458. doi: 10.1097/CCM.0000000000004207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Spies C, Haude V, Fitzner R, Schröder K, Overbeck M, Runkel N, et al. Serum cardiac troponin T as a prognostic marker in early sepsis. Chest. 1998;113:1055–1063. doi: 10.1378/chest.113.4.1055. [DOI] [PubMed] [Google Scholar]
- 70.Vasile VC, Chai H-S, Khambatta S, Afessa B, Jaffe AS. Significance of elevated cardiac troponin T levels in critically ill patients with acute respiratory disease. Am J Med. 2010;123:1049–1058. doi: 10.1016/j.amjmed.2010.06.021. [DOI] [PubMed] [Google Scholar]
- 71.Sharma A, Garcia G, Wang Y, Plummer JT, Morizono K, Arumugaswami V, et al. Human iPSC-derived cardiomyocytes are susceptible to SARS-CoV-2 infection. Cell Rep Med. 2020;1 doi: 10.1016/j.xcrm.2020.100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bojkova D, Wagner JUG, Shumliakivska M, Aslan GS, Saleem U, Hansen A, et al. SARS-CoV-2 infects and induces cytotoxic effects in human cardiomyocytes. Cardiovasc Res. 2020;116:2207–2215. doi: 10.1093/cvr/cvaa267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, et al. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020;5:1281. doi: 10.1001/jamacardio.2020.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Caro-Codón J, Rey JR, Buño A, Iniesta AM, Rosillo SO, Castrejon-Castrejon S, et al. Characterization of NT-proBNP in a large cohort of COVID-19 patients. Eur J Heart Fail. 2021;23:456–464. doi: 10.1002/ejhf.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Daniels CJ, Rajpal S, Greenshields JT, Rosenthal GL, Chung EH, Terrin M, et al. Prevalence of clinical and subclinical myocarditis in competitive athletes with recent SARS-CoV-2 infection. JAMA Cardiol. 2021 doi: 10.1001/jamacardio.2021.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular Magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42:1866–1878. doi: 10.1093/eurheartj/ehab075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hayama H, Ide S, Moroi M, Kitami Y, Bekki N, Kubota S, et al. Elevated high-sensitivity troponin is associated with subclinical cardiac dysfunction in patients recovered from coronavirus disease 2019. Glob Health Med. 2021;3:95–101. doi: 10.35772/ghm.2021.01025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Metlay JP, Fine MJ, Schulz R, Marrie TJ, Coley CM, Kapoor WN, et al. Measuring symptomatic and functional recovery in patients with community-acquired pneumonia. J Gen Intern Med. 1997;12:423–430. doi: 10.1046/j.1525-1497.1997.00074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang C-CH, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313:264. doi: 10.1001/jama.2014.18229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jeffery MM, D'Onofrio G, Paek H, Platts-Mills TF, Soares WE, Hoppe JA, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180:1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77:159–169. doi: 10.1016/j.jacc.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wu J, Mamas MA, MO Mohamed, Kwok CS, Roebuck C, Humberstone B, et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107:113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 91.Aktaa S, Wu J, Nadarajah R, Rashid M, de Belder M, Deanfield J, et al. Incidence and mortality due to thromboembolic events during the COVID-19 pandemic:multi-sourced population-based health records cohort study. Thromb Res. 2021;202:17–23. doi: 10.1016/j.thromres.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dunstan DW, Dogra S, Carter SE, Owen N. Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev Cardiol. 2021;18:637–648. doi: 10.1038/s41569-021-00547-y. [DOI] [PubMed] [Google Scholar]
- 93.Qian C, Lyu X, Zhu H-D, Zhang Y, Du R-J, Li R, et al. Venous thromboembolism in non-COVID-19 population during the pandemic: a nationwide multicenter retrospective survey. J Thromb Thrombolysis. 2021:1–7. doi: 10.1007/s11239-021-02442-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tomidokoro D, Hayama H, Okazaki T, Hara H, Hiroi Y. The effect of the COVID-19 pandemic on incidence and characteristics of pulmonary embolism. Glob Health Med. 2021;3:122–124. doi: 10.35772/ghm.2020.01119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Silva B, Rodrigues T, Cunha N, Brito J, Alves Da Silva P, Silverio Antonio P, et al. Pulmonary embolism during the COVID-19 pandemic. Eur J Preventive Cardiol. 2021;28 zwab061.183. [Google Scholar]
- 96.Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, Li Q, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. 2021 doi: 10.1136/bjsports-2021-104080. [DOI] [PubMed] [Google Scholar]
- 97.Lee SW, Lee J, Moon SY, Jin HY, Yang JM, Ogino S, et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. 2021 doi: 10.1136/bjsports-2021-104203. [DOI] [PubMed] [Google Scholar]
- 98.Lau D, McAlister FA. Implications of the COVID-19 pandemic for cardiovascular disease and risk-factor management. Can J Cardiol. 2021;37:722–732. doi: 10.1016/j.cjca.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wosik J, Clowse MEB, Overton R, Adagarla B, Economou-Zavlanos N, Cavalier J, et al. Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. Am Heart J. 2021;231:1–5. doi: 10.1016/j.ahj.2020.10.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Avaldi VM, Lenzi J, Urbinati S, Molinazzi D, Descovich C, Campagna A, et al. Effect of cardiologist care on 6-month outcomes in patients discharged with heart failure: results from an observational study based on administrative data. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-018243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hawkins NM, Scheuermeyer FX, Youngson E, Sandhu RK, Ezekowitz JA, Kaul P, et al. Impact of cardiology follow-up care on treatment and outcomes of patients with new atrial fibrillation discharged from the emergency department. EP Europace. 2020;22:695–703. doi: 10.1093/europace/euz302. [DOI] [PubMed] [Google Scholar]
- 102.Laoutaris ID, Dritsas A, Adamopoulos S. Cardiovascular rehabilitation in the COVID-19 era: ‘a phoenix arising from the ashes? Eur J Prev Cardiol. 2021:zwab116. doi: 10.1093/eurjpc/zwab116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME, et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic. Circulation. 2020;142:510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pouwels KB, Pritchard E, Matthews PC, Stoesser N, Eyre DW, Vihta K-D, et al. Impact of Delta on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. medRxiv. 2021 doi: 10.1038/s41591-021-01548-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rauch S, Jasny E, Schmidt KE, Petsch B. New vaccine technologies to combat outbreak situations. Front Immunol. 2018;9:1963. doi: 10.3389/fimmu.2018.01963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.US Department of Health and Human Services/Centers for Disease Control and Prevention Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: Update from the Advisory Committee on Immunization Practices — United States, June 2021. MMWR. 2021;70:977–982. doi: 10.15585/mmwr.mm7027e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN, et al. Patients with acute myocarditis following mRNA COVID-19 vaccination. JAMA Cardiol. 2021;27710:1–6. doi: 10.1001/jamacardio.2021.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, et al. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. 2021;92134:6–10. doi: 10.1001/jamacardio.2021.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Makris M, Pavord S, Lester W, Scully M, Hunt B. Vaccine-induced immune thrombocytopenia and thrombosis (VITT) Res PracticeThromb Haemost. 2021;5:2–5. doi: 10.1002/rth2.12529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pavord S, Scully M, Hunt BJ, Lester W, Bagot C, Craven B, et al. Clinical features of vaccine-induced immune thrombocytopenia and thrombosis. N Engl J Med. 2021 doi: 10.1056/NEJMoa2109908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Thaler J, Ay C, Gleixner KV, Hauswirth AW, Cacioppo F, Grafeneder J, et al. Successful treatment of vaccine-induced prothrombotic immune thrombocytopenia (VIPIT) J Thrombo Haemostas. 2021;19:1819–1822. doi: 10.1111/jth.15346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.WHO. Guidance for clinical case management of thrombosis with thrombocytopenia syndrome(TTS) following vaccination to prevent coronavirus disease (COVID-19). 2021. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-TTS-2021.1. [PubMed]
- 113.Patriquin CJ, Laroche V, Selby R, Pendergrast J, Barth D, Côté B, et al. Therapeutic plasma exchange in vaccine-induced immune thrombotic thrombocytopenia. N Engl J Med. 2021;385:857–859. doi: 10.1056/NEJMc2109465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Barda N, Dagan N, Ben-Shlomo Y, Kepten E, Waxman J, Ohana R, et al. Safety of the BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2021 doi: 10.1056/NEJMoa2110475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hippisley-Cox J, Patone M, Mei XW, Saatci D, Dixon S, Khunti K, et al. Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. BMJ. 2021;374:n1931. doi: 10.1136/bmj.n1931. [DOI] [PMC free article] [PubMed] [Google Scholar]