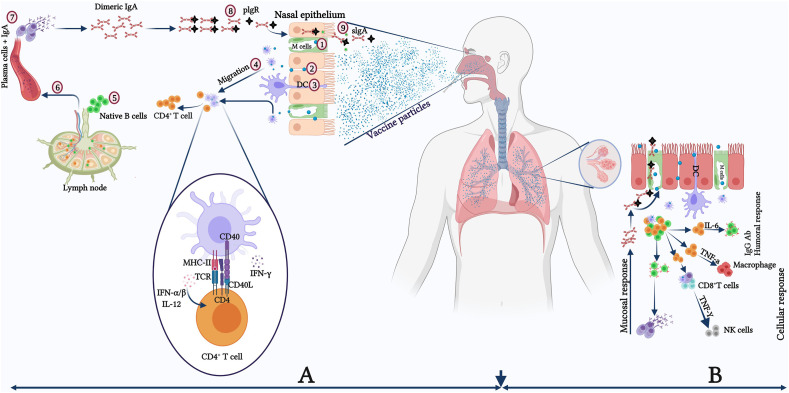
Fig. 1.
Schematic model of the potential effect of nasal vaccines on the upper and lower respiratory tract for the generation of mucosal and systemic immunity.(A) Protective immune responses in the nasopharynx-associated lymphoid tissue (NALT), with the virus-mediated reaction resulting mainly from secretory IgA antibodies generated by mucosal epithelial cells. (1) M cells actively take up antigens or penetrate epithelial junctions passively (2), DCs that extend into the lumen also take up antigens. (3). DCs acquire antigens and transport them to nearby lymphoid follicles or lymph nodes, where they are presented to CD4+ T-cells (4). CD4+ T cells activated by DCs activate naive B cells, causing them to switch isotype and become antigen-specific IgA+ committed B cells (5). These IgA+ B cells migrate from the lymph node to the blood circulations (6). Finally, IgA+ B cells exit the blood and enter towards the effector site. They undergo final differentiation and maturations producing IgA+ plasma cells (process enhanced by IL-5 and IL-6, a subset of Th2 cells) and ultimately form dimeric or polymeric IgA (7). The dimeric or polymeric IgA binds with pIgR in the basolateral region to form sIgA (8) and further transcytoses towards the apical side of the luminal surface (9). (B) Humoral immune response in the lower respiratory tract with bronchus-associated lymphoid tissue (BALT) having humoral as well as mucosal/local immune responses. DC: Dendritic cell; IL: Interleukin; M cell: Microfold cell; pIgR: Polymeric immunoglobulin receptor; sIgA: Secretory IgA; Th: T-helper cell.