Fig. 1. Study design.
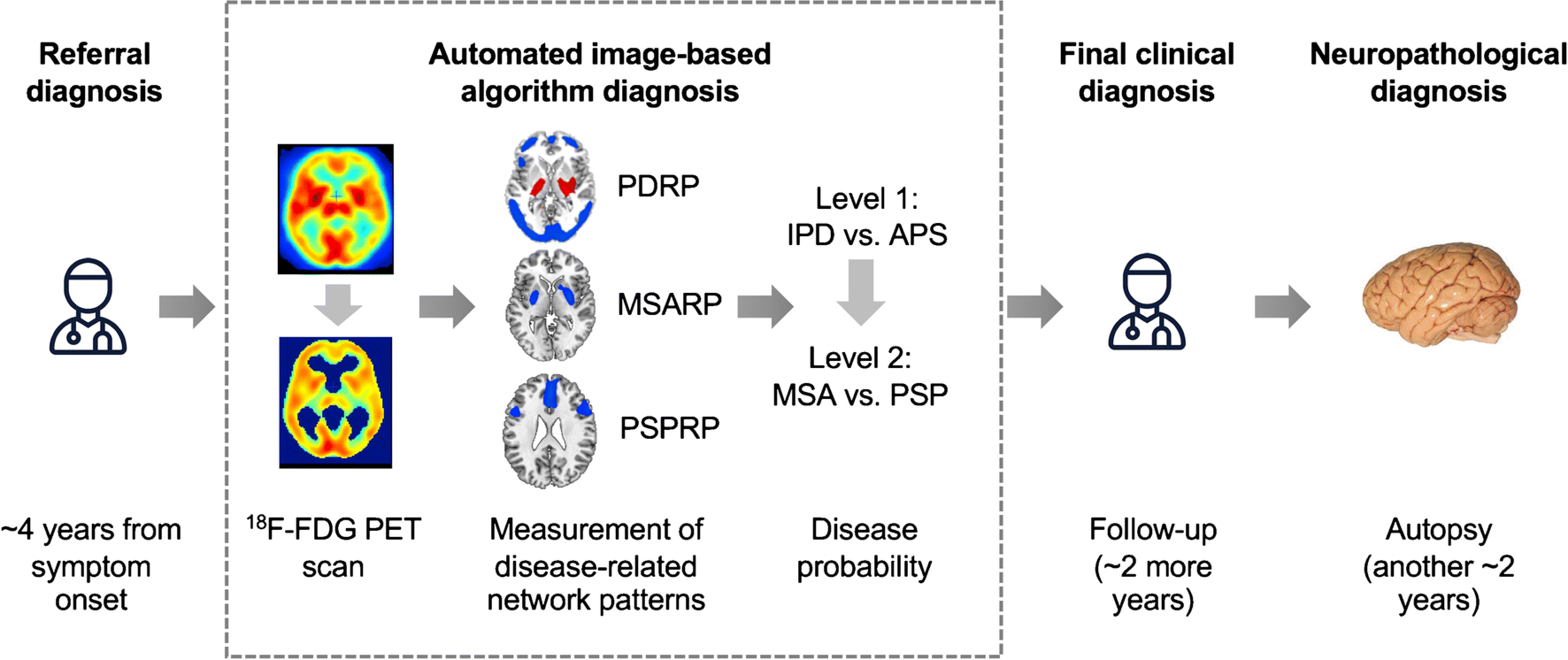
Patients with parkinsonism and uncertain clinical diagnosis were referred by a movement disorder specialist for brain imaging with FDG PET an average of 4 years from symptom onset. The first step (Level 1) determines whether the diagnosis is likely IPD or an atypical parkinsonian syndrome (APS); if the algorithm predicts an APS, Level 2 evaluates the diagnosis of progressive supranuclear palsy, and multiple system atrophy. At either Level, the pattern expression may be insufficiently developed for the algorithm to render a diagnosis, leading to an indeterminate (IND) diagnosis. The probability of each disease was calculated for every case (see Methods and Table 2). Each patient was followed clinically by a specialist who was blind to the results of the imaging algorithm. For every case, the referral diagnosis, the algorithm’s diagnosis, and the final clinical diagnosis were compared to the neuropathology, determined an average of two years after the final clinical diagnosis. [Abbreviations: 18F-FDG PET=fluorodeoxyglucose positron emission tomography; PSPRP=progressive supranuclear palsy-related pattern; MSARP=multiple system atrophy-related pattern; PDRP=Parkinson’s disease-related pattern]
