Fig. 1.
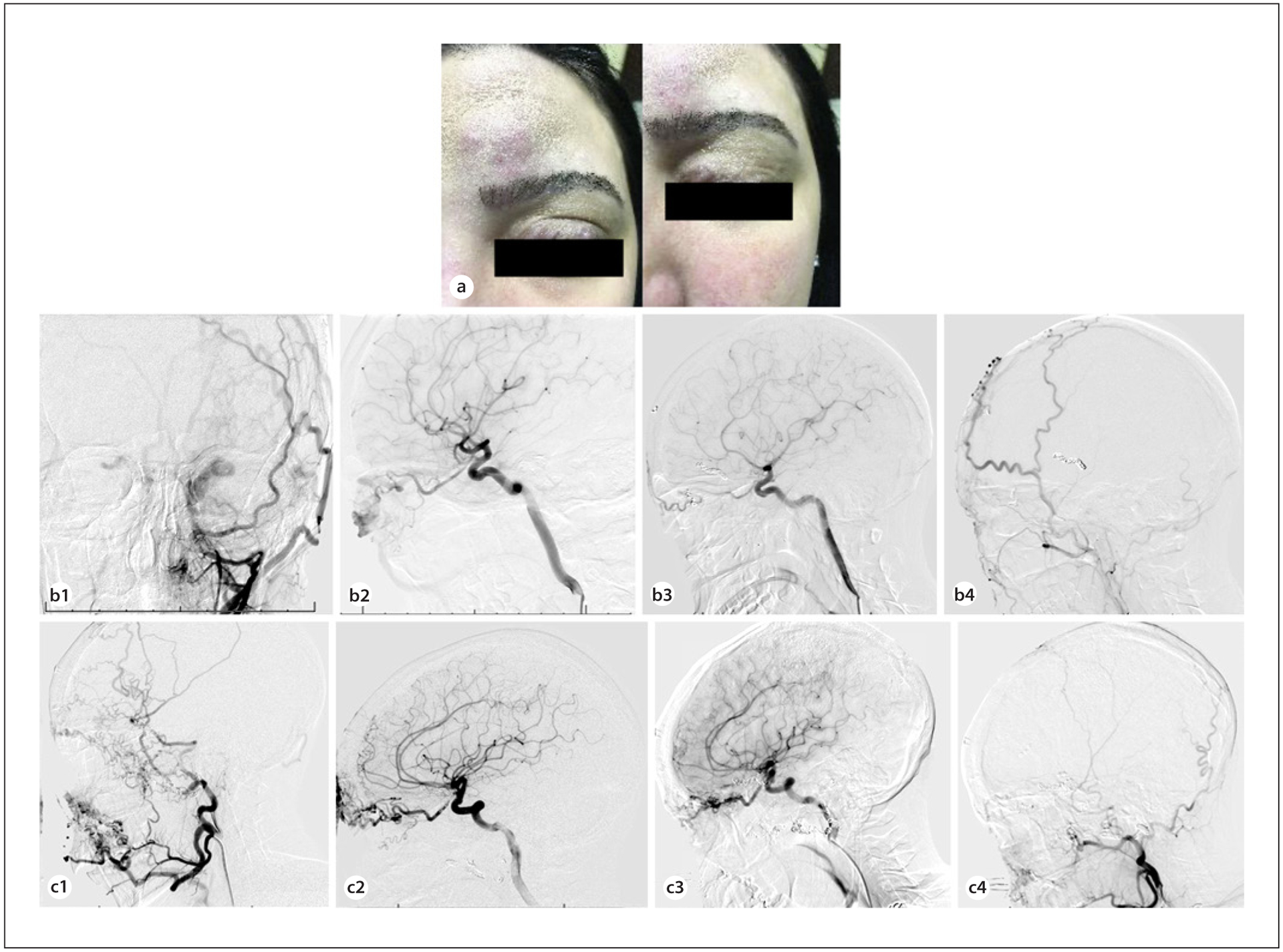
a A 23-year-old woman presented with difficulty opening her eye, pain, and swelling secondary to a left orbito-facial AVM. Curative surgery in this case would have involved extensive soft tissue dissection, and the patient wished to avoid undesirable cosmetic defects from open surgery. b The malformation prior to embolization was fed by branches of the facial and superficial temporal arteries as seen on anteroposterior projection of left external carotid injection (b1). Lateral projected view of internal carotid injection shows blood supply from the ophthalmic artery (b2). At 6-month follow-up after embolization and therapy with rapamycin, minimal residual contrast is visualized within the AVM on AP (b3) and lateral (b4) angiography of the external and internal carotid, respectively. c A 28-year-old woman with a right facial-orbital AVM presented with refractory epistaxis and left-sided retro-orbital pressure. She had previously undergone multiple operations, including enucleation of the right eye. The AVM was supplied by feeders arising from the internal maxillary, lingual, and superficial temporal arteries, as shown in the lateral external carotid injection (c1), and by the ophthalmic artery as shown in the lateral internal carotid injection (c2). In staged sessions, feeding pedicles including branches of the ophthalmic and sphenopalatine arteries were embolized and coiling of the ophthalmic artery aneurysm were performed. The patient subsequently initiated therapy with rapamycin. At 1-year follow-up, there was no significant increase in residual filling at the mandible from the facial and lingual arteries and the inferolateral trunk compared to what was seen following embolization (lateral projection of internal carotid injection (c3); lateral projection of external carotid injection (c4)). Epistaxis was noted to have ceased completely. AVM, arteriovenous malformation.
