Abstract
As the U.S. population ages, communities must adapt to help older adults thrive. Built environment features, like safe sidewalks and crosswalks, provide the foundation for age- and physical activity-friendly communities. Controlled studies are needed to evaluate advocacy training programs that instruct and support seniors to advocate for more walkable neighborhoods. The Senior Change Makers Pilot Study evaluated an advocacy program that taught seniors to evaluate pedestrian environments using the validated MAPS-Mini audit tool, identify barriers, and advocate for improvements. Participants (n = 50) were recruited from four low-income senior housing sites in San Diego, CA, which were randomly assigned to an 8-week advocacy program or physical activity (PA) comparison intervention. Evaluation included surveys, accelerometers to assess PA, and direct observation. Primary outcomes were seniors’ advocacy confidence and skills. Main analyses used repeated measures ANOVAs. Seniors in the advocacy condition (n = 17) increased their advocacy outcome efficacy (p = .03) and knowledge of resources (p = .04) more than seniors in the PA condition (n = 33). Most seniors in the advocacy condition completed a street audit (84%), submitted an advocacy request (79%), or made an advocacy presentation to city staff (58%). Environmental changes included repairs to sidewalks and crosswalks. City staff approved requests for lighting, curb cuts, and crosswalk markings. Seniors’ accelerometer-measured PA did not significantly increase, but self-reported transportation activity increased in the PA condition (p = .04). This study showed the potential of advocacy training to empower seniors to make communities more age- and activity-friendly.
Keywords: Exercise, Built environment, Policy, Older adult, Walkability, Walking, Age-friendly
Engaging older adults as advocates is a promising strategy for making age-friendly community improvements; more research is needed to evaluate and disseminate advocacy training programs
Implications.
Engaging older adults as advocates is a promising strategy for making age-friendly community improvements; more research is needed to evaluate and disseminate advocacy training programs.
INTRODUCTION
Age-friendly communities facilitate healthy aging by promoting and maintaining health across the life course and by helping people with varying physical and mental capacity to continue activities they value [1, 2]. Age-friendly communities provide affordable, accessible housing and transportation, opportunities for social and civic engagement, and built environment features that facilitate physical activity [1].
The health benefits of physical activity for older adults’ health have been well documented [3, 4]. Older adults who meet U.S. Physical Activity Guidelines by engaging in 150 min/week of moderate-intensity aerobic physical activity have 28% lower mortality compared to their less active counterparts [4, 5]. Yet older adults remain the least active age demographic [6]. Older adults are more physically active in safe, walkable, and aesthetically appealing neighborhoods [7, 8]. This higher activity level has been found across physical activity domains, including active travel [9, 10] and leisure time activity [11].
Engaging residents as advocates is a promising strategy for making age-friendly community improvements [2, 12]. The Surgeon General’s Call to Action to Promote Walking and Walkable Communities endorsed community member advocacy as an evidence-based strategy for making communities more activity-friendly [13]. Enacting changes to improve the physical activity environment requires relevant, local data [14]. However, local governments often lack funding to conduct audits (e.g., structured inventories of physical activity features of an environment) needed to identify and prioritize pedestrian barriers in every neighborhood. Community members, who stand to be the most impacted by built environment changes, can provide a valuable service by collecting data and informing local public works projects and policy decisions [12, 14].
The Our Voice Initiative [12], a series of participatory research projects conducted across the globe, included at least 14 programs empowering older adults to create positive change in their local environments. Participants in the Our Voice studies used the Discovery Tool mobile application to photograph features of their communities that might impact health, record audio or text narratives, discuss these qualitative data, and advocate for change [12]. Outcomes included creating a senior-friendly walking map, repairing sidewalks and crosswalks, and installing benches and wayfinding signage [12]. Our Voice focused on environmental outcomes, but increases in participants’ community engagement, empowerment, and neighborhood cohesion were also documented [12]. Despite potential benefits to the individual and community, older adults are rarely engaged as equitable partners or agents for change [15]. This is germane in underserved communities, where residents suffer higher rates of disability and chronic disease but are traditionally excluded from civic engagement and public discourse [12, 16].
Building on the Our Voice Initiative, The Senior Change Makers Pilot Study evaluated an advocacy training program conducted in low-income senior housing communities. Whereas most advocacy programs have used audit tools that collected qualitative data, the present study used the Microscale Audit of Pedestrian Streetscapes-Mini (MAPS-Mini) audit tool, which provides quantitative assessment of pedestrian environments [17]. Research has successfully used MAPS-Mini for advocacy work with youth [18], and the current study tested the tool’s usability with older adults. The primary aim of the present study was to assess the efficacy and feasibility of an 8-week advocacy program in comparison to a physical activity control intervention to increase seniors’ advocacy skills and confidence. We hypothesized the advocacy program would produce greater improvements in seniors’ advocacy skills and confidence at 8 weeks as compared to the physical activity program. The present study fills a gap in advocacy research by reporting a cluster-randomized controlled trial of an advocacy training program.
METHODS
The Senior Change Makers Pilot Study applied a multi-level approach with intervention components and measures at the individual, social, and environmental levels [19]. The study was informed by Social Cognitive Theory, providing training to develop advocacy skills and self-efficacy [20], and Empowerment Theory, providing opportunities to influence the environment through advocacy [21].
Study sites
Recruitment of low-income senior housing sites started in summer 2016 and was completed in 6 weeks. The researchers sought sites that met the following criteria: 150 or more low-income units to ensure a sufficient recruitment pool; units offered at reduced rent through government or other financial assistance programs; residents with diverse racial-ethnic backgrounds; majority of English-speaking residents; facilities available for onsite meetings; safe surroundings for outdoor walks; and site administrative approval. Using a directory of affordable housing, the researchers identified 13 low-income senior housing complexes with 150 or more units in the City of San Diego. The research team met with managers or activity coordinators at the 10 sites with the most housing units to maximize the recruitment pool. Six of the 10 sites were eliminated due to ongoing construction, lack of site administrative approval, majority of residents did not speak English, concerns regarding unsafe surroundings, another research study already in progress, and not enough residents to meet recruitment goals. The remaining four sites met study criteria and agreed to participate in either study condition. The four senior housing sites were randomly assigned using an online randomizing tool to either the physical activity or advocacy condition, such that two sites were in each condition. Randomization at the site-level was necessary to avoid cross-contamination of intervention activities within sites. Randomization occurred prior to recruitment.
Study population
Participants were recruited in fall 2016. Recruitment involved a collaboration with site managers and used word of mouth, flyers, and short presentations at pre-scheduled events like monthly resident birthday parties. Recruitment goals for the pilot study were limited by study funds but aimed for a sufficient sample to test program feasibility and identify statistical trends for primary outcomes. Eligibility criteria included being 50 years of age or older, having no falls that resulted in hospitalization in the past year and no non-exercise related chest pain in the past month, ability to walk without human assistance (cane or walker okay), fluency in English, and ability to provide informed consent. The University Institutional Review Board approved the study, and all participants gave written informed consent.
Intervention and control conditions
Both conditions involved weekly, 1-hr group meetings for 8 weeks. Weekly topics are listed in Table 1 and program materials, including leader guides and participant handouts, are available online at www.drjimsallis.org. To ensure consistency across the two advocacy sites and two physical activity sites, the researchers prepared detailed agendas and held weekly meetings to review the curriculum. The primary investigator co-led all study meetings to reinforce consistent practices across groups. Participants in the advocacy program identified potential advocacy projects using the MAPS-Mini [17]. MAPS-Mini is a 15-item audit used to score neighborhood features that relate to physical activity, such as the presence of sidewalks, benches, parks, graffiti, and trip hazards [17]. When conducting the audit, participants tested both a paper and electronic (mobile application) version of MAPS-Mini. Participants used the audit data to create a list of potential advocacy projects, which they prioritized based on importance and feasibility [14]. Participants presented selected projects to transportation engineers, submitted online requests through a municipal website, and/or called elected officials. The curriculum for the physical activity condition used an adapted evidence-based program for older adults [22] and included group exercise plus behavior change strategies, such as goal setting, social support, and positive thinking for increasing physical activity. The 8-week intervention concluded in November 2016. A 4-month follow-up was conducted in March 2017. All participants received a $20 gift card for completing post-test measures.
Table 1.
Weekly program topics by study condition
| Week | Advocacy condition | Physical activity condition |
|---|---|---|
| 0 | Introductory meeting Eligibility screening; informed consent Distribute baseline surveys and accelerometers |
Introductory meeting Eligibility screening; informed consent Distribute baseline surveys and accelerometers |
| 1 | Kick off Welcome and group guidelines Benefits of physical activity and current guidelines Environment and physical activity |
Kick off Welcome and group guidelines Walking safety; fall prevention Group walk |
| 2 | Introduction to advocacy and MAPS-Mini Advocacy 101 handout Introduction to MAPS-Mini tool for pedestrian audits |
Walking benefits and self-monitoring Posture and hip hinge Physical activity guidelines for seniors Benefits of physical activity Self-monitoring worksheet |
| 3 | MAPS-Mini in the field Group MAPS-Mini audit outdoors Homework: conduct MAPS-Mini audit around your home |
Benefits, barriers, and goal setting Benefits and barriers to physical activity SMART goals Group walk |
| 4 | Selecting an Advocacy Project Report back on your audit findings Evaluate projects’ importance and feasibility; select projects Prepare for meeting with traffic engineer Homework: presentations for traffic engineer |
Beyond walking (strength, flexibility, balance) Benefits of different modes of exercise Incorporating exercise into daily life Stations with different types of exercise Review guidelines and goals |
| 5 | Meeting with a Traffic Engineer Introduction to local transportation department, request process, and “Get it Done” website Present issues to traffic engineer |
Social support and positive thinking Identifying a support system Positive thinking in everyday life Group walk |
| 6 | Submitting online requests Creating a fact sheet Submit online request to city Homework: call your representative |
Sedentary behavior and health Identify adverse conditions associated with sedentary behavior Decreasing sedentary behavior Group walk |
| 7 | Advocacy work continued Example advocacy projects by older adults Calling your representative—report back Creating action plans and anticipating challenges Advocacy skills: communicating with your representative, identifying partners Distribute post-intervention surveys and accelerometers |
Keeping up the habit Barriers to walking Setbacks and relapse Group walk Distribute post-intervention surveys and accelerometers |
| 8 | Celebration/graduation Report on advocacy accomplishments Certificates of completion Collect post-intervention surveys and accelerometers |
Celebration/graduation Active games; review of key concepts Certificates of completion Collect post-intervention surveys and accelerometers |
Outcome measures
Outcome measures included pre-post surveys and pre–post accelerometer data. Details of instruments are provided in Table 2.
Table 2.
Measures for primary outcomes, secondary outcomes, and process evaluation
| Construct | Measure and timing | Scales or item | Psychometrics and source |
|---|---|---|---|
| Primary outcome | |||
| Advocacy confidence and skills |
Survey: baseline, 8 weeks |
• Self-efficacy for advocacy (mean of 2) • Perceived sociopolitical control: active participation (mean of 2) • Perceived sociopolitical control: optimism for change (mean of 2) • Advocacy outcome efficacy (1 item) • Assertiveness (mean of 3) • Participatory competence (mean of 2) • Knowledge of resources (1 item) • Group resiliency (1 item) |
Inter-item correlations ranged from .268 to .818 [23] |
| Secondary outcomes | |||
| Advocacy actions and outcomes | Tracking list; follow-up interviews |
Researchers tracked advocacy actions taken by advocacy group members during the 8-week program. Four months post-intervention, researchers called advocacy group members for updates. | [24] |
| Physical activity | Survey and accelerometer: baseline, 8 weeks |
• Accelerometer: mean min. MVPA/valid day • IPAQ Transportation PA: mean min/week • IPAQ Leisure PA: mean min/week • BRFSS strength: mean min/week • BRFSS flexibility: mean min/week |
IPAQ: Intraclass correlation coefficient 0.50 to 0.65 [25] |
| Process evaluation | |||
| Intervention adherence | Attendance sheet | Rate of participant attendance at group meetings. | [26] |
| Fidelity | Direct observation | Percentage of key curriculum points covered by site. | [27] |
| Perception of experience | Survey: 8 weeks |
• Roles and participation: Likert (mean of 2) • Opportunities for control in group (mean of 2) • Group cohesion (mean of 2) • Coordinator/leader characteristics (mean of 3) • Collective efficacy toward group goals (one item) • Pride in group work (mean of 2) • Follow up group resiliency (mean of 2) |
Inter-item correlations ranged from .202 to .481 [23] |
| MAPS-Mini evaluation | Focus group: week 3 |
Seniors provided feedback on MAPS-Mini usability, satisfaction, electronic versus paper, and provided recommendations for improvement. | [17, 28] |
Note. MVPA = moderate-to-vigorous physical activity; IPAQ = International Physical Activity Questionnaire; PA = physical activity; BRFSS = Behavioral Risk Factor Surveillance System.
Advocacy confidence and skills
Eight validated advocacy measures developed for the Youth Engagement and Action for Health (YEAH!) program [18, 23] were adapted and used to measure primary outcomes of advocacy confidence and skills in both conditions at baseline and 8 weeks. Content validity of the original advocacy measures was strengthened by use of Empowerment and Social Cognitive Theories and adaptation of items from the tobacco control literature [23]. Results of confirmatory factor analysis and inter-item correlations for subscales are reported in full elsewhere [23]. Scores for the eight advocacy measures were also averaged to create a cumulative advocacy index. Some items were revised from the original items [23] to apply to senior respondents and physical activity. For example, the item: “I am confident that I can work to make my school or community a better place for being physically active and eating healthy” was revised to read: “I am confident that I can work to make my community a better place for being physically active.”
Advocacy actions and outcomes
Researchers tracked the advocacy group members’ completion of advocacy actions (e.g., presentations to city staff) and resulting environmental changes (e.g., repaired sidewalks) throughout the 8-week intervention. Four months after the intervention ended, the research team followed up with the advocacy group participants for a brief interview to determine if any actions were taken, or results achieved, since the program ended. Researchers were guided by a list of advocacy actions and outcomes, including interim outcomes that often precede policy or environmental changes [24].
Physical activity
Seniors’ physical activity was measured at baseline and 8 weeks via accelerometer and survey. Participants wore Actigraph accelerometers (model GT3X, Pensacola, FL) on the dominant side of their waist for 7 days (with a minimum of five valid days) during waking hours except when bathing or swimming. A valid day was defined as 10 valid hours of wearing, and a valid hour had no more than 30 consecutive minutes of zero-intensity counts, an indication the meter was not being worn [29]. Accelerometers were set to collect data in 60-s epochs. MeterPlus version 4.0 was used to score and clean accelerometer data. Moderate-to-vigorous physical activity (MVPA) was scored using validated algorithms and cut points (≥1952 counts/min) [30] and calculated as average minutes of MVPA per valid wearing day [29].
Items from the International Physical Activity Questionnaire (IPAQ) Long version were used to assess self-reported walking for transportation and walking for leisure [25]. The IPAQ has been shown to be reliable and valid with older adults [25]. Two items were adapted from the Behavioral Risk Factor Surveillance System to assess frequency and duration of strength and flexibility training [31].
Process evaluation
Process evaluation measures included direct observation of group sessions, post-test survey items, and focus groups on MAPS-Mini (Table 2). Post-intervention focus groups were held to assess study feasibility; see the Supplemental Report for methods and results.
Intervention adherence and fidelity
Researchers took attendance at all group meetings in both conditions to evaluate intervention exposure [26]. To measure fidelity to intervention, direct observation was conducted in 34% (11/32) of group meetings across conditions by two researchers trained in direct observation. Researchers assessed coverage of predetermined key curriculum points for the physical activity and advocacy programs; scores for the two observers were averaged [27].
Perception of experience
In both conditions, post-test survey items [23] assessed participants’ perceptions of their roles and participation, opportunities for control in group work, group cohesion, leader characteristics, collective efficacy, pride in group work, and group resiliency.
MAPS-Mini focus group
After participants in the advocacy condition completed their pedestrian audit, researchers trained in qualitative methods held a focus group at each advocacy site to obtain feedback on the MAPS-Mini tool and evaluate feasibility for use among older adults. The moderator guide addressed likes/dislikes, clarity of items assessing neighborhood features, use of the mobile application, and feedback on pre-audit training [28]. Feasibility was considered “achieved” if >51% of focus group participants stated they could easily understand and use the MAPS-Mini tool, and the tool aided their advocacy process. Participants received a reusable shopping bag incentive for participation.
Statistical Analyses
Statistical analyses were performed using SPSS, version 24 (SPSS Inc., Chicago, IL). Significance was tested at alpha = .05.
Preliminary analyses
Descriptive statistics were used to report participant demographics. Baseline characteristics of participants were compared between study conditions using univariate ANOVAs for continuous variables and chi-square tests for dichotomous variables. To determine whether it was appropriate to aggregate participants across sites within the same condition (advocacy vs. physical activity) for analyses, SPSS General Linear Model univariate ANOVAs (for continuous variables) and chi-square tests (for dichotomous variables) were conducted to identify baseline differences among the four sites. Analyses showed no baseline differences across sites, supporting use of the intervention condition (advocacy vs. physical activity) rather than separate sites as the key independent variable per the a priori study design.
Primary outcomes
Main analyses testing intervention effects on advocacy confidence and skills were conducted using 2 (condition) × 2 (time) repeated measures ANOVAs. Condition by time interactions were examined to assess differential efficacy of the two programs to increase advocacy confidence and skills, with the hypothesis that primary advocacy-related outcomes would increase more over time for participants in the advocacy condition than those in the physical activity condition. Partial eta squared (η p2) was reported as a measure of effect size for the interaction term. The partial eta squared statistic can be interpreted as the percentage of unexplained variation in the outcome that can be uniquely explained by the time by condition interaction.
Secondary outcomes
Advocacy actions and outcomes were reported with a narrative summary of advocacy actions taken and outcomes achieved. Physical activity outcomes included both objective accelerometer measures of physical activity minutes and self-reported survey measures. To assess the differential efficacy of the two programs to increase physical activity, we used ANOVAs for repeated measures and examined the condition by time interactions.
Process evaluation
To report on measures of intervention adherence and fidelity, we used descriptive statistics. To compare advocacy versus physical activity condition participants’ perceptions of their experiences, we used the univariate ANOVA main effect for intervention condition to evaluate differences in the post-test scale means for each group. Data from the focus groups assessing feasibility for use of MAPS-Mini among older adults were analyzed separately by two researchers using content analysis to identify themes. Results were discussed and summarized in narrative form.
RESULTS
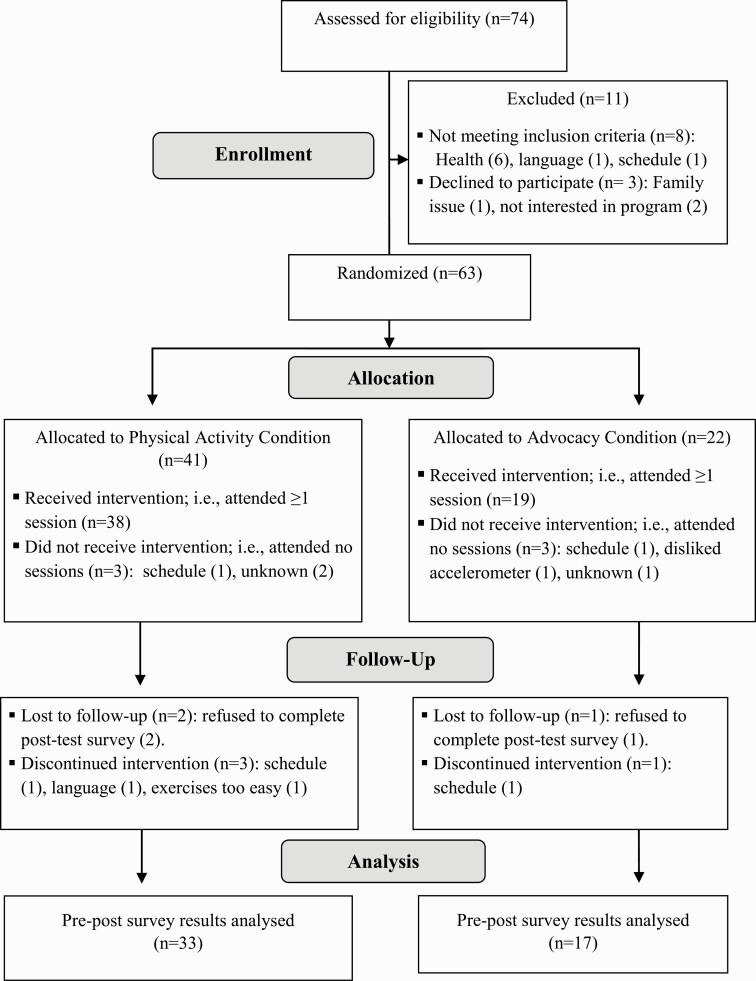
Of the 63 participants randomized by housing site (41 physical activity, 22 advocacy), 50 completed baseline and post-intervention data and were analyzed for the primary advocacy outcomes (33 physical activity, 17 advocacy). See Figure 1 for a participant flow diagram. Sample demographics and key baseline characteristics are presented in Table 3. At baseline, participants averaged 13 min of MVPA per day (SD = 18). Seniors in the physical activity condition accrued more daily MVPA (16.8 min/day, SD=19.6) than those in the advocacy condition (5.6 min/day, SD=8.7) at baseline, F(1, 51) = 4.99, p = .030. A higher percentage of those in the advocacy condition (52%) compared to the physical activity condition (18%) reported they had previously contacted a government official (p = .005). There were no other significant baseline differences between participants in the two conditions.
Fig 1.
CONSORT flow diagram of participants.
Table 3.
Sample demographics and baseline characteristics by study condition
| Physical activity | Advocacy | Total | p | |
|---|---|---|---|---|
| Number of participants | n = 39 | n = 21 | n = 60 | |
| Age, mean (SD) | 76 (9.65) |
74 (9.18) |
75 (9.45) |
.490 |
| Gender, % female | 83 | 86 | 84 | .747 |
| White, non-Hispanic, % | 65 | 81 | 70 | .194 |
| Annual household income, % | .141 | |||
| <$20,000 | 67 | 81 | 72 | |
| $20,000–$39,999 | 24 | 19 | 22 | |
| ≥ $40,000 | 9 | 0 | 6 | |
| Highest education completed, % | .209 | |||
| Junior high or less | 8 | 0 | 5 | |
| Some high school | 18 | 14 | 17 | |
| Some college or vocational | 46 | 57 | 50 | |
| Completed college | 21 | 10 | 17 | |
| Completed graduate degree | 8 | 19 | 12 | |
| BMI, mean (SD) | 27 (6) | 30 (8) | 28 (7) | .226 |
| Obese, % | 25 | 43 | 32 | .162 |
| MVPA, accelerometer, mean min/day (SD) | 16.8 (19.6) | 5.6 (8.7) | 13.1 (17.5) | .030 |
| Transport PA, mean min/week (SD) | 225 (239) | 251 (269) | 234 (248) | .702 |
| Leisure PA, mean min/week (SD) | 226 (219) | 127 (215) | 190 (221) | .101 |
| Strength PA, mean min/week (SD) | 83 (110) | 56 (85) | 74 (102) | .336 |
| Flexibility PA, mean min/week (SD) | 89 (92) | 54 (53) | 77 (81) | .115 |
| Self-efficacy for exercise, mean, range 1–10 (SD) | 6.1 (2.4) | 5.6 (2.6) | 5.4 (2.5) | .486 |
| Self-efficacy for advocacy, mean range 1–5(SD) | 4.0 (1.0) | 3.8 (.9) | 4.0 (.9) | .321 |
| Prior advocacy, range 0–6 (SD) | 1.7 (1.6) | 2.4 (1.7) | 2.0 (1.6) | .134 |
| Signed a petition, % yes | 59 | 71 | 63 | .348 |
| Contacted government official, % yes | 18 | 52 | 30 | .005 |
| Contacted news media, % yes | 28 | 38 | 32 | .441 |
| Letter to editor, % yes | 15 | 19 | 17 | .722 |
| Community assessment, % yes | 15 | 14 | 15 | .911 |
| Met school/government. official, % yes | 36 | 43 | 38 | .604 |
| Nothing prior to study, % yes | 23 | 19 | 22 | .723 |
Note. SD = standard deviation; BMI = body mass index (weight in kg/height in m2); MVPA = moderate to vigorous physical activity; PA = physical activity; obese = BMI > 30; p-values are for ANOVA F’s for between-groups effects when measures are continuous or ordinal and for chi-square tests when measures are dichotomous variables (gender, %White, and % obese). Boldface signifies alpha greater than or equal to .05.
Advocacy confidence and skills
Average changes in participants’ advocacy beliefs and skills from baseline to post-intervention 8 weeks later are shown for each measure in Table 4. Two of eight advocacy measures produced significant condition by time interactions with the advocacy group showing increases over time and the physical activity group showing minimal change: advocacy outcome efficacy, F(1, 47) = 4.75, p = .034, η p2 = .092, and knowledge of resources, F(1, 47) = 4.52, p = .039, η p2 = .088. The cumulative advocacy index showed a trend for the advocacy group to increase overall scores over time and the physical activity group to show minimal change, F(1, 47) = 3.81, p = .057, η p2 = .075.
Table 4.
Seniors’ advocacy skills and confidence: constructs, item language, and changes by study condition from baseline to 8 weeks
| Construct | Items (range 1–5)* | Physical actvity Mean (SD) n = 32 |
Advocacy Mean (SD) n = 17 |
F(1, 47) | p | η p2 | ||
|---|---|---|---|---|---|---|---|---|
| Baseline | 8 wks | Baseline | 8 wks | |||||
| Self-efficacy for advocacy | (1) I am sure that I can tell my friends to be physically active. (2) I am confident that I can work to make my community a better place for being physically active. |
4.05 (1.01) | 3.91 (.87) | 3.65 (.86) | 4.03 (1.10) | 2.36 | .131 | .048 |
| Perceived sociopolitical control: active participation | (1) I like to wait and see if someone else is going to solve a problem (reverse coded). (2) I find it very hard to talk in front of a group (reverse coded). |
3.36 (1.19) | 3.24 (1.00) | 3.59 (.92) | 3.59 (.81) | .183 | .671 | .004 |
| Perceived sociopolitical control: optimism for change | (1) If I tell someone “in charge,” like a leader, about my opinions, they will listen to me. (2) I enjoy participation in community groups because I want to have as much say as possible in my community. |
3.56 (.86) | 3.77 (.71) | 3.62 (.99) | 4.12 (.65) | 1.20 | .280 | .025 |
| Advocacy outcome efficacy | (1) Community groups can advocate for changes to make communities better places for physical activity. | 4.28 (.73) | 4.31 (.74) | 4.18 (.81) | 4.65 (.70) | 4.75 | .034 | .092 |
| Assertiveness | (1) I can talk with others about issues I believe in. (2) I can ask others to help work on making our community healthier. (3) I can start discussions with others about how to change our community to make it healthier. |
3.84 (.71) | 3.82 (4.16) | 4.18 (.67) | 4.16 (.60) | .000 | .997 | .000 |
| Participatory competence and decision-making | (1) If I have a problem when working towards a goal, I usually do not give up. (2) I can influence the decisions my group makes. |
3.92 (.98) | 4.06 (.78) | 3.74 (1.00) | 3.88 (.99) | .001 | .980 | .000 |
| Knowledge of resources | (1) I know how to get information about ways to make my community a better place for being physically active. | 3.72 (.99) | 3.66 (1.81) | 3.24 (1.25) | 4.00 (.79) | 4.52 | .039 | .088 |
| Group resiliency | (1) I am confident that our Senior Change Makers group can work through problems if they arise. | 4.00 (.88) | 4.16 (.81) | 3.94 (.97) | 4.41 (1.00) | 1.41 | .240 | .029 |
| Cumulative Advocacy Index | Mean of scores from 8 advocacy measures listed above (α = .791) | 3.84 (.56) | 3.86 (.52) | 3.76 (.72) | 4.10 (.64) | 3.81 | .057 | .075 |
Note: Items adapted from Millstein et al. [23]. Range 1–5: 1 = disagree strongly, 2 = disagree somewhat, 3 = neutral, 4 = somewhat agree, 5 = strongly agree; F’s and associated statistics are for the condition-by-time interaction term from repeated measures ANOVAs; η p2 = partial eta squared. Boldface signifies alpha greater than or equal to .05.
Advocacy actions and outcomes
Of the seniors in the advocacy groups, most completed an audit of nearby streets (84%), submitted an online advocacy request to the local transportation department (79%), and made an advocacy presentation (58%). These activities were completed during program sessions over the course of 8 weeks. Fewer seniors performed advocacy “homework” outside of sessions, such as making follow up telephone calls (42%) and emails (11%). In response to participant advocacy, within 1 month city staff patched broken asphalt in three crosswalks, fixed cracks in two sidewalks, approved two new streetlights, approved new curb cuts for two intersections, lengthened pedestrian signals, and fixed a broken water meter box in a sidewalk. At the 4-month follow up, one advocacy group had created their own “Senior Change Makers” group that met monthly to continue advocacy efforts.
Physical activity
Accelerometer protocols were completed by 56 participants at baseline and 50 participants at 8 weeks. Re-wears were requested in 16 cases to obtain complete data. Five participants were excluded from analyses because they did not accrue five valid wear days at both time points. No significant time by condition interactions were found for any accelerometer-measured outcome (Table 5). One of four self-reported physical activity measures produced a significant time by condition interaction. Participants in the physical activity condition reported increases over time in their “walking for transportation” to get from place to place, whereas participants in the advocacy condition showed a small decline, F(1, 47) = 4.35, p = .042, η p2 = .085.
Table 5.
Seniors’ physical activity: changes by study condition from baseline to 8 weeks
| Measure | Items | Physical activity n = 32 |
Advocacy n = 17 |
F(1, 47) | p | η p2 | ||
|---|---|---|---|---|---|---|---|---|
| Baseline | 8 wks | Baseline | 8 wks | |||||
| Accelerometer physical activity; mean min/valid wear day (SD); n = 44 (29 physical activity, 15 advocacy) |
Moderate and vigorous physical activity (MVPA) | 17.4 (19.2) | 17.6 (22.4) | 5.2 (9.0) | 3.6 (6.5) | .506 | .481 | .012 |
| Vigorous physical activity | .04 (.18) | .11 (.29) | .00 (.00) | .00 (.00) | .892 | .350 | .021 | |
| Moderate physical activity | 17.3 (19.2) | 17.5 (22.2) | 5.2 (9.0) | 3.6 (6.5) | .462 | .501 | .011 | |
| Light physical activity | 255.9 (92.4) | 269.0 (97.4) | 201.4 (57.0) | 194.4 (53.5) | 2.24 | .142 | .051 | |
| Sedentary | 551.8 (120.0) | 574.6 (160.6) | 602.7 (87.4) | 593.2 (98.3) | .867 | .357 | .020 | |
| Nonwear | 615.0 (66.5) | 578.9 (131.0) | 630.7 (71.2) | 648.7 (90.7) | 2.66 | .110 | .060 | |
| Transportation physical activity: adapted from IPAQ; mean min/week (SD) |
(1) During the last 7 days, on how many days did you walk for at least 10 minutes at a time to go from place to place? (2) How much time did you usually spend on ONE of those days walking from place to place? | 234.5 (252.6) | 377.5 (317.6) | 214.1 (252.2) | 164.4 (207.8) | 4.35 | .042 | .085 |
| Leisure physical activity: adapted from IPAQ; mean min/week (SD) |
(1) Not counting any walking for transportation you already mentioned above, during the last 7 days, on how many days did you walk for at least 10 minutes at a time in your leisure time? (2) How much time did you usually spend on ONE of those days walking in your leisure time? | 214.9 (205.6) | 252.5 (283.2) | 116.5 (220.5) | 79.1 (89.6) | 1.07 | .306 | .022 |
| Strength training: adapted from BRFSS; mean min/week (SD) |
(1) During the last 7 days, on how many days did you do activities designed to increase muscular strength or tone, such as lifting weights, pull-ups, push-ups, or sit ups? (2) How much time did you usually spend on ONE of those days doing activities designed to increase strength? | 93.9 (116.2) | 108.9 (111.0) | 52.0 (86.3) | 75.9 (130.6) | .078 | .781 | .002 |
| Flexibility training: adapted from BRFSS; mean min/week (SD) |
(1) During the last 7 days, on how many days did you do any activities designed to increase flexibility, such as stretching or yoga? (2) How much time did you usually spend on ONE of those days doing activities designed to increase flexibility? | 95.9 (93.2) | 138.3 (134.4) | 47.1 (53.6) | 92.6 (140.3) | .007 | .936 | .000 |
Note. F’s and associated statistics are for the condition-by-time interaction term from repeated measures ANOVAs. η p2 = partial eta squared; IPAQ = International Physical Activity Questionnaire; BRFSS = Behavioral Risk Factor Surveillance System. Boldface signifies alpha greater than or equal to .05.
Process evaluation
Seniors’ attendance rates in both groups remained steady over the course of the 8-week programs, ranging from 81% (week 6) to 93% (week 7). Coverage of key curriculum points, a measure of intervention fidelity, was similar in both groups, with a range of 80–100%.
Perception of experience
Seniors in the advocacy condition reported significantly higher levels of group participation, F(1, 47) = 5.04, p = .029, η p2 = .095, and reported more opportunities for control in group work, F(1, 47) = 8.48, p = .005, η p2 = .150, than seniors in the physical activity condition. Participants of both study conditions gave similar ratings for group cohesion, leader characteristics, collective efficacy toward group goals, pride in group work, and follow-up group resiliency.
MAPS-Mini focus group
Focus group participants from both advocacy groups (n = 14) concurred the MAPS-Mini tool was easy to use and understand. The tool helped them learn about features that impacted walking and drew attention to pedestrian barriers they might not have otherwise noticed. For example, several participants never noticed sidewalk buffers before but recognized they felt safer when there was a barrier, like a planter, separating them from traffic. Several participants reported that completing the audit with participants with different impairments (e.g., vision, balance, and use of assistive devices) provided a broader perspective for understanding potential barriers. Most participants preferred the paper version of the tool over the electronic version because of the tablet’s weight, glare, and challenges using the touch screen. Several participants reported balance challenges carrying their personal items, and/or assistive devices while walking and completing the audit tool. They appreciated having research assistants help carry items, take photographs, and fill out the audit tool.
Discussion
The Senior Change Makers Pilot Study showed the potential for an 8-week advocacy program to increase older adults’ advocacy skills and beliefs and result in real community improvements. The advocacy group participants worked with the City of San Diego’s Transportation Department to fix trip hazards on multiple crosswalks and sidewalks and repair a broken crosswalk signal. The City approved requests for additional street lighting, curb cuts, and crosswalk striping. Compared to participants in the physical activity comparison condition, seniors in the advocacy condition improved on two of eight advocacy measures: advocacy outcome efficacy and knowledge of resources. The cumulative advocacy index showed a trend for the advocacy group to increase scores more than the physical activity group over time. Findings of increased advocacy confidence and skills concur with previous uncontrolled advocacy studies [18, 32].
The advocacy curriculum sought to foster self-efficacy for advocacy by teaching skills and providing opportunities to advocate. The item testing advocacy outcome efficacy asked participants whether they believed “community groups can advocate for changes to make communities better places for physical activity.” Advocacy participants saw results within one month of their advocacy efforts. Seeing results, even a temporary or small fix, may be important for developing advocacy efficacy, which could be expected to facilitate further advocacy actions. To increase knowledge of resources, advocacy program participants received a tailored resource list featuring information germane to their communities and advocacy topics. Participants used the resource list, which included contact information for the Department of Transportation, the Mayor’s office, and other local representatives, to advocate for community change.
Small effect sizes for advocacy outcome efficacy and knowledge of resources might be explained by high baseline scores on the 5-point scale and having only one item per construct. Nonsignificant findings on six advocacy measures may be explained by the small sample size, high baseline scores (e.g., assertiveness and group resiliency), and unexpected increases in the physical activity groups’ scores, suggesting that advocacy and physical activity programs—or any group program that promotes socialization and attention—may confer some common psychosocial benefits. Survey items measuring advocacy outcomes were based on a validated tool used in youth advocacy [23], but some items were modified for use with older adults, and these adapted items lack psychometric analysis.
The MAPS-Mini audit tool proved feasible for use with older adult participants, with minimal training. MAPS-Mini was developed and evaluated using physical activity data from participants of all ages [17], and the present study was the first to evaluate its application in an advocacy training program. The criteria for determining feasibility were whether the tool was easy to use and aided the advocacy process. Focus group participants reported the tool was usable, though they preferred the paper version to the digital version on a tablet. The tool aided the advocacy process by providing a checklist of potential issues, teaching key terminology, and recording data to inform advocacy projects. Having group members with different impairments (vision, mobility, balance, etc.) and assistive devices conduct observations together made participants aware of built environment barriers they may not have experienced personally. One participant noted she was able to walk around holes in the crosswalk, but her friends with wheelchairs and walkers could not avoid the hazards. This experience points to greater empathy and compassion for others with disabilities, which may help reduce feelings of loneliness and improve well-being among seniors [33]. Older adults may be disproportionately affected by certain pedestrian barriers [16], and systematic observations that inform advocacy actions can help raise awareness and address needs.
Physical activity did not increase in the advocacy group. This was not surprising given the advocacy intervention did not directly target physical activity behavior change. The physical activity group increased self-reported walking for transportation activity, but the accelerometer-measured outcomes did not show significant condition by time interactions. The lack of change in seniors’ MVPA may be explained by the physical activity group’s relatively high baseline MVPA (17 min/day). In comparison, an observational study that used the same accelerometer cut points found community dwelling older adults accrued only 7 min/day of MVPA [29]. The physical activity group’s higher baseline MVPA might be explained by the resident population at the physical activity sites being more active by chance, or participants increasing their activity after study screening [34] or during baseline assessment due to measurement reactivity [35]. Future intervention studies might explore various accelerometer cut points to determine which may be more sensitive to change. For example, using the Freedson et al., younger-adult moderate intensity cut points [30], as was done in the study of older adults by King et al. [29], or high-light intensity cut points, as suggested by Buman et al. [36].
The Senior Change Makers Pilot Study adds to the rigor of the advocacy literature by using a cluster-randomized controlled study design, engaging seniors living in low-income housing, evaluating individual psychosocial factors, employing mixed methods evaluation, and using a quantitative audit tool. Study methods proved feasible with respect to recruitment, retention, intervention fidelity, and use of MAPS-Mini.
Study results showed some significant intervention effects, but the small sample size for sites and participants was an important limitation in this study. Larger samples sizes are needed to perform mediation analysis and explore pathways from the advocacy intervention to psychosocial factors and advocacy outcomes. Sample bias may have occurred due to use of a non-probability sampling method and randomization of sites prior to participant recruitment, which meant that the intervention description differed across conditions and could have appealed to different subsets of residents. Another source of bias could be imbalances in site characteristics at baseline. Future studies might consider matching sites according to baseline characteristics, such as those related to resident engagement, prior to randomization. In this study, differences in recruitment across sites may be attributable to variations across sites in study promotion by site staff, level of pre-existing programs and activities for residents, access to common spaces for events and activities, and level of resident engagement in site-sponsored activities. Risk of imbalance at baseline is greater in cluster-randomized trials compared to trials randomizing individuals because of challenges recruiting clusters with equal number of participants and the correlated nature of nested data [37]. Future and larger studies can correct for this limitation.
Findings support the need to continue conducting, evaluating, and disseminating advocacy programs that promote age-and activity-friendly communities. Future research might test strategies to recruit and engage isolated seniors and those who do not speak English as a first language. Future research might also assess psychometric properties of the revised survey items, and whether specific advocacy constructs are more important to successful advocacy outcomes. Longer-term studies are needed to address complex advocacy projects that require coalition building, fundraising, or political engagement, and to evaluate distal advocacy and health outcomes. Reporting health benefits associated with environmental changes, especially when translated into health care cost savings, can help persuade decision makers and build the case for activity-friendly community improvements.
Supplementary Material
Acknowledgments
We would like to acknowledge Sandra Winter, Katherine Briggs, and Abby Lawrence-Jacobson for their guidance on advocacy program materials and processes, Circulate San Diego for advocacy worksheets, and Khalisa Bowling and Katie Crist for guidance on the physical activity program. Final advocacy program materials are available for public review and use at www.drjimsallis.org.
Funding
This study was funded by a grant from the San Diego Foundation. The primary author was the recipient of the Allen and Pearl Reiter Scholarship for Research on Healthy Aging. Accelerometers were donated by Active Living Research.
Compliance with Ethical Standards
Conflict of Interest: All authors declare that they have no conflicts of interest.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
Study Registration: The study was pre-registered at http://clinicaltrials.gov. Link to study record: https://clinicaltrials.gov/ct2/show/NCT02944838.
Analytic Plan Pre-registration: The analysis plan was not formally pre-registered.
Data Availability: De-identified data from this study are not available in a public archive. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author.
Analytic Code Availability: Analytic code used to conduct the analyses presented in this study are not available in a public archive. They may be available by emailing the corresponding author.
Materials Availability: Some of the materials used to conduct the study are presented in a public archive: www.drjimsallis.org
References
- 1. World Health Organization. Global strategy and actionplan on ageing and health.2017. Retrieved November 18, 2020, from https://apps.who.int/iris/bitstream/handle/10665/329960/9789241513500-eng.pdf
- 2. Jeste DV, Blazer DG 2nd, Buckwalter KC, et al. . Age-friendly communities initiative: public health approach to promoting successful aging. Am J Geriatr Psychiatry. 2016;24(12):1158–1170. [DOI] [PubMed] [Google Scholar]
- 3. Chou CH, Hwang CL, Wu YT. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil. 2012;93(2):237–244. [DOI] [PubMed] [Google Scholar]
- 4. U.S. Department of Health and Human Services. Physical activity guidelines for Americans, 2nd ed. 2018. Retrieved November 18, 2020, from https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf [Google Scholar]
- 5. Hupin D, Roche F, Gremeaux V, et al. . Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged ≥60 years: a systematic review and meta-analysis. Br J Sports Med. 2015;49(19):1262–1267. [DOI] [PubMed] [Google Scholar]
- 6. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. [DOI] [PubMed] [Google Scholar]
- 7. Barnett DW, Barnett A, Nathan A, Van Cauwenberg J, Cerin E; Council on Environment and Physical Activity (CEPA) – Older Adults working group . Built environmental correlates of older adults’ total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cain KL, Millstein RA, Sallis JF, et al. . Contribution of streetscape audits to explanation of physical activity in four age groups based on the Microscale Audit of Pedestrian Streetscapes (MAPS). Soc Sci Med. 2014;116:82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cerin E, Nathan A, van Cauwenberg J, Barnett DW, Barnett A; Council on Environment and Physical Activity (CEPA) – Older Adults working group . The neighbourhood physical environment and active travel in older adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thornton CM, Kerr J, Conway TL, et al. . Physical activity in older adults: an ecological approach. Ann Behav Med. 2017;51(2):159–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Van Cauwenberg J, Nathan A, Barnett A, Barnett DW, Cerin E; Council on Environment and Physical Activity (CEPA)-Older Adults Working Group . Relationships between neighbourhood physical environmental attributes and older adults’ leisure-time physical activity: a systematic review and meta-analysis. Sports Med. 2018;48(7):1635–1660. [DOI] [PubMed] [Google Scholar]
- 12. King AC, King DK, Banchoff A, et al. . Employing participatory citizen science methods to promote age-friendly environments worldwide. Int J Environ Res Public Health. 2020;17(5):1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. U.S. Department of Health and Human Services. Step it up! The Surgeon General’s call to action to promote walking and walkable communities. 2016. Retrieved November 18, 2020, from https://www.surgeongeneral.gov/library/calls/walking-and-walkable-communities
- 14. Buman MP, Winter SJ, Baker C, Hekler EB, Otten JJ, King AC. Neighborhood Eating and Activity Advocacy Teams (NEAAT): engaging older adults in policy activities to improve food and physical environments. Transl Behav Med. 2012;2(2):249–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Corrado AM, Benjamin-Thomas TE, McGrath C, Hand C, Laliberte Rudman D. Participatory action research with older adults: a critical interpretive synthesis. Gerontologist. 2020;60(5): e413–e427. [DOI] [PubMed] [Google Scholar]
- 16. Mather M, Scommegna P.. Today’s Research on Aging: How Neighborhoods Affect the Health and Well-Being of Older Americans. Washington, DC: Population Reference Bureau; 2017. Retrieved November 8, 2020, from https://www.prb.org/resources/how-neighborhoods-affect-the-health-and-well-being-of-older-americans/. [Google Scholar]
- 17. Sallis JF, Cain KL, Conway TL, et al. . Is your neighborhood designed to support physical activity? A brief streetscape audit tool. Prev Chronic Dis. 2015;12:E141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Botchwey N, Jones-Bynes J, O’Connell K, Millstein RA, Kim A, Conway TL. Impact of a youth advocacy policy, systems and environmental change program for physical activity on perceptions and beliefs. Prev Med. 2020;136:106077. [DOI] [PubMed] [Google Scholar]
- 19. Sallis JF, Owen N, Fisher E. Ecological models of health behavior. Health Behav Theor Res Pract. 2015;5:43–64. [Google Scholar]
- 20. Bandura A. Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 21. Zimmerman MA, Rappaport J. Citizen participation, perceived control, and psychological empowerment. Am J Community Psychol. 1988;16(5):725–750. [DOI] [PubMed] [Google Scholar]
- 22. Rich P, Aarons GA, Takemoto M, et al. . Implementation-effectiveness trial of an ecological intervention for physical activity in ethnically diverse low income senior centers. BMC Public Health. 2017;18(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Millstein RA, Woodruff SI, Linton LS, Edwards CC, Sallis JF. Development of measures to evaluate youth advocacy for obesity prevention. Int J Behav Nutr Phys Act. 2016;13:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Coffman J, Hendricks A, Kaye JW, Kelly T, Masters B. The advocacy and policy change composite logic model. 2007. Retrieved November 8, 2020 from http://www.pointk.org/index.php?section_id=6&content_id=637
- 25. Tomioka K, Iwamoto J, Saeki K, Okamoto N. Reliability and validity of the International Physical Activity Questionnaire (IPAQ) in elderly adults: The Fujiwara-Kyo Study. J Epidemiol. 2011;21(6):459–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Linnan L, Steckler A.. Process Evaluation for Public Health Interventions and Research. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- 27. Marcoux MF, Sallis JF, McKenzie TL, Marshall S, Armstrong CA, Goggin KJ. Process evaluation of a physical activity self-management program for children: SPARK. Psychol Health. 1999;14(4):659–677. [Google Scholar]
- 28. Kirwan M, Duncan MJ, Vandelanotte C, Mummery WK. Design, development, and formative evaluation of a smartphone application for recording and monitoring physical activity levels: the 10,000 steps “iStepLog.” Health Educ Behav. 40(2):140–151. [DOI] [PubMed] [Google Scholar]
- 29. King AC, Sallis JF, Frank LD, et al. . Aging in neighborhoods differing in walkability and income: associations with physical activity and obesity in older adults. Soc Sci Med. 2011;73(10):1525–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. [DOI] [PubMed] [Google Scholar]
- 31. Keadle SK, McKinnon R, Graubard BI, Troiano RP. Prevalence and trends in physical activity among older adults in the United States: a comparison across three national surveys. Prev Med. 2016; 89:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Millstein RA, Woodruff SI, Linton LS, Edwards CC, Sallis JF. A pilot study evaluating the effects of a youth advocacy program on youth readiness to advocate for environment and policy changes for obesity prevention. Transl Behav Med. 2016;6(4):648–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee EE, Depp C, Palmer BW, et al. . High prevalence and adverse health effects of loneliness in community-dwelling adults across the lifespan: role of wisdom as a protective factor. Int Psychogeriatr. 2019;31(10):1447–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mama SK, Leach HJ, Soltero EG, Lee RE. Improved physical activity screening enhances intervention effectiveness in ethnic minority women: a longitudinal study. Health Promot Pract. 2017;18(1):54–61. [DOI] [PubMed] [Google Scholar]
- 35. Clemes SA, Deans NK. Presence and duration of reactivity to pedometers in adults. Med Sci Sports Exerc. 2012;44(6):1097–1101. [DOI] [PubMed] [Google Scholar]
- 36. Buman MP, Hekler EB, Haskell WL, et al. . Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ivers NM, Halperin IJ, Barnsley J, et al. . Allocation techniques for balance at baseline in cluster randomized trials: a methodological review. Trials. 2012;13:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.