Abstract
Objective
To synthesize the nature and extent of research on rehabilitation care provision to patients with COVID‐19. Specifically, we aimed to (1) describe the impact of COVID on patients and associated rehabilitation needs, (2) outline the adaptations and preparations required to enable the provision of COVID rehabilitation, (3) describe the types of rehabilitation services and treatments provided to COVID patients, and (4) identify barriers and facilitators to delivering COVID rehabilitation.
Literature Survey
We searched Medline, PsychINFO, Embase, and CINAHL on June 26, 2020 using key words such as “rehabilitation,” “physical medicine,” “allied health professionals,” and variations of “COVID.” The search was updated on October 13, 2020. We included articles published in English and that focused on some aspect of COVID rehabilitation for adults. We excluded articles focused on pediatric populations and those not focused (or minimally focused) on rehabilitation for COVID patients.
Methodology
Data were charted based on article type (ie, primary data, secondary data, guidelines). Key information extracted included (1) COVID sequelae; (2) rehabilitation adaptations; (3) structure, function, and content of rehabilitation services/programs; (4) facilitators and/or barriers to providing COVID rehabilitation; and (5) recommendations for COVID rehabilitation programming. Data were synthesized narratively.
Synthesis
In total, 128 articles were included in the review that reported primary data (n = 33), secondary data (n = 82), and clinical practice/patient self‐management guidelines (n = 13). Evidence begins to suggest that rehabilitation is necessary and valuable for addressing COVID‐related declines in health, function, and well‐being. Most articles recommended that an individualized rehabilitation program be provided across the continuum of care by an interdisciplinary team of professionals and that the nature and extent of rehabilitation be informed by the care setting and COVID severity. Most issues that challenged COVID rehabilitation delivery were directly addressed by the facilitators and adaptations identified.
Conclusions
Future recommendations include a greater emphasis on the psychosocial aspects of COVID rehabilitation, inclusion of families in rehabilitation planning, and the use of qualitative approaches to complement clinical data.
BACKGROUND
The COVID‐19 pandemic has required a rapid and drastic response by health care systems worldwide, including major changes in how organizations and staff function and deliver patient care. 1 Growing evidence indicates that many survivors are experiencing “long COVID” (ie, lasting and debilitating symptoms that impede both physical and emotional recovery). 2 In turn, rehabilitation is being recognized as a pivotal aspect of the postacute COVID 3 , 4 response. Critically ill patients with COVID are typically ventilated for longer than other patients requiring care in the intensive care unit (ICU), which can lead to higher levels of physical deconditioning. 5 They also experience neurological and respiratory impairments, increasing the likelihood of a more complex and prolonged recovery. 5 Existing evidence on sepsis (which has an inpatient mortality rate similar to that of COVID) indicates that 30% of hospitalized patients require posacute care. 6 In the United Kingdom, it is estimated that 45% of COVID patients will need some form of rehabilitation and that 4% will require more specialized and long‐term rehabilitation in an inpatient setting. 5
Unfortunately, rehabilitation is often underemphasized in global disaster planning and responses, and the need for rehabilitation is often not recognized until many months after a disaster. 7 Yet rehabilitation is a key component of standard care delivery pathways and in other populations improves independence, facilitates community reintegration, and mitigates long‐term disability. 8 For patients with COVID, rehabilitation can improve functional capacity, address the effects of deconditioning after prolonged ICU stays, and alleviate stress by providing patients with needed support throughout recovery. 9 Collectively, this can potentially facilitate patients' return to home and vocational activities. Rehabilitation has been described as a necessity and right in the context of the COVID pandemic, and it is recommended that it be routinely incorporated into pandemic response plans early on before widespread disability. 5
The COVID care pathway is complicated by several issues including (1) a lack of clarity around the patients' eligibility for rehabilitation,10 (2) the ability of rehabilitation facilities/units to adapt and prepare for COVID patients, and (3) the impact of physical distancing on the provision of rehabilitation treatments and community discharge support. In light of the mounting recognition that rehabilitation will play a key role in COVID patients' recovery, many studies and practice guidelines have begun to address these issues. By synthesizing information across these data sources, our scoping review aims to provide rehabilitation practitioners with a comprehensive review of the evidence to support the ongoing rehabilitation response to the pandemic.
STUDY GOAL AND OBJECTIVES
Our goal was to synthesize the nature and extent of research on rehabilitation care provision to COVID patients. Specifically, we aimed to:
Describe the impact of COVID on patients and associated rehabilitation needs;
Outline the adaptations and preparations required to enable the provision of COVID rehabilitation;
Describe the types of rehabilitation services and treatments provided to patients with COVID; and
Identify barriers and facilitators to delivering COVID rehabilitation.
METHODS
We followed Arksey and O'Malley's methodological framework for conducting scoping reviews. 11 The framework entails five stages: (1) identifying the research questions; (2) identifying relevant studies; (3) study selection; (4) charting the data; and (5) collating, summarizing, and reporting the results. We searched Medline, PsychINFO, Embase, and CINAHL on June 26, 2020. For stage 2, the search strategy was tailored to each database using key terms that included “rehabilitation,” “physical medicine,” “allied health professionals,” and variations of “COVID‐19” (see Appendix A for Medline search strategy). For stage 3, articles were included if they were in English and focused on some aspect of rehabilitation care specifically for COVID patients. Research articles reporting both primary and secondary data were included. Articles were excluded if they were (1) not focused on the COVID pandemic, (2) not focused on the field of rehabilitation, (3) not focused on rehabilitation for COVID patients (ie, focused on some aspect of rehabilitation in the context of the pandemic but not on care for COVID patients themselves), and (4) focused on a pediatric population.
The database searches produced 1399 studies for consideration. After duplicates were eliminated, 1167 articles remained. A two‐phase screening process was undertaken. For phase 1, M.B.W. reviewed the title and abstracts to determine if they were eligible for full‐text review. This resulted in the identification of 252 articles for full‐text review. For phase 2, M.B.W. and S.R.C. first screened 10% of the articles to establish interrater reliability (k = 0.746, 88% agreement). Discrepancies were resolved by discussing the abstract(s) in question and coming to a consensus. M.B.W. and S.R.C. then proceeded to screen the remainder of the articles, where 57 met the inclusion/exclusion criteria and were included in the review. Our hand search identified an additional 11 articles for inclusion in the review. In total, 68 studies were included. We conducted an updated search on October 13, 2020. After screening and full‐text review (conducted by S.R.C. and K.M.K.), we identified an additional 60 articles for inclusion. In total, we included 128 articles in our review. See Figure 1 for a Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) Flow Diagram of article selection.
FIGURE 1.
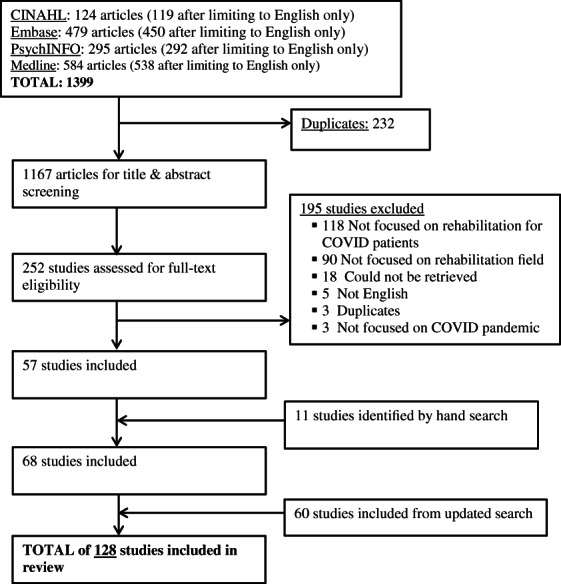
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram
For stage 4, we used a data abstraction chart to extract relevant information from studies (eg, sample details, rehabilitation program details). For stage 5, we employed a narrative synthesis of the included studies to answer the research questions. 12 Analysis was an iterative process of combining, categorizing, summarizing, and comparing information across studies.
RESULTS
Study demographics
The initial search on June 26, 2020 produced 1167 articles after deduplication, of which 68 met the inclusion/exclusion criteria. Our updated search on October 13, 2020 produced 2501 articles after deduplication, of which 60 met the inclusion/exclusion criteria. In total, we included 128 articles in our review (see Figure 1 for PRISMA diagram). 3 , 4 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 With respect to article type, 33 were primary data articles (ie, observational studies, case reports), 22 , 24 , 33 , 41 , 51 , 55 , 57 , 63 , 69 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 115 , 117 , 119 , 127 , 128 , 129 , 131 , 132 , 134 , 136 , 137 , 138 82 were secondary articles (ie, reviews, letters to the editor that did not report results of an original research project, commentaries) 3 , 4 , 14 , 17 , 18 , 19 , 20 , 21 , 25 , 27 , 28 , 29 , 30 , 31 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 53 , 54 , 56 , 58 , 59 , 60 , 62 , 64 , 65 , 66 , 67 , 68 , 70 , 71 , 73 , 74 , 75 , 90 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 116 , 118 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 130 , 133 , 135 and 13 were articles reporting guidelines for rehabilitation in COVID patients. 13 , 15 , 16 , 23 , 26 , 32 , 50 , 52 , 61 , 72 , 76 , 77 , 91 Details pertaining to the geographic distribution of research can be found in Table 1.
TABLE 1.
Geographic distribution of COVID rehabilitation research
| Continent | Country | Articles (N) | Citations |
|---|---|---|---|
| Europe (n = 54) | Italy | 24 | 3, 14, 18, 19, 24, 29, 36, 43, 44, 48, 51, 54, 60, 63, 68, 69, 94, 110, 111, 114, 117, 119, 121, 122 |
| United Kingdom | 17 | 16, 23, 25, 30, 34, 52, 57, 61, 70, 71, 72, 80, 95, 97, 104, 108, 109 | |
| Turkey | 4 | 15 , 20 , 67 , 118 | |
| Spain | 2 | 90 , 100 | |
| France | 2 | 38, 55 | |
| Denmark | 1 | 26 | |
| Greece | 1 | 33 | |
| Switzerland | 1 | 84 | |
| Netherlands | 1 | 17 | |
| Multi‐country | 1 | 21 | |
| Asia (n = 33) | China | 14 | 22, 40, 41, 56, 74, 75, 77, 78, 89, 96, 98, 128, 134, 135 |
| Japan | 6 | 47, 49, 85, 103, 136, 137 | |
| India | 4 | 31, 99, 126, 127 | |
| Singapore | 3 | 87, 132, 138 | |
| Korea | 1 | 115 | |
| Taiwan | 1 | 120 | |
| Iran | 1 | 58 | |
| Nepal | 1 | 107 | |
| Philippines | 1 | 37 | |
| Israel | 1 | 133 | |
| The Americas (n = 31) | United States | 21 | 27, 28, 39, 42, 45, 46, 64, 65, 73, 79, 81, 82, 83, 86, 92, 102, 112, 123, 129, 130, 131 |
| Canada | 4 | 4 , 32 , 62 , 93 | |
| Brazil | 4 | 53 , 59 , 101 , 125 | |
| Multicountry | 2 | 50 , 91 | |
| Australia (n = 5) | Australia | 4 | 13, 35, 66, 88 |
| New Zealand | 1 | 76 | |
| Africa (n = 3) | Nigeria | 2 | 105 , 106 |
| Morocco | 1 | 113 | |
| Multi‐content (n = 2) | — | 2 | 116 , 124 |
Note: Citations bolded correspond to articles reporting primary data. The remaining references correspond to secondary data articles and guidelines.
Primary study details
Of the 33 articles that reported primary data, most were cross‐sectional in nature and aimed to describe the development and delivery of a rehabilitation program for patients with COVID (n = 13). 22 , 24 , 33 , 41 , 51 , 63 , 69 , 78 , 81 , 88 , 127 , 129 , 136 Additionally, one article described a physician's experience with being treated for COVID, 57 a second outlined the organizational changes made to accommodate COVID patients, 63 and a third estimated the postacute rehabilitation needs of COVID patients. 55 Three studies aimed to describe the demographics, clinical characteristics, and level of rehabilitation of patients with COVID at their institutions. 79 , 80 , 85 One additional study investigated the rehabilitation needs of COVID patients at their institution. 134 Only one study implemented a randomized control trial (RCT) design to investigate the outcomes of a pulmonary rehabilitation program for COVID patients. 41
Study sample characteristics
In total, 30 studies reported sample sizes. Seventeen case report studies reported on 1 to 9 patients, 33 , 51 , 78 , 79 , 81 , 83 , 84 , 85 , 86 , 88 , 115 , 117 , 119 , 128 , 131 , 132 , 137 , 138 and the remaining 16 studies reported sample sizes ranging from 9 to 312, with a mean of 101. The mean age of patients in the case reports was 53 years old (range: 41‐69). Five of the cross‐sectional studies 22 , 24 , 63 , 127 , 129 reported the mean age of patients in the sample (50‐73 years old; mean = 63) and one study 55 reported the median (66 years old; interquartile range: 45; 85). A third cross‐sectional study reported age groups for their participants (ie, ≤35, 36‐50, 51‐65, ≥76). 134 The RCT reported a mean of 69.4 years old for the intervention group and 68.9 for the control group. Twenty‐seven studies reported participants' gender. All but five of the case reports 83 , 115 , 128 , 131 , 132 reported on male patients 33 , 51 , 78 , 79 , 81 , 84 , 85 , 86 , 88 , 117 , 119 , 137 , 138 and the RCT study included only men in both the intervention (n = 24) and control groups (n = 25). The remaining six cross‐sectional studies 22 , 24 , 55 , 127 , 129 , 134 reported a mean of 61 women and 101 men. Ten studies reported information pertaining to patients' ICU length of stay (LOS). The manner of reporting varied, with two studies reporting a mean of 5 22 and 16.4 days 24 and one reporting a median of 15 days (interquartile range: 2;30), 55 whereas two studies were similar at 14 days. 83 , 136 Another study mean reported a mean of 19 days (± 10 days). 80 The mean ICU LOS across the case report studies was 18.8 days. 33 , 51 , 78 , 115 , 119 , 131 Only one study reported a 25‐day postacute rehabilitation LOS. 51 Other studies reported an overall rehabilitation LOS of 10 days to 14 weeks. 81 , 84 , 87 , 88 , 119 , 127 , 136
COVID sequelae
In total, 19 of the 33 articles reporting primary data discussed COVID sequelae that would warrant the need for rehabilitation for this population. 22 , 33 , 51 , 55 , 57 , 63 , 69 , 79 , 80 , 81 , 87 , 115 , 117 , 119 , 127 , 128 , 129 , 131 , 136 , 137 Table 2 outlines the specific sequelae reported.
TABLE 2.
COVID sequelae details from primary data articles (n = 22)
| COVID sequelae | Manifestation |
|---|---|
| Respiratory (n = 15) | Obstructive respiratory dysfunction, pneumonia, deterioration and/or failure of respiratory function, dyspnea, cough, and intensive care unit‐acquired weakness. 22 , 33 , 51 , 55 , 57 , 82 , 87 , 119 , 127 , 128 , 129 , 131 , 136 , 137 , 138 |
| Physical (n = 11) |
Muscle weakness and fever. 22 , 51 , 57 , 63 , 83 , 87 , 129 , 137 COVID‐related fatigue and pain were discussed and included overall fatigue, nausea, vomiting, and myalgia. 57 , 82 , 119 One case study described lower‐limb amputation as the result of COVID related coagulopathy. 117 |
| Psychosocial (n = 7) | Anxiety, depression, sense of abandonment, isolation, fear, posttraumatic stress syndrome. 69 , 83 , 87 , 115 , 119 , 128 , 138 |
| Cognitive (n = 3) | Delirium. 80 , 84 , 86 |
| Cardiovascular (n = 2) | Coagulopathy, stroke, and myocarditis. 117 , 127 |
| Organ system(s) failure (n = 2) | Renal failure was mentioned by one article, 55 and another mentioned multiorgan failure. 127 |
| Communication/swallowing (n = 1) | One study reported dysphagia. 84 |
Comorbidities
Eleven articles mentioned common comorbidities that COVID patients presented with, including cardiovascular comorbidities (eg, hypertension, arrhythmias, heart disease), 24 , 41 , 69 , 80 , 83 , 85 , 86 , 115 , 117 , 131 , 134 overweight/obesity, 83 , 86 , 119 , 128 , 131 mental health diagnosis (eg, depression), 86 , 115 , 119 preexisting respiratory disease (eg, chronic obstructive pulmonary disease [COPD]), 117 , 132 , 134 type 2 diabetes, 24 , 41 , 80 , 83 , 85 , 117 , 131 , 134 and other chronic diseases (eg, liver disease, hyperthyroidism, polyneuropathy). 117 , 129 , 134
Rehabilitation admission criteria
Six articles discussed potential criteria and associated assessments that could be used to identify COVID patients for postacute rehab. The most commonly discussed criteria were as follows:
Age (>65 years) 41
Mechanical ventilation and tracheostomy status (ie, those who were ventilated are expected to need rehab) 80
Functional status 51 , 55 , 138 (eg, high level of dependency as determined by an activities of daily living [ADL] score < 4)
Dyspnea 51 , 138 (eg, using Medical Research Council Dyspnoea Scale 24 )
Other considerations for identifying eligible COVID patients included body composition, muscle function, and quality of life. 51 , 138 Two articles suggested that patients might potentially be excluded from rehab because of other comorbidities (eg, stroke, neurodegenerative diseases, additional respiratory complications). 24 , 41
Adaptations to rehabilitation
Six studies discussed the adaptations made to provide rehabilitation to COVID patients. 63 , 80 , 82 , 84 , 137 , 138 These adaptations included (1) modifying tasks, roles, and scheduling of the rehabilitation teams; (2) creating multidisciplinary COVID teams including the physicians, nurses, respiratory physiotherapists (RPTs), and physiotherapists (PTs); (3) scheduling changes, including scaling back staff numbers to address personal protective equipment (PPE) shortages; (4) delegating tasks based on expertise (eg, RPTs trained in management of chronic respiratory failure and noninvasive ventilation); (5) organizing an online communication system to facilitate email and printing of documents (so as to minimize contact between care team members); and (6) mandating PPE for patients undergoing rehabilitation. Some studies described moving from in‐person rehabilitation to telerehabilitation. 84 , 88 , 136
Nature of rehabilitation programs
All of the articles provided information on what a rehabilitation program for COVID patients could entail (Table 3).
TABLE 3.
Nature of rehabilitation program (primary data articles)
| Program element | Details |
|---|---|
| Timing |
|
| Duration and frequency of rehabilitation activities | |
| Modality |
|
| Disciplines involved | |
| Rehabilitation treatments/services provided |
Respiratory Therapy Interventions
:
|
| Pulmonary Therapy Interventions : | |
| Musculoskeletal Therapy Interventions : | |
| Psychosocial Therapy Interventions : | |
| Speech‐Language Therapy Interventions : |
Abbreviation: ICU, intensive care unit.
Secondary data article details
Of the 82 secondary articles, 57 articles specified the place of rehabilitation (ie, acute care/ICU (n = 39), 3 , 4 , 17 , 19 , 20 , 21 , 27 , 28 , 29 , 30 , 36 , 39 , 40 , 43 , 44 , 46 , 49 , 53 , 59 , 60 , 62 , 64 , 66 , 68 , 73 , 75 , 96 , 99 , 105 , 107 , 110 , 114 , 118 , 120 , 122 , 123 , 124 , 126 , 130 postacute/ICU discharge (n = 10), 3 , 28 , 29 , 44 , 64 , 68 , 95 , 110 , 118 , 122 inpatient rehabilitation (n = 15), 18 , 19 , 21 , 29 , 38 , 39 , 48 , 62 , 74 , 110 , 112 , 124 , 130 , 133 and community‐based setting (n = 20). 17 , 25 , 27 , 30 , 39 , 40 , 47 , 53 , 54 , 56 , 65 , 67 , 73 , 74 , 105 , 107 , 109 , 111 , 120 , 130 ) The most common rehabilitation profession to be involved in care for COVID patients was physiotherapy (n = 29), 4 , 19 , 20 , 27 , 47 , 49 , 58 , 59 , 60 , 64 , 65 , 66 , 68 , 73 , 96 , 102 , 103 , 104 , 105 , 106 , 107 , 109 , 111 , 113 , 114 , 122 , 125 , 126 , 130 with three studies highlighting the inclusion of RPTs. 30 , 36 , 53 Other rehabilitation professionals included physiatrists/physical medicine and rehabilitation (PMR) specialists (n = 11), 4 , 21 , 58 , 60 , 64 , 65 , 67 , 92 , 99 , 113 , 130 occupational therapists (OTs) (n = 11), 4 , 27 , 62 , 64 , 65 , 73 , 95 , 102 , 104 , 113 , 122 , 130 speech language pathologists (SLPs) (n = 7), 4 , 19 , 46 , 62 , 65 , 95 , 104 , 130 psychologists (n = 2), 112 , 113 dieticians (n = 1), 95 respiratory therapists (n = 1), 113 and social workers (n = 1). 62
COVID sequelae
In total, 60 articles discussed COVID sequelae (see Table 4).
TABLE 4.
COVID sequelae details from secondary data articles (n = 60)
| COVID Sequelae | Manifestation |
|---|---|
| Respiratory (n = 41) | Breathing difficulties, acute respiratory distress syndrome, lung damage, pneumonia, and hypoxia. 4 , 14 , 17 , 21 , 28 , 29 , 31 , 34 , 35 , 38 , 39 , 40 , 44 , 45 , 49 , 53 , 54 , 56 , 59 , 60 , 62 , 66 , 67 , 70 , 74 , 90 , 93 , 94 , 95 , 96 , 98 , 99 , 100 , 102 , 103 , 104 , 105 , 107 , 113 , 114 , 121 , 122 , 123 , 125 , 126 |
| Psychosocial (n = 30) | Depression, anxiety, posttraumatic stress disorder, and quality of life. 4 , 14 , 17 , 21 , 31 , 34 , 39 , 40 , 48 , 53 , 56 , 60 , 62 , 67 , 68 , 71 , 74 , 93 , 95 , 98 , 102 , 103 , 104 , 105 , 110 , 112 , 113 , 122 , 123 , 130 |
| Neurological (n = 35) |
Dizziness, impaired consciousness and polyneuropathy. 3 , 14 , 21 , 34 , 35 , 39 , 42 , 60 , 62 , 67 , 68 , 70 , 75 , 90 , 93 , 94 , 97 , 102 , 107 , 110 , 112 , 122 , 130 Impacts on cognition (eg, impaired memory, attention, and higher order executive function; delirium). 4 , 17 , 21 , 28 , 29 , 39 , 48 , 93 , 112 , 113 , 123 , 130 |
| Motor (n = 23) | Deconditioning and muscle weakness. 17 , 20 , 21 , 29 , 30 , 34 , 35 , 39 , 42 , 53 , 56 , 59 , 60 , 67 , 68 , 74 , 97 , 105 , 107 , 110 , 113 , 122 , 130 |
| Cardiovascular (n = 13) | Myopericarditis, thrombosis, and myocardial injury. 42 , 56 , 59 , 62 , 70 , 74 , 90 , 93 , 95 , 96 , 99 , 102 , 126 |
| Physical/movement (n = 10) | Problems with fatigue or pain 34 , 59 , 95 , 96 , 98 , 107 , 110 , 122 and fever. 101 , 102 |
| Organ system(s) failure (n = 9) | Renal and multiorgan failure. 56 , 62 , 70 , 74 , 95 , 96 , 102 , 104 , 126 |
| Communication/swallowing (n = 5) | Communication and swallowing issues. 21 , 46 , 114 , 122 , 123 |
| Other (n = 4) | Gastrointestinal issues 95 and malnutrition. 18 , 102 , 130 |
Comorbidities
Only 11 secondary articles identified comorbidities observed in individuals with COVID. 34 , 38 , 40 , 53 , 62 , 65 , 74 , 120 The most commonly discussed comorbidities were cardiovascular diseases 40 , 53 , 97 , 120 , 123 including coronary artery disease, 62 hypertension, 38 , 53 , 62 , 120 and stroke. 62 , 65 Other conditions included diabetes, 40 , 53 , 90 , 97 , 120 pressure injuries, 40 bladder dysfunction, 40 chronic pulmonary diseases, 74 , 120 , 123 , 126 cancer, 123 autoimmune diseases, 123 and neurological conditions. 65 , 126
Rehabilitation admission criteria
Only 12 of the secondary articles explicitly outlined criteria that could be used to determine COVID patients' eligibility for rehabilitation: (1) negative COVID status of the patient (eg, two consecutive negative nasal swabs within 24 hours or 7+ since diagnosis) 4 , 21 , 29 , 42 , 48 , 111 , 124 , 130 ; (2) stable cardiovascular function, respiratory function (eg, stable oxygen saturation with no need for respiratory assistance), nervous system function and general parameters (eg, no fever) 4 , 21 , 29 , 38 , 44 , 105 , 130 ; and (3) functional status of the patient should reflect some independence (as determined by the Functional Independence Measure). However, patients should receive rehabilitation to address any functional deficits they may be experiencing (eg, unable to complete some activities/instrumental activities of daily living, residual functional deficits owing to hospital‐acquired weakness). 29 , 70 , 73 Only two studies addressed ventilation status, with one suggesting that ventilator‐dependent patients to be tracheotomized at least 24 hours before admission 38 and the other recommending that rehabilitation not begin unless there is absence of ventilator resistance. 105
Adaptations to rehabilitation
Eighteen articles described adaptations to rehabilitation services that facilitated the provision of rehabilitation to COVID patients. These adaptations included (1) modifying the physical space of the rehabilitation unit/center (eg, to enable isolation of infectious COVID patients or to create additional space for ICU patients—many who could receive early rehabilitation as a result) or modifying tasks, roles, and schedules of the rehabilitation teams 4 , 19 , 29 , 38 , 39 , 43 , 49 , 62 , 65 , 66 , 107 , 123 ; (2) creating multidisciplinary COVID teams including physicians, nurses, RPTs, and PTs 29 , 35 , 38 , 49 , 107 ; (3) scheduling changes to address PPE shortages 4 ; (4) delegating tasks based on expertise (eg, matching approaches to the right profession, using best mix of skills) 25 , 68 , 107 ; and (5) using technology to facilitate communication between providers and to deliver rehabilitation at a distance. 25 , 62 , 73 , 123
Nature of rehabilitation programs across the continuum
All of the included articles discussed the nature of rehabilitation. Fourteen articles touched on what rehabilitation may look like in a broader context rather than within a specific area (ie, acute care). 3 , 14 , 31 , 37 , 42 , 45 , 58 , 70 , 71 , 96 , 99 , 113 , 121 , 125 The articles highlighted how rehabilitation is a vital component of care and recovery for persons with COVID. 14 , 31 Articles suggested that the COVID rehabilitation program include pulmonary, 31 , 58 , 125 cardiac, 31 respiratory, 45 , 113 physical, 45 , 58 , 70 , 113 , 121 psychosocial, 70 , 113 and swallowing 113 aspects. Postural positioning was discussed as an important technique to help mitigate the impacts of prolonged bedrest. 40 , 58 , 70 Only two studies described specific techniques that could be used in this population (eg, Zheng's recumbent exercises, airway clearance, bed mobility, sit to stand, walking, etc) but did not describe specific prescription information. 58 , 113 Articles also suggested that severity of the illness be considered when developing a therapy regimen. 45 , 58 , 71 Lopez and colleagues suggested that a registry be created to document symptoms and recovery trajectories over time of COVID patients to help inform rehabilitation practices going forward. 42 Finally, one study recommend the use of telehealth but did not describe a protocol. 37 An additional 12 articles provided specific suggestions for frequency, duration, and modality of COVID rehabilitation (see Table 5). Most of the suggestions were adapted from respiratory rehabilitation guidelines for COVID patients specifically 56 , 62 , 73 , 106 or for similar populations (eg, COPD, acute respiratory distress syndrome). 58 , 59 , 73 , 109 One article made recommendations based on front‐line expert consensus and references 74 and another adapted general exercise principles from the American College of Sports Medicine. 120 Three articles did not specify what they based their recommendations on. 47 , 60 , 122
TABLE 5.
Suggested modality, frequency, intensity and timing of rehabilitation protocols from secondary articles
| Article | Modality | Program components | Frequency | Intensity | Duration | Timing |
|---|---|---|---|---|---|---|
| Mukaino et al. 47 | Telehealth | Exercise program | Once | NR | 20 min | Community rehabilitation |
| Qu et al. 56 | Telehealth | Exercise program | Daily | 1.0 MET ‐ <3.0 METS | 15‐45 min | Community rehabilitation |
| Rayegani et al. 58 | NR | Physical activity | 2x per day, 1 h after eating | NR | 15–45 min | NR |
| Righetti et al. 59 | In person | Prone ventilation | Once per day | NR | 12‐16 h | Acute care |
| Ronconi et al. 60 | In person | Prone positioning | Once per day | NR | 12 h | Acute care |
| Head and arm mobilization | NR | Every 4–6 h | ||||
| Sheehy 62 | In person | Strength training | 3× per week, for 6 weeks | 8–12 RM, 1–3 sets | NR | Across continuum |
| Aerobic exercise | Increased to 3–5× per week over time | Start with <3 METs and increase over time | Increased to 20‐30 min over time | |||
| Wang et al., 73 | In‐person | Prone positioning | NR | NR | 2 min | Acute care |
| Stretching | 3× per day | NR | NR | |||
| Yang and Yang 74 | Telehealth | Aerobic exercises | Increase to 3–5× per week | Progressive increase from low intensity | Increase up to 20–30 min | Community rehabilitation |
| Strength training | 2–3× per week | 8–12 RM, 1–3 groups each time; increase load 5%–10% every week | 2 min per group | |||
| Traditional Chinese Medicine | Once per day | NR | 30–50 min | |||
| Abdullahi 105 , 106 | In person | Postural management | Once per day | NR | 12–16 h | Within 72 h of endotracheal intubation |
| Ahmed and Haji 109 | Telehealth | Aerobic exercises | 3–5× per week | Build toward 12–14/20 RPE | Baseline tolerance build to 60 min | At home |
| Resistance training | 2+ days per week | 40%–50% 1 RM, 1–4 sets, 10–15 reps | NR | |||
| Flexibility | 2 days per week | 2–4 reps per muscle group | 10–30 s per stretch | |||
| Cheng et al. 120 , a | Telehealth | Aerobic exercises | 5×+/week | 40%–59% HRR | 30–60 min | At home |
| Resistance training | 2–3 days/week, 48 h intervals | Strength—60% 1 RM, 2‐4 sets, 8‐12 reps | ||||
| Endurance—50% 1 RM, ≤2 sets, 15‐25 reps | ||||||
| Demeco et al. 122 | Telehealth | Aerobic exercises | 3–5× per week | Low intensity with steady increase | 20–30 min | At home |
| Strength training | 2–3× per week for 6 weeks | Weekly intensity increases by 5%–10% | NR |
Recommended for mild COVID with no preexisting risk factors.
Abbreviations: HRR, heart rate reserve; METS, metabolic equivalents; NR, not reported; RM, repetition maximum; RPE, rate of perceived exertion.
Acute care
Thirty‐one articles provided information on what rehabilitation in the acute phase may look like. 4 , 17 , 19 , 20 , 21 , 27 , 29 , 30 , 36 , 40 , 43 , 44 , 46 , 49 , 59 , 60 , 62 , 64 , 66 , 68 , 73 , 105 , 107 , 110 , 118 , 120 , 122 , 123 , 124 , 126 , 130 Four studies identified that rehabilitation in the acute phase would be helpful to mitigate sequelae of COVID but did not provide any additional information regarding the rehabilitation program itself. 3 , 39 , 53 , 75 Nearly all the articles recommended in‐person rehabilitation at the bedside, with one specifying techniques that minimize handling of patients (eg, mechanical assisted limb exercisers, remote controlled mechanical tilting beds). 124
Respiratory rehabilitation was most commonly discussed (n = 18). 19 , 20 , 28 , 29 , 30 , 36 , 40 , 43 , 44 , 46 , 59 , 60 , 62 , 66 , 68 , 73 , 114 , 122 In the acute stage, early mobilization (ie, postural management) was suggested by articles to improve respiratory function and maintain oxygen saturation levels. 4 , 19 , 20 , 28 , 30 , 36 , 40 , 43 , 44 , 46 , 60 , 66 , 68 , 73 , 105 , 107 , 110 , 118 , 126 Articles proposed that for unconscious or sedated patients, passive range of motion mobilization exercises 19 , 20 , 27 , 30 , 110 , 114 , 120 , 126 and electrical muscle stimulation (EMS) 30 , 49 , 59 , 68 , 110 , 114 , 118 could be used in an attempt to counteract deconditioning and immobilization deficits. Airway clearance techniques such as stimulated cough maneuvers and airway suctioning were also discussed in nine studies for those who were on invasive mechanical ventilation. 30 , 36 , 66 , 68 , 73 , 105 , 107 , 114 , 120 These techniques were not recommended for patients with significant bronchial obstruction. 30 One study described exercise training, breathing exercises and chest care and airway secretion for those who were ventilated but had “clear cognitive status” (not defined in article). 120 Further details about articles' recommendations for COVID rehabilitation in the acute care setting can be found in Table 6.
TABLE 6.
Nature and modality of acute‐based COVID rehabilitation
| Nature of rehabilitation | Rehabilitation modality | Rehabilitation to avoid |
|---|---|---|
|
For patients with mild COVID:
For patients with moderate COVID:
For all patients regardless of COVID severity:
|
Postacute care (exact setting unspecified)
It was recommended by all articles that COVID patients receive rehabilitation after discharge from the acute care setting—though a subset did not specify the exact setting. 3 , 28 , 29 , 44 , 64 , 68 , 105 , 110 , 118 , 122 With respect to what a postacute program might look like, details were scarce. Articles suggested that post‐ICU discharge exercise therapy, 28 multimodal physiotherapy treatment 44 and respiratory therapy 3 be prescribed but did not provide further details. For individuals who have functional deficits and physical barriers to discharge (eg, inability to navigate steps to enter home, needing assistance with transfers), continued physical and occupational therapy as well as access to a physiatrist can help with discharge planning and symptom management. 64 Few described a postacute care rehabilitation program in more detail. 29 , 68 , 105 , 118 , 122 These articles focused on respiratory therapy, mobilization and postural management, 29 , 68 strength training, endurance training, balance training, EMS, and chest physiotherapy. 68 , 105 , 118 , 122 Articles recommended that prescribed exercise be of low intensity (<3.0 metabolic equivalents). 68 , 118 Psychological support, nutritional support and ADL guidance was also suggested for this phase of recovery. 68 , 105 , 118 , 122 Finally, it was recommended that the rehabilitation program be tailored based on disease severity. 110
Inpatient rehabilitation
Three of the nine studies that suggested that persons with COVID undergo inpatient rehabilitation did not provide additional details. 38 , 39 , 67 Overall, it was recommended that care be provided by a multidisciplinary team included OTs and PTs. 130 Some articles proposed that rehabilitation programs in the inpatient setting include mobilization, 19 strength training, 19 , 21 , 29 , 48 , 124 endurance training, 21 , 29 , 48 , 74 , 124 and balance exercises 48 , 62 , 74 to help with recovery from deconditioning and generalized weakness. The main goal of rehabilitation discussed for inpatient settings was for the patient to regain enough physical functioning to be independent. 17 , 133 Three of the articles suggested that assessments be done to identify deficits in activities of daily living. 29 , 48 , 62 With respect to respiratory training, only three articles described the use of this type of therapy at this stage. 21 , 62 , 74 One article proposed that oxygen therapy be provided to support COVID patients with chronic pulmonary diseases during exercises. 74 Another suggested that respiratory functioning be assessed and if the muscles are found to be weak, respiratory training could be included. 62 Carda et al 21 recommended breathing training in line with published guidelines for primary lung fibrosis. Other areas of consideration for an inpatient rehabilitation program for COVID included cognitive rehabilitation, 112 smoking cessation, 48 , 74 dietary and nutritional counseling, 18 , 21 , 48 , 74 , 124 psychological support, 21 , 29 , 48 , 62 , 98 , 112 , 124 , 130 and supports to improve quality of life. 48 , 74 One article described the need to address voice or communication impairments. 62 Telerehab was recommended for consultations once approved by a consultant on the unit. 130
Community‐based rehabilitation
A majority of the articles (n = 13) indicated the use of a telehealth‐based program for those requiring rehabilitation upon return to the community. 25 , 27 , 30 , 39 , 40 , 47 , 65 , 67 , 73 , 74 , 104 , 107 , 130 It was recommended that the focus of the telehealth program be on physical functioning, quality of life, and support with returning to community participation. 107 One article argues that telerehab is a better choice for patients at higher risk of COVID mortality, such as immunocompromised individuals and patients with diabetes. 96 Another study recommended the use of apps that provided guidance on completing exercise regimens. 74 With respect to in‐person settings, one article recommended the use of spa facilities to provide community rehabilitation. 111
With respect to what these programs might entail, main areas included exercise training (ie, strength and endurance training), 30 , 40 , 54 , 56 , 74 , 130 diet guidance, 40 , 56 , 74 pulmonary or respiratory rehabilitation, 39 , 54 , 74 , 111 , 130 cognitive rehabilitation, 39 , 54 , 130 and psychological support. 56 , 74 , 130 Few studies (n = 6) discussed the assessment and rehabilitation of psychosocial issues such as quality of life, adjustment to family and social life, return to work, and ADL. 30 , 39 , 40 , 53 , 54 , 56 However, none of these studies described what may be included in this type of program.
Guideline details
A total of 13 guideline documents were included in the review. Each of these outlined an actionable set of recommendations that targeted patients with COVID, 26 , 61 rehabilitation practitioners, 13 , 15 , 16 , 32 , 50 , 72 , 76 , 77 , 139 or policy makers. 52 The guidelines were published by organizations and researchers from the United Kingdom, 16 , 52 , 61 , 72 , 139 Australia, 13 Turkey, 15 Denmark, 26 Canada, 32 , 91 China, 77 and New Zealand. 76
Nature of rehabilitation programs across the continuum
Nearly all of the guidelines (n = 10) suggested that COVID rehabilitation programs be provided by an interdisciplinary team of practitioners including physiatrists, PTs, OTs, SLPs, and dietitians. 13 , 15 , 16 , 32 , 50 , 52 , 61 , 72 , 76 , 77 Guidelines recommended that COVID rehabilitation begin early (ie, as soon as the patient has stable system(s) functioning) and be sustained throughout the patient's recovery and across the continuum of care. 13 , 15 , 16 , 50 , 76 , 77 , 139
Acute care
Guidelines suggested that rehabilitation in the acute care setting focus primarily on respiratory management, mobility, and nutrition. Respiratory management is likely provided by respiratory therapists and SLPs who can help COVID patients resume normal breathing patterns through oxygenation, airway secretion clearance, and ventilation weaning. 32 , 50 , 52 , 76 , 77 PTs and OTs can support early mobility by mitigating the effects of deconditioning using both passive and active range of motion exercises, positioning, and strength training. 32 , 61 , 76 , 77 SLPs are well positioned to support patients' nutrition by screening for malnutrition, addressing swallowing difficulties, and providing appropriate diet and fluid modifications. 50 , 72 , 76
Inpatient rehabilitation
Guidelines suggested that postacute care focus on addressing ongoing impairments in mobility, respiratory function, nutrition, and communication with the goal of promoting independence with activities of daily living. 50 Both mobility and respiratory function can be managed using aerobic exercises that are tailored to patients' abilities (eg, slow jogging, swimming, brisk walking), strength training, and breathing exercises. 76 , 77 Nutritional needs can be monitored in terms of oral intake and muscle function. Specifically, SLPs can help manage swallowing issues and promote communication ability. 72 , 76
Community‐based rehabilitation
Most guidelines recognized that COVID recovery is a complex and ongoing process that will likely extend into the community. 26 , 32 , 50 , 52 , 72 , 76 The suggested goal of community‐based rehabilitation is to optimize COVID patients' functional recovery and quality of life. This entails continuing to provide rehabilitation support to manage respiratory function, mobility, nutrition, and communication (eg, through tailored exercise programs, energy/fatigue management plans, SLP support for diet plans). 32 , 50 , 72 , 76 Importantly, it is recommended that patients be supported and empowered to manage their own health and reintegrate into the community. 72 This can be facilitated by rehabilitation practitioners providing patient education, 50 virtual rehabilitation, 50 home safety assessments. 32 , 50 , 76
Key recommendations (across article types)
Five primary articles, 12 guidelines, and 40 secondary data articles provided recommendations to inform the ongoing rehabilitation response to the COVID pandemic (Table 7).
TABLE 7.
Key recommendations from articles for COVID rehabilitation
| Recommendation area | Details |
|---|---|
| Timing of rehabilitation | |
| Rehabilitation assessment | |
| Rehabilitation provision | |
| Prescribing rehabilitation |
|
| Discharge and community reintegration |
|
Note: Citations bolded correspond to articles reporting primary data. The remaining references correspond to secondary data articles and guidelines.
Barriers and facilitators of COVID rehabilitation provision (across article types)
Factors that act as barriers (Table 8) or facilitators (Table 9) of COVID rehabilitation provision were discussed across primary data articles (n = 7), secondary data articles (n = 42), and guidelines (n = 6).
TABLE 8.
Barriers to providing COVID rehabilitation
| Barriers | Details |
|---|---|
| COVID infectivity |
|
| Patients' health status |
|
| Lack of evidence/guidelines | |
| Personal protective equipment |
|
| Staff‐related issues | |
| Health system issues |
|
Note: Citations bolded correspond to articles reporting primary data. The remaining references correspond to secondary data articles and guidelines.
TABLE 9.
Facilitators of providing COVID rehabilitation
| Facilitators | Details |
|---|---|
| Use of virtual care |
|
| Multidisciplinary teams | |
| Self‐management | |
| Professional development |
|
| Reorganization of unit and staffing |
Note: Citations bolded correspond to articles reporting primary data. The remaining references correspond to secondary data articles and guidelines.
DISCUSSION
The goal of this scoping review was to provide a comprehensive and up‐to‐date synthesis of evidence pertaining to rehabilitation for COVID patients. We included 128 articles, with 26% reporting primary data (n = 33), 64% reporting secondary data (n = 82), and 10% outlining practice/self‐management guidelines (n = 13). A quarter of the included articles came from Italy and China, which were among the first countries to experience and begin responding to the impact of the COVID pandemic.
Rehabilitation programs to meet the needs of patients with COVID
The emerging body of literature on COVID rehabilitation has begun to elucidate the important role that rehabilitation can play in addressing COVID‐related declines in health, function, and well‐being. Most articles agreed that an individualized rehabilitation program be provided across the continuum of care by an interdisciplinary team of professionals and that the nature and extent of rehabilitation be informed by the care setting and COVID severity.
Only a small number of articles (29%) made mention of the psychosocial impacts of COVID (eg, anxiety, depression, posttraumatic stress disorder, reduced quality of life) and very few (5%) presented evidence pertaining to rehabilitation's role in addressing them. 29 , 48 , 62 , 68 , 74 , 107 A number of psychosocial factors (eg, distress, mental health) have been found to be significantly associated with an elevated risk of COVID hospitalization. 140 It is likely that these psychosocial vulnerabilities that predispose individuals to COVID hospitalization are the same vulnerabilities exacerbated post hospitalization. In turn, psychosocial rehabilitation programming warrants further attention. Our review begins to elucidate what psychosocial rehabilitation might entail, including psychological counseling/interventions to address issues such as depression, anxiety, and sleep deprivation 48 , 62 , 68 , 78 ; collaboration between physical medicine and rehabilitation specialists and psychiatrists/psychologists 21 ; and education to promote patients’ participation in valued activities. 62 , 74
None of the articles discussed what community‐based psychosocial rehabilitation should entail or how it should be delivered. Telehealth was widely discussed and endorsed by studies in our review but its potential for providing psychosocial rehabilitation was not considered. Telehealth and computer‐mediated consultations with other chronic illness populations have been shown to be beneficial and to foster closeness and communication amongst care providers, patients, and families. 141 Although telerehab interventions have been demonstrated to be comparable in effectiveness to in‐person therapy with other disease populations such as stroke, 142 , 143 they disproportionately focus on physical recovery and have been underused to provide social support to patients and their family caregivers in the community setting. 142 To this end, we suggest that telehealth and other virtual care modalities have high potential for facilitating outpatient counseling and education to community‐residing COVID patients. Rehabilitation professionals can also leverage virtual modalities to facilitate peer‐led support and education for COVID patients. Despite peer support being recognized as an important aspect of psychosocial rehabilitation, 144 it was not discussed by studies in our review. Peer support has been demonstrated to promote community reintegration in other patient populations 145 and may be particularly beneficial for COVID patients who are already reporting that online groups are a valuable source of experiential knowledge and support—especially in the absence of other community/home care services. 146
Adaptations to enable the provision of COVID rehabilitation
Several of the adaptations and facilitators we identified directly resolved issues that challenged the provision of COVID rehabilitation. For example, modifying physical spaces, schedules, and teams was done to limit the spread of COVID and to address PPE shortages. Providing professional development opportunities was considered one way of addressing staff wellness and burnout. These solution‐oriented adaptations should continue to be optimized so as to break down barriers to rehabilitation provision.
Notably, three aspects identified as challenging the provision of COVID care were not explicitly addressed by any of the adaptations or facilitators: (1) the paucity of evidence and guidelines for COVID rehabilitation, (2) patients' health status, and (3) health system issues. The first two issues are interconnected as the variability in COVID severity and impact has made it difficult to establish eligibility criteria and to generate a broad rehabilitation prescription. At a minimum, articles in our review recommend that eligibility criteria entail (1) negative COVID status (as determined by two negative nasal swabs or patient being 7+ days from diagnosis), (2) stability in respiratory and cardiovascular function as well as general health parameters (eg, stable oxygen saturation, no fever), and (3) functional need (one article suggested rehabilitation need be determined by a functional independence measure [FIM] score of <100). 29 As mentioned earlier, the rehabilitation prescription itself is best tailored to each patient to ensure that it holistically meets individual needs.
The health system issues we identified centered on poor system coordination that limited the continuity of COVID rehabilitation across the care continuum. Challenges with rehabilitation continuity—especially as patients transition back to the community—are not new. 147 However, several aspects of the COVID pandemic exacerbate these challenges (eg, physical distancing restrictions, closing outpatient services, and early discharge from inpatient rehabilitation), suggesting that a multipronged approach is needed. Many actionable strategies to promote COVID rehabilitation continuity can be leveraged from articles in our review and adapted from research that has focused on maintaining rehabilitation for non‐COVID patients in the wake of the pandemic. These include (1) capitalizing on telemedicine to provide remote rehabilitation 130 , 148 , 149 —particularly using accessible tools such as Skype, FaceTime, and Zoom without penalty to health care providers for noncompliance with privacy regulations 149 ; (2) creating strong partnerships with home care 130 and ensuring that rehabilitation services are viewed as “essential” —particularly for those returning to congregate care settings where lockdowns may restrict nonessential care 148 ; and (3) ensuring that health care providers can bill and/or be reimbursed for telehealth visits using appropriate billing codes and in a streamlined way that does not detract from their time with patients. 4 , 65 , 149 It is important to note that these suggestions will not universally apply to health systems and organizations across geographic boundaries. In turn, they should be adapted to countries' national and regional contexts and health system capacities.
Future directions
Many aspects of COVID rehabilitation were difficult to summarize across articles given the vast variability in reporting. Thus, there is a need for more consistent reporting to ensure that future studies can be meaningfully aggregated to inform COVID rehabilitation programming and evaluation. Based on our review, we suggest standardized reporting parameters for the following data elements: patient populations, rehabilitation admission, service adaptations, and rehabilitation programming. For patient populations, capturing demographic information such as age, gender, hospital/ICU/rehabilitation LOS, comorbidities, and COVID sequelae would provide important contextual information and enable detailed program evaluations. There was not a great deal of consistency in rehabilitation admission criteria reported but, at a minimum, our review elucidates that COVID status at admission, respiratory function (eg, oxygen saturation), and functional ability (eg, using the FIM) should be outlined. Some degree of consistency was observed in the reporting of adaptations to enable COVID rehabilitation according to the broad categories of modifications to physical space, staffing, scheduling, and communication modalities/procedures. Although information pertaining to rehabilitation programming was inconsistently reported across articles, we were able to extract data from at least one article for each of the following categories and thus suggest them as a good starting point for more streamlined reporting: (1) timing (ie, when program was initiated), (2) duration (ie, duration from start to end of program), (3) frequency, (4) modality (eg, bedside, virtual), (5) setting (ie, acute care, ICU, inpatient/outpatient/community rehabilitation), and (6) content (ie, rehabilitation disciplines involved, number of rehabilitation professionals involved, specific therapies provided).
The role of families in supporting COVID patients' rehabilitation and recovery was not a focus of any articles included in our review. This is potentially because of ongoing public health restrictions that limit the physical presence of families for hospitalized patients. 150 However, it has been pointed out that physical restrictions on family presence should not undermine family‐centered care efforts. 150 Distressing times like those experienced during the pandemic intensify patients' need to feel safe and connected to their loved ones, 151 making family‐centered rehabilitation more important now than ever. Like other complex illnesses, COVID leads to a large and diverse set of needs requiring active participation and support from families. 152 Family‐centered COVID rehabilitation ensures the involvement of both patients and families in treatment planning and can thus facilitate the individualized type of rehabilitation that COVID patients need. 153 Several strategies for engaging families in the overall care of COVID patients can be adapted and implemented in the rehabilitation setting. These include (1) facilitating synchronous patient‐family communication (eg, using videoconferencing) as well as asynchronous engagement (eg, prerecorded videos, pictures, patient journaling), (2) ensuring environmental familiarity for patients (eg, arranging for family to bring in objects from home) and describing this environment to families, and (4) prioritizing family‐care provider communication (eg, establishing a family communication plan, daily videoconferencing). 151 Engaging families early on when COVID patients are in hospital can enable smoother transitions to home and greater continuity in care. 153
Sociocultural factors were considered by only one article in our review, 116 highlighting the need for further investigation into their impact on COVID rehabilitation provision and outcomes. For example, those with lower socioeconomic status (SES) may have reduced access to telerehab, which may differentially affect their recovery and other outcomes). Future research should capture variations in age, race, gender, and SES as it is becoming increasingly apparent that COVID disproportionately affects older adults, people of color, women, and those with lower SES. 154 , 155 , 156
Our review identified only one qualitative study pertaining to COVID rehabilitation. Qualitative approaches are an important complement to epidemiological and clinical research and can provide insight into behaviors and perceptions. 157 In the context of COVID rehabilitation research, qualitative approaches can elucidate stakeholders' (eg, patients, families, care providers) lived experiences with rehabilitation care and recovery, thereby moving us beyond the “what” of COVID rehabilitation (eg, what aspects of rehabilitation to provide? what outcomes to measure?) to the “why” and “how” (eg, why are certain aspects of a rehabilitation program beneficial? How do the unique circumstances of COVID patients and families influence care needs and experiences?). 157
STRENGTHS AND LIMITATIONS
To the best of our knowledge, this is the first scoping review to systematically identify and synthesize a diverse set of evidence sources (ie, primary data, secondary data, guidelines) pertaining to rehabilitation for COVID patients. Our comprehensive synthesis of 128 articles has the potential to provide rehabilitation practitioners with a range of evidence to support their ongoing response to the COVID pandemic. Although the authors have expertise in scoping review conduct, the present review may have been strengthened by an academic librarian designing and deploying the search strategy. The search strategy did not include any terms explicitly related to psychological rehabilitation, which may account to some extent for the lack of data on psychosocial rehabilitation programming for COVID patients. Given that this review was conducted during the early stages of the COVID pandemic, the large majority (74%) of articles we included reported only secondary data (eg, reviews, opinion papers). As such, we were limited in our ability to synthesize primary evidence and make recommendations based on real‐world data that capture COVID rehabilitation “in action.”
CONCLUSION
It is clear that rehabilitation will need to play an important role in the recovery of COVID patients, many of whom have long‐lasting symptoms that do not permit return to full community participation. Research to date has begun to elucidate the criteria that can be used to identify patients for rehabilitation as well as the nature, extent, timing, and mode of this rehabilitation. However, a large majority of articles reported secondary data, underscoring that we know little about actual COVID patients receiving rehabilitation, the rehabilitation program itself, and the effectiveness of COVID rehabilitation across the continuum of care. Organization‐ and system‐level adaptations have the potential to facilitate COVID rehabilitation delivery by mitigating barriers to rehabilitation provision. Additionally, engaging families in COVID rehabilitation may serve to optimize the continuity of care for patients. Future research should prioritize the reporting of primary data and subsequently the synthesis of studies reporting on the effectiveness of rehabilitation interventions as they are developed and delivered over time.
Supporting information
Appendix S1. Supporting Information
Wasilewski MB, Cimino SR, Kokorelias KM, Simpson R, Hitzig SL, Robinson L. Providing rehabilitation to patients recovering from COVID‐19: A scoping review. PM&R. 2022;14(2):239-258. 10.1002/pmrj.12669
REFERENCES
- 1. Jaime CY, McIntyre M, Dow H, Robinson L, Winston P. Changes to rehabilitation service delivery and the associated physician perspectives during the COVID‐19 pandemic: a mixed methods needs assessment study. Am J Phys Med Rehabil. 2020;99(9):775‐782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mahase E. Covid‐19: what do we know about “long covid”? BMJ. 2020;370:360. [DOI] [PubMed] [Google Scholar]
- 3. Coraci D, Fusco A, Frizziero A, Giovannini S, Biscotti L, Padua L. Global approaches for global challenges: the possible support of rehabilitation in the management of COVID‐19. J Med Virol. 2020;92:1739‐1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID‐19 infection. Am J Phys Med Rehabil. 2020;99(6):470‐474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thornton J. Covid‐19: the challenge of patient rehabilitation after intensive care. BMJ. 2020;369:369. [DOI] [PubMed] [Google Scholar]
- 6. Grabowski DC, Maddox KEJ. Postacute care preparedness for COVID‐19: thinking ahead. JAMA. 2020;323(20):2007‐2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rathore FA, Gosney JE, Reinhardt JD, Haig AJ, Li J, DeLisa JA. Medical rehabilitation after natural disasters: why, when, and how? Arch Phys Med Rehabil. 2012;93(10):1875‐1881. [DOI] [PubMed] [Google Scholar]
- 8. Phillips M, Turner‐Stokes L, Wade D, Walton K. Rehabilitation in the Wake of Covid‐19‐A Phoenix from the Ashes. London, UK; British Society of Rehabilitation Medicine (BSRM); 2020. [Google Scholar]
- 9. Pattanakuhar S, Suksathien R, Thirapatarapong W. Recommendations for preparedness of medical rehabilitation services in Thailand during COVID‐19 outbreak. ASEAN J Rehabil Med. 2020;30(1):2‐7. [Google Scholar]
- 10. Gitkind AI, Levin S, Dohle C, et al. Redefining pathways into acute rehabilitation during the COVID‐19 crisis. Phys Med Rehabil. 2020;12(8):837‐841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arksey H, O'malley L. Scoping Studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19‐32. [Google Scholar]
- 12. Khan KS, ter Riet G, Glanville J, Sowden AJ, Kleijnen J. Undertaking systematic reviews of research on effectiveness: CRD's guidance for carrying out or commissioning reviews. 2001;4. 2nd edition. NHS Centre for Reviews and Dissemination. [Google Scholar]
- 13. Amatya B, Khan F. Rehabilitation response in pandemics. Am J Phys Med Rehabil. 2020;99(8):663‐668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Andrenelli E, Negrini F, De Sire A, Arienti C, Patrini M, Negrini S. Systematic rapid living review on rehabilitation needs due to Covid‐19: update to May 31st 2020. Eur J Phys Rehabil Med. 2020;56(3):347–353. [DOI] [PubMed] [Google Scholar]
- 15. Aytür YK, Köseoğlu BF, Taşkıran, et al. Pulmonary rehabilitation principles in SARS‐COV‐2 infection (COVID‐19): a guideline for the acute and subacute rehabilitation. Turk J Phys Med Rehabil. 2020;66(2):104‐120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Barker‐Davies RM, O'Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post‐COVID‐19 rehabilitation. Br J Sports Med. 2020;54:949‐959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bij de Vaate E, KHL G, Goossens PH. Personalized recovery of severe COVID19: rehabilitation from the perspective of patient needs. Eur J Clin Invest. 2020; Epub ahead of print: e13325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brugliera L, Spina A, Castellazzi P, et al. Nutritional management of COVID‐19 patients in a rehabilitation unit. Eur J Clin Nutr. 2020;74(6):860‐863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brugliera L, Spina A, Castellazzi P, et al. Rehabilitation of COVID‐19 patients. J Rehabil Med. 2020;52(4):1‐3. [DOI] [PubMed] [Google Scholar]
- 20. Candan SA, Elibol N, Abdullahi A. Consideration of prevention and management of long‐term consequences of post‐acute respiratory distress syndrome in patients with COVID‐19. Physiother Theory Pract. 2020;36(6):663‐668. [DOI] [PubMed] [Google Scholar]
- 21. Carda S, Invernizzi M, Bavikatte G, et al. COVID‐19 pandemic. What should PRM specialists do? A clinician's perspective. Eur J Phys Rehabil Med. 2020;56(4):515–524. [DOI] [PubMed] [Google Scholar]
- 22. Chen J‐M, Wang Z‐Y, Chen Y‐J, Ni J. The Application of eight‐segment pulmonary rehabilitation exercise in people with Coronavirus disease 2019. Front Physiol. 2020;11:646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. National Post‐Intensive Care Rehabilitation Collaborative . Responding to COVID‐19 and Beyond: A Framework for Assessing Early Rehabilitation Needs Following Treatment in Intensive Care. London, UK; British Society of Rehabilitation Medicine; 2020. [Google Scholar]
- 24. Curci C, Pisano F, Bonacci E, et al. Early rehabilitation in post‐acute COVID‐19 patients: data from an Italian COVID‐19 rehabilitation unit and proposal of a treatment protocol. A cross‐sectional study. Eur J Phys Rehabil Med. 2020;56(5):633–641. [DOI] [PubMed] [Google Scholar]
- 25. De Biase S, Cook L, Skelton DA, Witham M, Ten Hove R. The COVID‐19 Rehabilitation Pandemic. Age Ageing. 2020;49(5):696‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. World Health Organization Regional Office for Europe . Support for Rehabilitation Self‐Management after COVID‐19 Related Illness. Copenhagen, Denmark: World Health Organization; 2020. [Google Scholar]
- 27. Falvey JR, Ferrante LE. Flattening the disability curve: rehabilitation and recovery after COVID‐19 infection. Heart Lung. 2020;49(5):440‐441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hoenig H, Koh G. Response to letter regarding "How Should the Rehabilitation Community Prepare for 2019‐nCoV?". Arch Phys Med Rehabil. 2020;101(8):1471‐1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Iannaccone S, Castellazzi P, Tettamanti A, et al. Role of rehabilitation Department for Adult Individuals With COVID‐19: the Experience of the San Raffaele Hospital of Milan. Arch Phys Med Rehabil. 2020;101(9):1656‐1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kalirathinam D, Guruchandran R, Subramani P. Comprehensive physiotherapy management in COVID‐19—A narrative review. Sci Med. 2020;30(1):e‐38030. [Google Scholar]
- 31. Kalra A, Kantroo V. Clinical tools for cardiorespiratory assessment and rehabilitation: a primary care perspective. J Pak Med Assoc. 2020;70(Suppl 3):S56‐S59. [DOI] [PubMed] [Google Scholar]
- 32. COVID‐19 Scientific Advisory Group . COVID‐19 Scientific Advisory Group Rapid Evidence Report. Canada: Alberta; 2020. [Google Scholar]
- 33. Karamouzos V, Fligou F, Gogos C, Velissaris D. High flow nasal cannula oxygen therapy in adults with COVID‐19 respiratory failure. A case report. Monaldi Arch Chest Dis. 2020;90(2). [DOI] [PubMed] [Google Scholar]
- 34. Kemp HI, Corner E, Colvin LA. Chronic pain after COVID‐19: implications for rehabilitation. Br J Anaesth. 2020;125(4):436‐440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Khan F, Amatya B. Medical rehabilitation in pandemics: towards a new perspective. J Rehabil Med. 2020;52(4):1‐4. [DOI] [PubMed] [Google Scholar]
- 36. Lazzeri M, Lanza A, Bellini R, et al. Respiratory physiotherapy in patients with COVID‐19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis. 2020;90(1). [DOI] [PubMed] [Google Scholar]
- 37. Leochico CFD. Adoption of telerehabilitation in a developing country before and during the COVID‐19 pandemic. Ann Phys Rehabil Med. 2020;63(6):563–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Levy J, Leotard A, Lawrence C, et al. A model for a ventilator‐weaning and early rehabilitation unit to deal with post‐ICU impairments with severe COVID‐19. Ann Phys Rehabil Med. 2020;63(4):376–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lew HL, Oh‐Park M, Cifu DX. The War on COVID‐19 Pandemic: role of Rehabilitation Professionals and Hospitals. Am J Phys Med Rehabil. 2020;99(7):571‐572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zeng B, Chen D, Qiu Z, et al. Expert consensus on protocol of rehabilitation for COVID‐19 patients using framework and approaches of WHO International Family Classifications. Aging Med. 2020;3(2):82‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID‐19: a randomized controlled study. Complement Ther Clin Pract. 2020;39:101166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lopez M, Bell K, Annaswamy T, Juengst S, Ifejika N. COVID‐19 guide for the rehabilitation clinician: a review of non‐pulmonary manifestations and complications. Am J Phys Med Rehabil. 2020;99(8):669‐673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mammi P, Ranza E, Petraglia F, et al. In response to: Simpson R and Robinson L: rehabilitation following critical illness in people with COVID‐19 infection. Am J Phys Med Rehabil. 2020;99(8):679‐680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Masiero S, Zampieri D, Del Felice A. The place of early rehabilitation in ICU for Covid‐19. Am J Phys Med Rehabil. 2020;99(8):677‐687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. McNeary L, Maltser S, Verduzco‐Gutierrez M. Navigating Coronavirus Disease 2019 (Covid‐19) in Physiatry: a CAN report for inpatient rehabilitation facilities. Phys Med Rehabil. 2020;12(5):512‐515. [DOI] [PubMed] [Google Scholar]
- 46. Mohan R, Mohapatra B. Shedding light on Dysphagia associated with COVID‐19: the What and Why. OTO Open. 2020;4(2):2473974X20934770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mukaino M, Tatemoto T, Kumazawa N, et al. Staying active in isolation: Telerehabilitation for individuals with the severe acute respiratory syndrome Coronavirus 2 infection. Am J Phys Med Rehabil. 2020;99(6):478‐479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Mureddu GF, Ambrosetti M, Venturini E, et al. Cardiac rehabilitation activities during the COVID‐19 pandemic in Italy. Position Paper of the AICPR (Italian Association of Clinical Cardiology, Prevention and Rehabilitation). Monaldi Arch Chest Dis. 2020;90(2). [DOI] [PubMed] [Google Scholar]
- 49. Nakamura K, Nakano H, Naraba H, Mochizuki M, Hashimoto H. Early rehabilitation with dedicated use of belt‐type electrical muscle stimulation for severe COVID‐19 patients. Crit Care. 2020;24(1):342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Pan American Health Organization . Rehabilitation Considerations during the COVID‐19 Outbreak. Washington, D.C., USA: 8 Apr; World Health Organization (WHO); 2020. [Google Scholar]
- 51. Pancera S, Galeri S, Porta R, et al. Feasibility and Efficacy of the Pulmonary Rehabilitation Program in a Rehabilitation Center: case Report of a Young Patient Developing Severe Covid‐19 Acute Respiratory Distress Syndrome. J Cardiopulm Rehabil Prev. 2020;40(4):205‐208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chartered Society of Physiotherapy . Rehabilitation and COVID‐19—CSP Policy Statement. London, UK; Chartered Society of Physiotherapy; 2020. [Google Scholar]
- 53. Pinto TF, CRFd C. SARS CoV‐2 (COVID‐19): lessons to be learned by Brazilian Physical Therapists. Braz J Phys Ther. 2020;24(3):185‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Polastri M, Nava S, Clini E, Vitacca M, Gosselink R. COVID‐19 and pulmonary rehabilitation: preparing for phase three. Eur Respir J. 2020;55(6):2001822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Poussardin C, Oulehri W, Isner ME, Mertes PM, Collange O. In‐ICU COVID‐19 patients' characteristics for an estimation in post‐ICU rehabilitation care requirement. Anaesth Crit Care Pain Med. 2020;39(4):479‐480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Qu J‐M, Wang C, Cao B. Guidance for the management of adult patients with coronavirus disease 2019. Chin Med J. 2020;133(13):1575‐1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ramachandran S. A junior doctor's experience of critical illness: from treating patients to becoming a patient with COVID‐19. Anaesth Rep. 2020;8(1):59‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rayegani SM, Raeissadat SA, Fakharian A, et al. Role of rehabilitation medicine in the COVID‐19 pandemic: an Iranian consensus. Eur J Phys Rehabil Med. 2020:309–310. [DOI] [PubMed] [Google Scholar]
- 59. Righetti RF, Onoue MA, Politi FVA, et al. Physiotherapy care of patients with Coronavirus Disease 2019 (COVID‐19)—A Brazilian experience. Clinics. 2020;75:e2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ronconi G, Ferrara PE, Codazza S, Cerulli S. Is the rehabilitation ready for COVID‐19 patients' care? Minerva Med. 2020. [DOI] [PubMed] [Google Scholar]
- 61. Ross D, Allport F, Carter R, et al. COVID‐19 Patient Rehabilitation Booklet—Information for Patients. Leeds, UK; National Health Service (NHS); 2020. [Google Scholar]
- 62. Sheehy LM. Considerations for Postacute Rehabilitation for Survivors of COVID‐19. JMIR Public Health Surveill. 2020;6(2):e19462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Simonelli C, Paneroni M, Fokom AG, et al. How the COVID‐19 infection tsunami revolutionized the work of respiratory physiotherapists: an experience from Northern Italy. Monaldi Arch Chest Dis. 2020;90(2). [DOI] [PubMed] [Google Scholar]
- 64. Smith SR, Jenq G, Claflin T, Magnant C, Haig AJ, Hurvitz E. Proposed Workflow for Rehabilitation in a Field Hospital Setting during the COVID‐19 Pandemic. Phys Med Rehabil. 2020;12:823‐828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Stein J, Visco CJ, Barbuto S. Rehabilitation Medicine Response to the COVID‐19 Pandemic. Am J Phys Med Rehabil. 2020;99(7):573‐579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Thomas P, Baldwin C, Bissett B, et al. Physiotherapy management for COVID‐19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Tur BS, Evcik D. Is physical medicine and rehabilitation needed much more for COVID‐19 pandemic? Turk J Phys Med Rehabil. 2020;66(2):101‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Vitacca M, Carone M, Clini EM, et al. Joint Statement on the Role of Respiratory Rehabilitation in the COVID‐19 Crisis: the Italian Position Paper. Respiration. 2020;99(6):493‐499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Vitacca M, Lazzeri M, Guffanti E, et al. Italian suggestions for pulmonary rehabilitation in COVID‐19 patients recovering from acute respiratory failure: results of a Delphi process. Monaldi Arch Chest Dis. 2020;90(2). [DOI] [PubMed] [Google Scholar]
- 70. Wade DT. Rehabilitation after COVID‐19: an evidence‐based approach. Clin Med. 2020;20:359‐365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wainwright TW, Low M. Beyond acute care: why collaborative self‐management should be an essential part of rehabilitation pathways for COVID‐19 patients. J Rehabil Med. 2020;52(5):1‐2. [DOI] [PubMed] [Google Scholar]
- 72. Wallace S, Behenna K, Bolton L, et al. COVID‐19 Speech and Language Therapy Rehabilitation Pathway. London, UK; Royal College of Speech & Language Therapists; 2020. [Google Scholar]
- 73. Wang TJ, Chau B, Lui M, Lam G‐T, Lin N, Humbert S. PM&R and Pulmonary Rehabilitation for COVID‐19. Am J Phys Med Rehabil. 2020;99(9):769‐774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Yang L‐L, Yang T. Pulmonary Rehabilitation for Patients with Coronavirus Disease 2019 (COVID‐19). Chronic Dis Transl Med. 2020;6(2):79‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Yu P, Wei Q, He C. Early rehabilitation for critically Ill patients with COVID‐19: more benefits than risks. Am J Phys Med Rehabil. 2020;99(6):468‐469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ministry of Health and Allied Health Aotearoa New Zealand . Guidance for the Rehabilitation of People with or Recovering from COVID‐19 in Aotearoa New Zealand. Wellington, New Zealand; Ministry of Health and Allied Health Aotearoa New Zealand; 2020. [Google Scholar]
- 77. Zhao H‐M, Xie Y‐X, Wang C. Recommendations for respiratory rehabilitation in adults with COVID‐19. Chin Med J. 2020;133(13):1595‐1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zhu C, Wu Y, Liu H, Ban Y, Ma X, Zhang Z. Early pulmonary rehabilitation for SARS‐CoV‐2 pneumonia: experience from an intensive care unit outside of the Hubei province in China. Heart Lung. 2020;49(5):449‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Negrini F, Ferrario I, Mazziotti D, et al. Neuropsychological features of severe hospitalized COVID‐19 patients at clinical stability and clues for post‐acute rehabilitation. Arch Phys Med Rehabil. 2020;102(1):155–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. McWilliams D, Weblin J, Hodson J, Veenith T, Whitehouse T, Snelson C. Rehabilitation levels in COVID‐19 patients admitted to intensive care requiring invasive ventilation: an observational study. Ann Am Thorac Soc. 2020;18(1):122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ng JA, Miccile LA, Iracheta C, et al. Prone positioning of patients with acute respiratory distress syndrome related to COVID‐19: a Rehabilitation‐Based Prone Team. Phys Ther. 2020;100(10):1737‐1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Rosen K, Patel M, Lawrence C, Mooney B. Delivering telerehabilitation to COVID‐19 Inpatients: a retrospective chart review suggests it is a viable option. HSS J. 2020;16(Suppl 1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Shan MX, Tran YM, Vu KT, Eapen BC. Postacute inpatient rehabilitation for COVID‐19. BMJ Case Rep. 2020;13(8):e237406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Stierli S, Buss I, Redecker H, et al. Insights from an interprofessional post‐COVID‐19 rehabilitation unit: a speech and language therapy and respiratory medicine perspective. J Rehabil Med. 2020;52(9):1‐4. [DOI] [PubMed] [Google Scholar]
- 85. Suzuki E, Sakai T, Hoshino C, Hirao M, Yamaguchi R, Nakahara R. Assessment of the need for early initiation of rehabilitation treatments in patients with Coronavirus Disease 2019. Prog Rehabil Med. 2020;5:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Steere HK, Polich G, Silver JK, et al. Ambulatory rehabilitation of patients hospitalized with SARS CoV‐2 Infections: early pandemic experience in New York City and Boston. Phys Med Rehabil. 2020. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Tay SS, Neo E Jr, Tan MM, Tan PL. Post‐critical care COVID‐19 patient benefits from a robotic patient‐guided suspension system for pulmonary rehabilitation. Ann Acad Med Singapore. 2020;49(6):401‐404. [PubMed] [Google Scholar]
- 88. Wootton SL, King M, Alison JA, Mahadev S, Chan ASL. COVID‐19 rehabilitation delivered via a telehealth pulmonary rehabilitation model: a case series. Respirol Case Rep. 2020;8(8):e00669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Zha L, Xu X, Wang D, Qiao G, Zhuang W, Huang S. Modified rehabilitation exercises for mild cases of COVID‐19. Ann Palliative Med. 2020;9(5):3100‐3106. [DOI] [PubMed] [Google Scholar]
- 90. Roman‐Belmonte JM, De La Corte‐Rodriguez H, Rodriguez‐Merchan EC, La Torre EMD, Vazquez‐Sasot A. Strengthening with blood flow restriction: can it be a useful option in the rehabilitation of patients with coronavirus? Arch Bone Jt Surg. 2020;8(4):552‐555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Namasivayam‐MacDonald AM, Riquelme LF. Speech‐language pathology management for adults with COVID‐19 in the acute hospital setting: initial recommendations to guide clinical practice. Am J Speech Lang Pathol. 2020;29(4):1‐16. [DOI] [PubMed] [Google Scholar]
- 92. Odonkor CA, Sholas MG, Verduzco‐Gutierrez M, Zafonte RD, Silver JK. African American Patient Disparities in COVID‐19 Outcomes: a call to action for physiatrists to provide rehabilitation care to black survivors. Am J Phys Med Rehabil. 2020;99(1):986‐987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Papathanassoglou E, Pohar Manhas K, Kusi‐Appiah E. Beyond acute respiratory distress: multiple organ effects and early rehabilitation in COVID‐19. CONNECT: The World of Critical Care Nursing. 2020;13:155‐161. [Google Scholar]
- 94. Pincherle A, Johr J, Pancini L, et al. Intensive care admission and early neuro‐rehabilitation. Lessons for COVID‐19? Front Neurol. 2020;11:880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Sivan M, Halpin S, Hollingworth L, Snook N, Hickman K, Clifton IJ. Development of an integrated rehabilitation pathway for individuals recovering from COVID‐19 in the community. J Rehabil Med. 2020;52(8):1‐5. [DOI] [PubMed] [Google Scholar]
- 96. Shah SZA, Nasb M, Lu M, Huang L, Wang Y, Chen H. Scaling the need, benefits, and risks associated with COVID‐19 acute and postacute care rehabilitation: a review. Rehabil Res Pract. 2020;2020:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Rooney S, Webster A, Paul L. Systematic review of changes and recovery in physical function and fitness after severe acute respiratory syndrome–Related Coronavirus infection: implications for COVID‐19 rehabilitation. Phys Ther. 2020;100(10):1717‐1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Sun T, Guo L, Tian F, et al. Rehabilitation of patients with COVID‐19. Expert Rev Respir Med. 2020;14(12):1249‐1256. [DOI] [PubMed] [Google Scholar]
- 99. Uppal H, Rai S. Role of rehabilitation during COVID‐19 pandemic: an Indian perspective. Disaster Med Public Health Prep. 2020;1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Valenzuela PL, Joyner M, Lucia A. Early mobilization in hospitalized patients with COVID‐19. Am J Phys Med Rehabil. 2020;63(4):384‐385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Vergara J, Skoretz SA, Brodsky MB, et al. Assessment, diagnosis, and treatment of Dysphagia in paitents infected with SARS‐CoV‐2: a review of the Literature and International Guidelines. Am J Speech Lang Pathol. 2020;29(4):2242‐2253. [DOI] [PubMed] [Google Scholar]
- 102. Yonter SJ, Alter K, Bartels MN, et al. What now for rehabilitation specialists? Coronavirus Disease 2019 (COVID‐19) Questions and Answers. Arch Phys Med Rehabil. 2020;101:2233‐2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Zhu Y, Wang Z, Zhou Y, et al. Summary of respiratory rehabilitation and physical therapy guidelines for patients with COVID‐19 based on recommendations of World Confederation for Physical Therapy and National Association of Physical Therapy. J Phys Ther Sci. 2020;32(8):545‐549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Salawu A, Green A, Crooks MG, Brixey N, Ross DH, Sivan M. A proposal for multidisciplinary tele‐rehabilitation in the assessment and rehabilitation of COVID‐19 survivors. Int J Environ Res Public Health. 2020;17(13):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Abdullahi A. Safety and efficacy of chest physiotherapy in patients with COVID‐19: a critical review. Front Med. 2020;7:454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Abdullahi A, Bello B, Mukhtar NB, et al. Physiotherapy management of COVID‐19 in Africa: ongoing efforts, challenges, and future directions. Physiother Theory Pract. 2020;36(8):871‐872. [DOI] [PubMed] [Google Scholar]
- 107. Adhikari SP, Dev R, Sandborgh M. Alternatives to routinely used physiotherapy interventions for achieving maximum patients' benefits and minimising therapists' exposure in treatment of COVID‐19‐a commentary. Eur J Physiother. 2020;22:373‐378. [Google Scholar]
- 108. Ahmed I. Covid‐19: prioritising rehabilitation when mortality figures dominate the headlines. BMJ. 2020;370:m3381. [DOI] [PubMed] [Google Scholar]
- 109. Ahmed I, Haji G. COVID‐19—Is it time for exercise clinicians to prehabilitate "high risk" respiratory patients? Curr Sports Med Rep. 2020;19(8):281‐283. [DOI] [PubMed] [Google Scholar]
- 110. Ambrosino P, Papa A, Maniscalco M, Di Minno MND. COVID‐19 and functional disability: current insights and rehabilitation strategies. Postgraduate Med J. 2020;469‐470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Antonelli M, Donelli D. Respiratory rehabilitation for post‐COVID19 patients in spa centers: first steps from theory to practice. Int J Biometeorol. 2020;64(10):1811‐1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Arenivas A, Carter KR, Harik LM, Hays KM. COVID‐19 neuropsychological factors and considerations within the acute physical medicine and rehabilitation setting. Brain Inj. 2020;34(8):1136‐1137. [DOI] [PubMed] [Google Scholar]
- 113. Asly M, Hazim A. Rehabilitation of post‐covid‐19 patients. Pan Afr Med J. 2020;36:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Battaglini D, Robba C, Caiffa S, et al. Chest physiotherapy: an important adjuvant in critically ill mechanically ventilated patients with COVID‐19. Respir Physiol Neurobiol. 2020;282:103529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Beom J, Jung J, Hwang I‐C, et al. Early rehabilitation in a critically ill inpatient with coronavirus disease 2019: a case report. Eur J Phys Rehabil Med. 2020;6(6):858–861. [DOI] [PubMed] [Google Scholar]
- 116. Brown DA, O'Brien KK, Josh J, et al. Six lessons for COVID‐19 rehabilitation From HIV rehabilitation. Phys Ther. 2020;100(11):1906‐1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Brugliera L, Spina A, Castellazzi P, et al. Rehabilitative of COVID‐19 patients with acute lower extremity Ischemia and amputation. J Rehabil Med. 2020;52(9):jrm00094. [DOI] [PubMed] [Google Scholar]
- 118. Candemir I, Ergun P. COVID‐19 infections and pulmonary rehabilitation. Tuberk Toraks. 2020;68(2):192‐194. [DOI] [PubMed] [Google Scholar]
- 119. Cavalagli A, Peiti G, Conti C, Penati R, Vavassori F, Taveggia G. Cranial nerves impairment in post‐acute oropharyngeal Dysphagia after COVID‐19: a case report. Eur J Phys Rehabil Med. 2020;56(6):853–857. [DOI] [PubMed] [Google Scholar]
- 120. Cheng Y‐Y, Chen C‐M, Huang W‐C, et al. Rehabilitation programs for patients with COronaVIrus Disease 2019: consensus statements of Taiwan Academy of Cardiovascular and Pulmonary Rehabilitation. J Formos Med Assoc. 2020;120(1 Pt 1):83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Curci C, Pisano F, Negrini F, De Sire A. Which are the main assessment tools of functional capacity in post‐acute COVID‐19 patients admitted to Rehabilitation Units? Eur J Phys Rehabil Med. 2020. Epub ahead of print. [Google Scholar]
- 122. Demeco A, Marotta N, Barletta M, et al. Rehabilitation of patients post‐COVID‐19 infection: a literature review. J Int Med Res. 2020;48(8):300060520948382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Exum E, Hull BL, Lee ACW, Gumieny A, Villarreal C, Longnecker D. Applying telehealth technologies and strategies to provide acute care consultation and treatment of patients with confirmed or possible COVID‐19. J Acute Care Phys Ther. 2020;11(3):103‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Gautam AP, Arena R, Dixit S, Borghi‐Silva A. Pulmonary rehabilitation in COVID‐19 pandemic era: the need for a revised approach. Respirology. 2020;25(12):1320‐1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Grigoletto I, Cavalheri V, Lima FF, Ramos EMC. Recovery after COVID‐19: the potential role of pulmonary rehabilitation. Braz J Phys Ther. 2020;24:463‐464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Jangra M, Saxena A. Significance of physiotherapy in "SARS‐CoV‐2/COVID‐19: an Epidemic". Ann Thorac Med. 2020;15(3):179‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Jiandani MP, Salagre SB, Kazi S, et al. Preliminary observations and experiences of physiotherapy practice in acute care setup of COVID 19: a retrospective observational study. J Assoc Physicians India. 2020;68(10):18‐24. [PubMed] [Google Scholar]
- 128. Jiang Y, Chen J, Cen F, et al. Importance of respiratory airway management as well as psychological and rehabilitative treatments to COVID‐19 patients. Am J Emerg Med. 2020;38(8):1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Johnson JK, Lapin B, Green K, Stilphen M. Frequency of physical therapist intervention is associated with mobility status and disposition at hospital discharge for patients With COVID‐19. Phys Ther. 2020;101(1):pzaa181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Kim SY, Kumble S, Patel B, et al. Managing the rehabilitation wave: rehabilitation services for COVID‐19 survivors. Arch Phys Med Rehabil. 2020;101:2243‐2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Le MQ, Rosales R, Shapiro LT, Huang LY. The down side of prone positioning: the case of a Coronavirus 2019 survivor. Am J Phys Med Rehabil. 2020;99(10):870‐872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Lee AJY, Chung CLH, Young BE, et al. Clinical course and physiotherapy intervention in 9 patients with COVID‐19. Physiotherapy. 2020;109:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Levi N, Ganchrow K, Gheva M. Decision‐making: physical therapist intervention for Patients with COVID‐19 in a geriatric setting. Phys Ther. 2020;100(9):1465‐1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Li Z, Zheng C, Duan C, et al. Rehabilitation needs of the first cohort of post‐acute COVID‐19 patients in Hubei, China. Eur J Phys Rehabil Med. 2020;56(3):339‐344. [DOI] [PubMed] [Google Scholar]
- 135. Li J. Rehabilitation management of patients with COVID‐19: lessons learned from the first experience in China. Eur J Phys Rehabil Med. 2020;56(3):335‐338. [DOI] [PubMed] [Google Scholar]
- 136. Sakai T, Hoshino C, Yamaguchi R, Hirao M, Nakahara R, Okawa A. Remote rehabilitation for patients with COVID‐19. J Rehabil Med. 2020;52(9):jrm00095. [DOI] [PubMed] [Google Scholar]
- 137. Saeki T, Ogawa F, Chiba R, et al. Rehabilitation therapy for a COVID‐19 patient who received mechanical ventilation in Japan. Am J Phys Med Rehabil. 2020;99(10):873‐875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Ramalingam MB, Huang Y, Lim PAC. Rehabilitation of post‐ICU patient after severe Covid‐19 pneumonia—A case report. Am J Phys Med Rehabil. 2020;99:1092‐1095. [DOI] [PubMed] [Google Scholar]
- 139. Collaborative, N. P. I. C. R. Responding to COVID‐19 and beyond: A framework for assessing early rehabilitation needs following treatment in intensive care. 2020. Society BSoRMaIC, editor, 36.
- 140. Batty G, Deary I, Luciano M, Altschul D, Kivimäki M, Gale C. Psychosocial factors and hospitalisations for COVID‐19: prospective cohort study based on a community sample. Brain Behav Immun. 2020;89:569‐578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Solli H, Hvalvik S, Bjørk IT, Hellesø R. Characteristics of the relationship that develops from nurse‐caregiver communication during telecare. J Clin Nurs. 2015;24(13–14):1995‐2004. [DOI] [PubMed] [Google Scholar]
- 142. Sarfo FS, Ulasavets U, Opare‐Sem OK, Ovbiagele B. Tele‐rehabilitation after stroke: an updated systematic review of the literature. J Stroke Cerebrovasc Dis. 2018;27(9):2306‐2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Chen J, Jin W, Zhang X‐X, Xu W, Liu X‐N, Ren C‐C. Telerehabilitation approaches for stroke patients: systematic review and meta‐analysis of randomized controlled trials. J Stroke Cerebrovasc Dis. 2015;24(12):2660‐2668. [DOI] [PubMed] [Google Scholar]
- 144. Chaturvedi SK. Covid‐19 related psychiatric disorders and the new psychosocial rehabilitation. J Psychosoc Rehabil Ment Health. 2020; Epub ahead of print:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Mental Health Foundation . Peer Support. Mental Health Foundation. https://www.mentalhealth.org.uk/a-to-z/p/peer-support. Published 2019. Accessed January 8, 2020.
- 146. Ladds E, Rushforth A, Wieringa S, et al. Persistent symptoms after Covid‐19: qualitative study of 114 long Covid patients and draft quality criteria for services. medRxiv. 2020;20(1):1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Medina‐Mirapeix F, Oliveira‐Sousa S, Sobral‐Ferreira M, et al. Continuity of rehabilitation services in post‐acute care from the ambulatory outpatients' perspective: a qualitative study. J Rehabil Med. 2011;43(1):58‐64. [DOI] [PubMed] [Google Scholar]
- 148. Falvey JR, Krafft C, Kornetti D. The essential role of home‐and community‐based physical therapists during the COVID‐19 pandemic. Phys Ther. 2020;100(7):1058‐1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Khera A, Baum SJ, Gluckman TJ, et al. Continuity of care and outpatient management for patients with and at high risk for cardiovascular disease during the COVID‐19 pandemic: a scientific statement from the American Society for Preventive Cardiology. Am J Prev Cardiol. 2020;1:100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Hart JL, Turnbull AE, Oppenheim IM, Courtright KR. Family‐centered care during the COVID‐19 Era. J Pain Symptom Manage. 2020;60(2):e93‐e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Howe EG. How can careproviders most help patients during a disaster? J Clin Ethics. 2011;22(1):3‐16. [PubMed] [Google Scholar]
- 152. Cameron JI, Naglie G, Silver FL, Gignac MA. Stroke family caregivers' support needs change across the care continuum: a qualitative study using the timing it right framework. Disabil Rehabil. 2013;35(4):315‐324. [DOI] [PubMed] [Google Scholar]
- 153. Creasy KR, Lutz BJ, Young ME, Stacciarini JMR. Clinical implications of family‐centered care in stroke rehabilitation. Rehabil Nurs. 2015;40(6):349‐359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Connor J, Madhavan S, Mokashi M, et al. Health risks and outcomes that disproportionately affect women during the Covid‐19 pandemic: A review. Soc Sci Med. 2020;266:113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID‐19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2020;72(4):703–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Burström B, Tao W. Social determinants of health and inequalities in COVID‐19. Eur J Public Health. 2020;30(4):317‐318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Vindrola‐Padros C, Chisnall G, Cooper S, et al. Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID‐19. Qual Health Res. 2020;30(14):2192‐2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information


