Abstract
Aim:
We conducted an integrative review of the global-free maternity (FM) policies and evaluated the quality of care (QoC) and cost and cost implications to provide lessons for universal health coverage (UHC).
Methodology:
Using integrative review methods proposed by Whittemore and Knafl (2005), we searched through EBSCO Host, ArticleFirst, Cochrane Central Registry of Controlled Trials, Emerald Insight, JSTOR, PubMed, Springer Link, Electronic collections online, and Google Scholar databases guided by the preferred reporting item for systematic review and meta-analysis protocol (PRISMA) guideline. Only empirical studies that described FM policies with components of quality and cost were included. There were 43 papers included, and the data were analysed thematically.
Results:
Forty-three studies that met the criteria were all from developing countries and had implemented different approaches of FM policy. Review findings demonstrated that some of the quality issues hindering the policies were poor management of complications, worsened referral systems, overburdening of staff because of increased utilisation, lack of transport, and low supply of stock. There were some quality improvements on monitoring vital signs by nurses and some procedures met the recommended standards. Equally, mothers still bear the burden of some costs such as the purchase of drugs, transport, informal payments despite policies being ‘free’.
Conclusions:
FM policies can reduce the financial burden on the households if well implemented and sustainably funded. Besides, they may also contribute to a decline in inequity between the rich and poor though not independently. In order to achieve the SDG goal of UHC by 2030, there is a need to promote awareness of the policy to the poor and disadvantaged women in rural areas to help narrow the inequality gap on utilisation and provide a sustainable form of transport through collaboration with partners to help reduce impoverishment of households. Also, there is a need to address elements such as cultural barriers and the role of traditional birth attendants which hinder women from seeking skilled care even when they are freely available.
Key words: cost of care, free maternity policy, free delivery policy, quality of care, universal health coverage
Background
While maternal deaths have reduced by nearly 50% since 1990, the Sustainable Development Goals (SDGs) aim to further decrease the maternal mortality ratio (MMR) to less than 70 per 100 000 live births by 2030 (United Nations, 2017b). Many countries have made relatively little progress so far. A recent systematic analysis of maternal mortalities in 181 countries from 1980 to 2008 showed that while there was progress in achieving reduced MMR, only 23 countries including China, Egypt, Bolivia, and Ecuador were on track to achieve a considerable decrease of 75% (Hogan et al., 2010). From the global estimates of 2017, there are nearly 295 000 maternal mortalities that happen globally, mainly from complications related to pregnancy and childbirth (World Health Organisation, 2019). Low- and middle-income countries (LMICs) account for the majority of the high burden of the mortalities (Carrera, 2007). For instance, MMR in Benin is estimated at 405 deaths in 100 000 live births (Dossou et al., 2018), 575 in Nigeria (Oyeneyin et al., 2017), and as high as 1360 in Sierra Leone (Koroma et al., 2017). Poor use of lifesaving maternal services and family planning services contributes to the high MMR in developing countries which is 14 times higher than the developed countries (United Nations, 2017b).
Women are increasingly forming the backbone of many families as breadwinners (Amu, 2005), and their death can push the whole family to penury. Women’s increased risks of dying in pregnancy are primarily due to preventable causes (Koroma et al., 2017) such as haemorrhage, toxaemia, unsafe abortion, and obstructed labour (Hulton et al., 2000). In Sub-Saharan Africa (SSA), such deaths are mainly caused by lack of timely access to skilled delivery caused by the delayed decision by individuals and family to seek care, delay in getting to the health facility, and delay in the provision of adequate care by the facility. Gabrysch and Campbell (2009) identified and grouped 20 determinants that affect skilled institutional deliveries into four themes as socio-cultural factors, the perceived benefits and needs of skilled birth attendance, economic accessibility, and physical accessibility. Besides, they suggested the role of quality of care (QoC) which is, in most instances, not captured in household surveys, the role of distance, and the ability to pay. While increasing service availability is perceived as imperative, it does not always increase the use of the service (Hulton et al., 2000). Both the perceived and actual quality of maternal and neonatal healthcare are imperative because they influence the decision to seek healthcare.
On the other hand, high out-of-pocket (OOP) expenditure is increasingly forcing households into poverty (Xu et al., 2003). Globally, there are approximately 150 million who experience health-related catastrophic expenditure, of which 100 million fall into poverty (Xu et al., 2007). This health catastrophic expenditure is both in low- and high-income countries, but over 90% of people who suffer the most are in LMIC (Xu et al., 2003). An analysis of the nationally representative survey in Malaysia, Sri-Lanka, Indonesia, and Thailand showed that of the 2.7% of the population under survey, approximately 78 million remained with less than one-dollar-a-day after paying for health care and that the exemption policies, particularly for the more impoverished people, was an important strategy to mitigate such payments that could lead to impoverishment (Van Doorslaer et al., 2006).
Many countries have implemented financial incentives to address the element of QoC and outcome, catastrophic cost, and equitable utilisation of maternal healthcare services (Stanton et al., 2013) and to achieve universal health coverage (UHC). One such incentive is the removal of user fees for primary health care (PHC) which also covers maternal healthcare and is aimed at reducing pregnancy and childbirth-related morbidities and mortalities. One study that mapped countries that implemented free policies showed that of the 49 countries selected for mapping, more than half (28) were exclusively focusing on free delivery care or were being implemented together with other curative services (Witter, 2010).
This integrative review (IR) limits itself to analysing the QoC and outcome, and the cost implications of free maternity (FM)/delivery policies to provide lessons for UHC. The review complements the findings on the utilisation of services under FM policies – links with existing literature on utilisation because many prior analyses have mainly focused on comparing the changes in utilisation of services before and after the implementation of the free policies (Ridde, 2003; Masiye et al., 2008; Nabyonga-Orem et al., 2008). Some studies that have gone beyond evaluating the changes in utilisation before and after the free policy have mainly focussed on the preventative and curative care themes (Lagarde et al., 2012) and not maternal health services. Therefore, this review focuses on the free maternal or delivery healthcare policies as implemented globally.
Purpose of the integrative review study
The review answers the following questions:
What are the approaches to implementation of FM policy?
What is the quality (care and outcomes) and the cost implications about policy and practice that legislate for the free global maternity care?
What lessons can we learn from the global FM policy to support the achievement of UHC?
Methods
Study design
The study utilised the integrative literature review, which allows for the synthesis of several streams of literature (Whittemore and Knafl, 2005; Yorks, 2008). The method was useful for reviewing, critiquing, and synthesising evidence from research in an integrative way that allowed new perspectives and frameworks to be drawn (Christmals and Gross, 2017; Rosa et al., 2017). In particular, the study included a wide range of literature from several fields of study which were analysed through a multidisciplinary approach. Also, the study focused on peer-reviewed literature, models, frameworks, policy documents on free maternal/delivery policies that reported on elements of quality and cost of care and outcomes.
Search methods
We searched for articles in databases and sources, as shown in Table 1. All articles that met the criteria were included irrespective of the year of publication. We then reviewed the bibliographies of all studies identified after which we reached the saturation point and provided a comprehensive list that was validated by SK. Boolean operators (OR and AND) were used to limit and expand the search as appropriate. We had four sets of search terms (Table 2) adapted and modified from Ridde and Morestin (2010) and Ridde et al. (2012c) which were combined using OR within each set and AND linking different sets. All searches were imported to Endnote library and pooled, after which duplicates were removed.
Table 1.
Source of evidence
| e-journal services and electronic databases | Applied social sciences index and abstracts, EBSCO Host (Academic search complete, Cumulative Index to Nursing and Allied health Literature (CINAHL), Econ Lit, MEDLINE, and PsycINFO), ArticleFirst, Cochrane Central Registry of Controlled Trials (Cochrane Library, Wiley Online Library), Emerald Insight, JSTOR, PubMed, Springer Link (Springer Reference), Google scholar, and Electronic Collections Online. |
| Health Sources | International Bibliography of the Social Sciences, SAGE journals Online, Nursing/Academic Edition, Latin-American and Caribbean Centre on Health Sciences Information (LILACS), African Journals Online, SCOPUS, Science Direct, Web of Science (Web of Knowledge & Science Citation Index), OVID (Social Policy and Practice). |
| Websites on health financing | World Health Organisation, The World Bank, Mednar, Intute, Nexis UK, Qual page, Scirus, WorldWideScience.org, and Eldis |
| Grey Literature | SIGLE database |
Table 2.
Search words
| (“User fee*” OR “user charg*” OR “cost shar*” OR “cost recover*” OR “User Fee* Policy” OR “User Policy”)) AND |
| (“Free polic*” OR “Free policy” OR “Free Health*” OR “Free Car*” OR “free care” OR “Discontin*” OR “Abol*” OR “exempt*” OR “waiv*” OR “Remov*” OR “end*” OR “Policy Chang*” OR “Chang*” OR “implement*” OR “Policy implement*”)) AND |
| (“matern*” OR “deliver*” OR “Mother car*” OR “baby car*” OR “infant car*” OR “matern* car*” OR “deliver* car*” OR “giv* birth” OR “labour” OR labor OR mother*” OR “Childbirth*” OR “birth” OR “parturit*” OR “accouch*”)) AND |
| (“Quality” OR “quality car*” OR “health care quality” OR “quality outcome*” OR “cost*” OR “Expenditure” OR “Economic*” OR “Financ*” OR “effective Cover*” OR “Universal Care” OR “Universal Health Cover*” OR “Universal Health” |
Selection criteria
The review was limited to studies conducted in English that reported the concepts of implementation, quality and cost of care and outcomes of FM policies, and lessons for UHC. We included all study types, and the final review included experimental studies, quantitative, qualitative, and mixed-method studies done in single or multiple countries. Some of the excluded studies had no relevance to healthcare, had a poor methodological approach, and were talking about free maternity services (FMS) but not the quality or cost of the free maternal healthcare policy. First, all titles were screened for eligibility. Second, studies that met eligibility had their abstract further screened for eligibility after which full texts were screened for those studies that meet the eligibility criteria. All articles were included irrespective of the date. Figure 1 shows the search outcomes.
Figure 1.
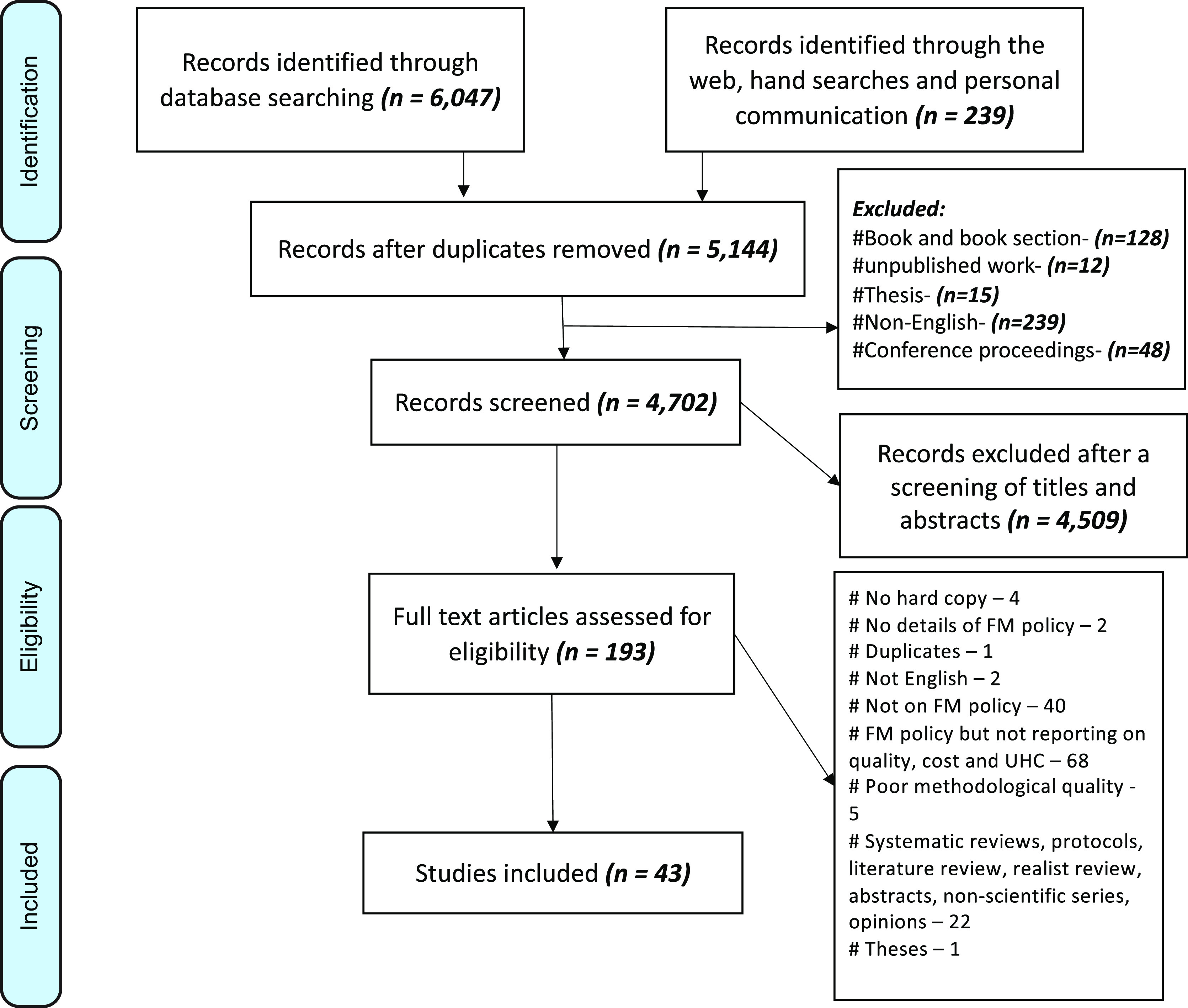
Flow chart of the selection of studies for review
Quality appraisals
In this review, we did not do meta-analysis because there was much heterogeneity in the studies. We applied a mix of validated critical quality appraisal techniques (Wechkunanukul et al., 2017). First, we applied the checklist for writing an integrative review as stipulated by Toracco (2005) and utilised the Preferred Reporting Item for Systematic Reviews and Meta-Analysis (PRISMA) checklist for reporting systematic reviews (Moher et al., 2015) (Figure 1). For the quality appraisal of the individual study designs, we applied the Critical Appraisal Skills Programme (CASP) tools (Critical Appraisal Skills Programme, 2017a; 2017b; 2017c; 2017d; 2017e; 2017f, 2017g; 2017h). All the articles were, through a sampling technique, evaluated by a second researcher at the last stage, and where there was disagreement, the resolution was made through consultation.
Data abstraction, analysis and evaluation
There were five steps applied in this review: data reduction, display, comparison, concluding, and verification (Torraco, 2005; Whittemore and Knafl, 2005; Wechkunanukul et al., 2017). Data reduction was classified by the subgroup classification of studies based on research design. Data were abstracted and entered into Microsoft Excel®, from where the synthesis of the text was done through thematic analysis using variables of interest and conclusions are drawn.
Definitions and frameworks
Quality cannot be measured by itself (Kelley and Hurst, 2006) and Donabedian broadly classifies it as structure, process, and outcome dimensions (Donabedian, 1988; Donabedian, 1990) which can be identified, measured, and attributed to healthcare. Structure indicators represent pointers which are inputs to or characteristics of health; process indicators represent gauges to either appropriate or inappropriate care in a targeted population which are “consistent with current professional knowledge”; outcome indicators are the measures of both improved or deteriorated health and is attributed to medical care (Kelley and Hurst, 2006). In this review, we broadly defined QoC using the quality of maternal and newborn healthcare framework as proposed by the World Health Organisation (WHO) (2016). There are eight domains of QoC in the framework that targets mothers and their newborns in the health system (hospitals), making it likely to achieve the desired individual and facility-level outcome. The approach gives two quality improvement standards: provision and experience of care. Provision of care supports evidence-based practices for routine care and management of complications, actionable information system, and functional referral system, while the experience of care supports effective communication, respect and preservation of dignity, and emotional support. There are two cross-cutting areas of QoC, namely: competent, motivated human resources and essential physical resources available.
On the other hand, increased cost of care is repeatedly attributed to the cause of reduced use of services (Mekonnen and Mekonnen, 2003). In this review, costs elements are defined thematically from the perspective of the patients, provider, and the policymakers (Figure 2).
Figure 2.
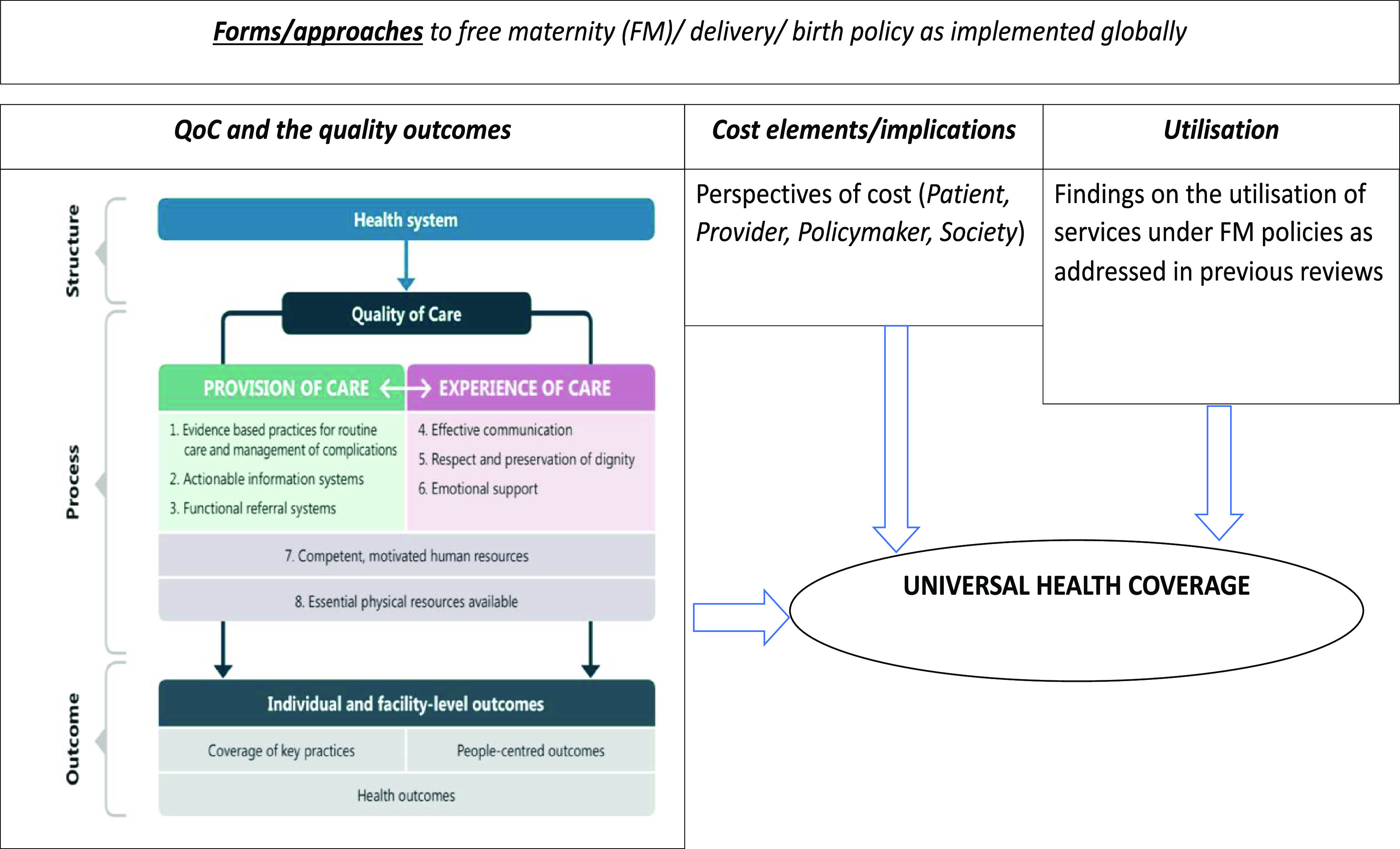
Analysis framework (Source: Review of literature and WHO framework for the quality of maternal and newborn health care)
Results
Description of the studies
Additional file 1 shows an overview of all the papers included in the review. The IR identified 6047 articles published without date restriction until December 2017 and an addition of 239 identified through the web, hand searches, and personal communications. After filtering for duplicates, 5,144 articles were considered for review. The articles then had their titles and abstracts screened for eligibility for which 43 articles met all the criteria and thus included in the final stage of data abstraction (Additional file 1).
The quality scores of the individual studies are reported in Additional file 1. The quality appraisal of 21 studies included in the review was rated as high because they reported sufficient details about the FM policy and highlighted robust methodologies with findings according to the appraisal tools used (Witter et al., 2007; Masiye et al., 2010; Witter et al., 2010; Nimpagaritse and Bertone, 2011; Steinhardt et al., 2011; Witter et al., 2011; Ameur et al., 2012; Ridde et al., 2012b; Witter et al., 2012; Arsenault et al., 2013; Ridde et al., 2013; Ganle et al., 2014; Delamou et al., 2015; Ravit et al., 2015; Ridde et al., 2015; Boukhalfa et al., 2016; Ganaba et al., 2016; Witter et al., 2016; Chankham et al., 2017; Ensor et al., 2017; Witter et al., 2017); 13 studies were rated medium (Asante et al., 2007; Bosu et al., 2007; Kruk et al., 2008; Nabyonga-Orem et al., 2008; Ridde and Diarra, 2009; Ridde et al., 2012a; The World Bank, 2013; Chama-Chiliba and Koch, 2014; Philibert et al., 2014; Chama-Chiliba and Koch, 2016; Lange et al., 2016; Dalinjong et al., 2017; Koroma et al., 2017); and six studies were rated low because they either did not report their study design or their description of the method section was not sufficient but captured enough information on the FM policy (Nahar and Costello, 1998; Khan, 2005; Kenya Ministry of Health, 2015; Sidze et al., 2015; Vallières et al., 2016; Edu et al., 2017). One study did not address the criteria for methodological quality (Luwei et al., 2011).
On study designs, two studies did not outrightly indicate the study design but indicated their study methods (Luwei et al., 2011; Sidze et al., 2015); eleven utilised a cross-sectional design (Nahar and Costello, 1998; Khan, 2005; Asante et al., 2007; Bennis and De Brouwere, 2012; Ridde et al., 2012a; The World Bank, 2013; Ridde et al., 2015; Boukhalfa et al., 2016; Vallières et al., 2016; Chankham et al., 2017; Koroma et al., 2017); four case control designs (Ameur et al., 2012; Arsenault et al., 2013; Philibert et al., 2014; Ravit et al., 2015); one cohort study (Nabyonga-Orem et al., 2008), and seven case studies (Masiye et al., 2010; Nimpagaritse and Bertone, 2011; Ridde et al., 2012b; Philibert et al., 2014; Ganaba et al., 2016; Witter et al., 2016; Witter et al., 2017). Other study designs indicated in the papers were: one interrupted time series design (Chama-Chiliba and Koch, 2016); 3 quasi-experimental design studies (Chama-Chiliba and Koch, 2014; Philibert et al., 2014; Ensor et al., 2017); three studies had components of before and after intervention study design (Bosu et al., 2007; Masiye et al., 2010; Witter et al., 2011); one descriptive convergent parallel mixed method design (Dalinjong et al., 2017); and one mixed method sequential explanatory design (Ridde et al., 2013). The other studies were evaluations studies that applied varied evaluation approaches (and not one specific design). For instance, three studies used realist approaches (Ganle et al., 2014; Witter et al., 2016; Witter et al., 2017); one descriptive and analytical implementation evaluation (Ridde et al., 2013) and another policy implementation evaluation (Witter et al., 2012); two process evaluations with varied designs (Ridde and Diarra, 2009; Witter et al., 2013); one monitoring and evaluation using mixed methods (Kenya Ministry of Health, 2015); and one monitoring and evaluation using a before and after study design (Witter et al., 2011). Others are one outcome evaluation (Steinhardt et al., 2011), one policy baseline evaluation (Witter et al., 2007), and another policy evaluation (Witter et al., 2010). See Additional file 1.
A closer analysis of the articles revealed that three articles were multi-country studies, with two of them reporting on both low-income countries (LIC) and LMIC countries (Witter et al., 2016; Witter et al., 2017), one being a transversal analysis of entirely LICs (Ridde et al., 2012b), 21 evaluated singular counties that were LICs (Kruk et al., 2008; Nabyonga-Orem et al., 2008; Ridde and Diarra, 2009; Witter et al., 2010; Luwei et al., 2011; Nimpagaritse and Bertone, 2011; Steinhardt et al., 2011; Witter et al., 2011; Ameur et al., 2012; Ridde et al., 2012a; Arsenault et al., 2013; Ridde et al., 2013; Philibert et al., 2014; Delamou et al., 2015; Ravit et al., 2015; Ridde et al., 2015; Ganaba et al., 2016; Lange et al., 2016; Vallières et al., 2016; Ensor et al., 2017; Koroma et al., 2017), and 19 were in LMICs (Nahar and Costello, 1998; Khan, 2005; Asante et al., 2007; Bosu et al., 2007; Witter et al., 2007; Masiye et al., 2010; Bennis and De Brouwere, 2012; Witter et al., 2012; The World Bank, 2013; Witter et al., 2013; Chama-Chiliba and Koch, 2014; Ganle et al., 2014; Kenya Ministry of Health, 2015; Sidze et al., 2015; Boukhalfa et al., 2016; Chama-Chiliba and Koch, 2016l Chankham et al., 2017; Dalinjong et al., 2017; Edu et al., 2017). No work from high income country (HIC) met the criteria. See Additional file 1.
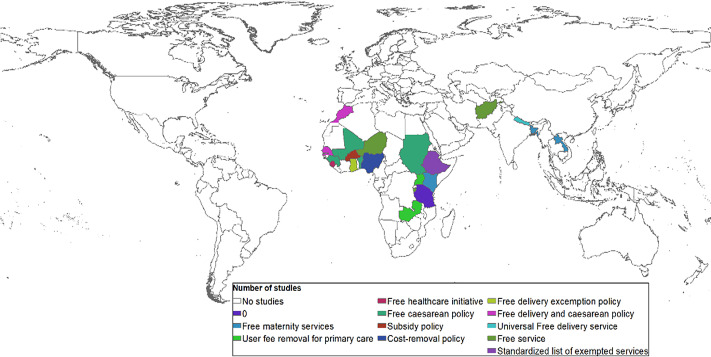
Forms of free maternity policy by different countries
The review found different forms of the FM policies, which are mainly implemented in LICs and LMICs (Figure 3). The FM policy processes of several countries that were reviewed required a significant amount of resources, political processes, and social institutions to institutionalise, maintain, or shape their structures (Lightman and Lightman, 2017). In some countries, the processes were well planned to use the steps of the stage heuristic model, others required a window of opportunity to implement, and some were born out of need.
Figure 3.
Forms of policy implementation of free maternity policy (Source: authors mapped from review of literature)
Quality of maternal care
The QoC and outcome reported in this section utilised the WHO proposed framework (World Health Organisation, 2016) from the perspective of the managers, service providers, and users in two aspects: provision and experience of care.
Provision of care
The findings on provision of care are in three main areas: evidence-based practices for routine care and management of complications, actionable information systems, and functional referral system.
Evidence-based practices for routine care and management of complications
Eight studies reviewed had positive, evidence-based practices for routine care and management of complication with the FM Policy (Bosu et al., 2007; Steinhardt et al., 2011; Delamou et al., 2015; Kenya Ministry of Health, 2015; Sidze et al., 2015; Vallières et al., 2016; Witter et al., 2016; Edu et al., 2017; Koroma et al., 2017), seven studies had contrary evidence (Witter et al., 2007; Witter et al., 2012; Sidze et al., 2015; Ganaba et al., 2016; Lange et al., 2016; Witter et al., 2016; Koroma et al., 2017), while three showed no change after implementation of FM policy (Luwei et al., 2011; Kenya Ministry of Health, 2015; Chama-Chiliba and Koch, 2016).
For instance, the authors linked the policies to improved perception of QoC index by hospitals (Steinhardt et al., 2011) and mothers (Koroma et al., 2017). FM policies have been linked with an increase in the number of ANC visits (Kenya Ministry of Health, 2015), improved screening for vital signs such as weight, foetal movements (Koroma et al., 2017), measurements of BP (Sidze et al., 2015; Koroma et al., 2017), screening of urine and blood, and maternal immunisation for tetanus at ANC (Sidze et al., 2015). Equally, they were linked with increased immunisation of children (Vallières et al., 2016) and more mothers being counselled on breastfeeding and pregnancy-related complication during ANC (Sidze et al., 2015). Maternal complications were either identified early, referred and hospitalised as appropriate (Delamou et al., 2015; Edu et al., 2017), or declined (Kenya Ministry of Health, 2015), leading to reduced maternal deaths (Bosu et al., 2007; Kenya Ministry of Health, 2015). Importantly, the policies are associated with a reduction in the stillbirths, underweight babies, and preterm babies (Kenya Ministry of Health, 2015). Significantly, there was a reduced transmission of HIV at birth from mother to child (Kenya Ministry of Health, 2015), and some hospitals had the best technical quality care measured by reduced delays, low omission scores, and low fatality rates for adverse complications (Witter et al., 2016).
In some policies, the HCWs were poorly using the partograph (Witter et al., 2007), others were not adhering to treatment guidelines and procedures (Witter et al., 2012) or were using treatment methods perceived as not sterile (Lange et al., 2016). Others had critical omissions in routine procedures (Witter et al., 2016) and even concentrated more on complicated and surgical deliveries than vaginal deliveries (Ganaba et al., 2016). From a hospital perspective, facilities were unable to manage emergencies such as infections, pre-eclampsia, haemorrhage, anaemia, breech birth because they lacked essential lifesaving skills and emergency equipment (Koroma et al., 2017). Others showed increased maternal complications such as obstructed labour (Sidze et al., 2015) and increased burden of maternal and neonatal near misses (Witter et al., 2016).
Luwei et al. (2011) revealed that there was little significant difference between facilities providing free care and facilities charging a fee on the standard parameters of quality such as the use of a partograph to monitor labour, availability of oxytocin, managing direct obstetric complications, and the availability of new-born resuscitation procedures. There was limited evidence of better patient safety measures and of assuring/monitoring adherence to expected care standards (Kenya Ministry of Health, 2015). In Zambia, a before and after analysis of the free primary care demonstrated that there was little or insignificant difference in uptake of ANC despite the likelihood of good quality of ANC influencing the use of a health facility for delivery (Chama-Chiliba and Koch, 2016).
Actionable information systems
Only two studies reported on information system (Ridde and Diarra, 2009; Chankham et al., 2017). Ridde and Diarra (2009) in their process evaluation of FM services in Niger highlighted that the new policy introduced a parallel operating system to the already existing system which meant that the HCWs mainly had to provide care to different groups of patients registered in the free program and the old program resulting to increased workload. Chankham et al. (2017) noted that the provision of information at the health facilities enhanced satisfaction with the quality-of-service provision.
Functional referral
Nine studies reviewed reported on the element of the referral system relating to FM policies (Witter et al., 2007; Ridde and Diarra, 2009; Nimpagaritse and Bertone, 2011; Ridde et al., 2012b; The World Bank, 2013; Ganle et al., 2014, Delamou et al., 2015; Sidze et al., 2015; Edu et al., 2017). Studies showed that FM policies resulted in proper referral where patients were referred from lower-level to higher-level facilities (Sidze et al., 2015; Edu et al., 2017) which in turn resulted in early detection of and reduced complications (Edu et al., 2017). Reimbursement strategies played a role in referral. For instance, hospital reimbursement strategies that were pegged on successful referral helped to improve quality outcomes (Witter et al., 2007). However, reimbursing hospitals based on the number and type of deliveries conducted resulted in some unintended consequences. Some unintended consequence included lower facilities not referring patients for fear of losing revenue as is the case of Ghana (Witter et al., 2007), or HCWs choosing caesarean section over normal birth even if unwarranted for higher revenues as the case in Laos PDR (The World Bank, 2013).
With regard to the implementation of the FM policies, it was evidenced that there was uncoordinated and unreimbursed referral strategies (Witter et al., 2007) and some faced lack of critical staff to handle referred emergencies (Ganle et al., 2014). In some counties such as Guinea, there was a significant decrease in unmet obstetric need after implementation of the policy as hospitals were incentivised to handle complications hence reduce referral (Delamou et al., 2015). By including the transport component to the FM policy, there was improved satisfaction outcomes and satisfaction with the services (Ridde et al., 2012b). However, specific gaps in referral after policy implementation such as inadequate or lack of follow-up to ensure the evacuated mothers received care as intended (Ridde and Diarra, 2009) or in cases where implementation is done rapidly, there was a disruption of referral system (Nimpagaritse and Bertone, 2011).
Experience of care
The findings on the experience of care highlight three main areas of quality: cognition and effective communication, respect and preservation of dignity, and emotional support.
Cognition and effective communication
Three studies highlighted how cognition and effective communication influenced perception or technical elements of quality (Lange et al., 2016; Witter et al., 2016; Edu et al., 2017). How the HCWs communicated to the mothers determined their perception of confidence in handling complications (Edu et al., 2017). The studies showed that the nurses had not well-informed mothers about delivery procedures and that there was lack of proper reason for the procedure in cases of emergency (Lange et al., 2016). Equally, poor communication between HCWs and mothers influenced the lack of informed consent for surgery and poor bedside manners (Witter et al., 2016). Besides, nurses took time to decide between having to do a CS or normal delivery with inconsistencies in scheduling a CS because of the surgeon’s unavailability (Lange et al., 2016). Mothers perceived some negligence by HCWs who provided inadequate care and support of the perineum during vaginal delivery (Lange et al., 2016).
Respect and preservation of dignity
Eight studies reviewed highlighted components of respect and preservation of dignity (Witter et al., 2007; Nabyonga-Orem et al., 2008; Masiye et al., 2010; Ganle et al., 2014; Philibert et al., 2014; Kenya Ministry of Health, 2015; Witter et al., 2016; Edu et al., 2017). Some highlighted respect concerns were harsh treatment from some HCWs (Edu et al., 2017), negative attitude towards the women (Witter et al., 2007; Ganle et al., 2014), staff being too few, rude, and not available when required (Nabyonga-Orem et al., 2008), and poor interpersonal relationship between the mothers and HCWs (Witter et al., 2016). In relation to this, the women distrusted the knowledge, practices, skills, and competence of the maternal healthcare providers mothers because they were chided and scolded for not attending ANC early and a high throughput of patients made it difficult to maintain privacy for the mothers during procedures (Ganle et al., 2014).
However, some studies showed that HCWs had shown a kind attitude (Edu et al., 2017) and excellent interpersonal skills (Kenya Ministry of Health, 2015) towards pregnant mothers. Others had little indication to propose that staff courtesy had deteriorated after the policy change (Masiye et al., 2010), or that the provider–patient interaction, nursing care, and the delivery environment had changed (Philibert et al., 2014).
Emotional support
Only one study reviewed showed captured elements of emotional support. The study showed that mothers who were experiencing difficulty with breastfeeding had received emotional support from their HCWs, who provided adequate breastfeeding counselling (Sidze et al., 2015).
The aspect that cut across both provision and experience of care
Competent, motivated human resource and essential physical resources available are two QoC areas that cut across both provision and experience of care and that do not fit across the eight categories.
Competent, motivated human resource
Sixteen studies reviewed highlighted the components of competency and motivation of HCWs following the implementation of FM policies (Bosu et al., 2007; Witter et al., 2007; Nabyonga-Orem et al., 2008; Masiye et al., 2010; Nimpagaritse and Bertone, 2011; Witter et al., 2011; Witter et al., 2012; Ganle et al., 2014; Kenya Ministry of Health, 2015; Sidze et al., 2015; Lange et al., 2016; Vallières et al., 2016; Witter et al., 2016; Chankham et al., 2017; Koroma et al., 2017; Witter et al., 2017). Factors that were highlighted as determinants of competency and motivation were functionality of infrastructure (Witter et al., 2012), the type of working conditions (Vallières et al., 2016), presence or absence of incentives from reimbursements for services (Witter et al., 2012; Vallières et al., 2016; Koroma et al., 2017), transparency in the use of reimbursements by in charges (Masiye et al., 2010), timeliness of reimbursements (Kenya Ministry of Health, 2015), weak guidance on the use of reimbursements (Kenya Ministry of Health, 2015), flexibility in the use of reimbursement to reward HCWs by hospitals (Witter et al., 2011; Lange et al., 2016), and changes in workload following free policies(Witter et al., 2007; Nimpagaritse and Bertone, 2011; Witter et al., 2011; Witter et al., 2012; Ganle et al., 2014; Kenya Ministry of Health, 2015; Lange et al., 2016; Vallières et al., 2016; Witter et al., 2016; Koroma et al., 2017; Witter et al., 2017).
The factors highlighted above resulted in increased corruption by the HCWs as a result of the loss of incentive that came with user fees (Witter et al., 2012; Lange et al., 2016) or poor pay (Lange et al., 2016), difficulty in recruitment of HCWs because of poor working conditions (Vallières et al., 2016), unequal distribution of HCWs because of the functionality of infrastructure (Witter et al., 2012). In some cases where workload increased, there was reduced productivity by the HCW (Witter et al., 2016) which saw them spend less time with mothers as a way of coping with the higher numbers at the clinic (Edu et al., 2017). Though, in others, the policy resulted in better birth outcomes and more deliveries due to HCWs working longer hours (Bosu et al., 2007; Witter et al., 2017) which Witter et al. (2017) called an efficiency gain. Some HCWs perceived workload as acceptable (Ganaba et al., 2016) or reasonable (Witter et al., 2017) since nurses took an equal amount of time with the patients like before the policy (Masiye et al., 2010). Despite the workload changes, often the mothers and HCWs perceived either increased waiting times resulting from the policies (Witter et al., 2012; Ganle et al., 2014; Sidze et al., 2015; Witter et al., 2016) or waiting times that remained the same (Masiye et al., 2010; Chankham et al., 2017) but were highly satisfied with the staff behaviour and because of the belief that they were dedicated and working beyond their abilities to cater to the increase in the workload (Nabyonga-Orem et al., 2008; Witter et al., 2012).
Essential physical resources available
Fifteen studies reviewed showed mixed findings on physical resources, medication, and equipment (Nabyonga-Orem et al., 2008; Ridde and Diarra, 2009; Masiye et al., 2010; Nimpagaritse and Bertone, 2011; Steinhardt et al., 2011; Witter et al., 2011; Ridde et al., 2012b; Chama-Chiliba and Koch, 2014; Kenya Ministry of Health, 2015; Sidze et al., 2015; Boukhalfa et al., 2016; Ganaba et al., 2016; Witter et al., 2016; Chankham et al., 2017; Edu et al., 2017). Some of the components of physical resources that were perceived positively by both the HCWs and patients after the FM policy implementation were improved physical condition and cleanliness of hospitals (Masiye et al., 2010) and the health facility environment (Chankham et al., 2017). In other aspects, availability of amenities such as water and toilets in the majority of the health facilities (Kenya Ministry of Health, 2015), unrestricted access to latrines, and more use of treated water (Witter et al., 2016) were perceived positively. However, two studies reported that there was lack of or unstable electricity coupled with a lack of or inadequate water facilities in the hospitals after the free policy (Nabyonga-Orem et al., 2008; Edu et al., 2017), and one showed that there was no consistent evidence of an increase in investments on things such as infrastructure (Kenya Ministry of Health, 2015).
In terms of medication and equipment, there was a perceived readiness of medicine and medical equipment after the policy implementation (Chankham et al., 2017), increase in drug availability (Nabyonga-Orem et al., 2008; Ridde and Diarra, 2009; Masiye et al., 2010; Chama-Chiliba and Koch, 2014), and adequate and well-organised supply of drugs (Ridde and Diarra, 2009). In cases where the drugs were not available, HCWs in Uganda sent the patients to buy them from the private clinics and drug shops (Nabyonga-Orem et al., 2008). Also, in Niger, HCWs were even educated on using essential generic drugs and new treatment protocols, especially for malaria (Ridde and Diarra, 2009). Eight studies highlighted increased shortages of drugs after the implementation of the policy (Nabyonga-Orem et al., 2008; Nimpagaritse and Bertone, 2011; Witter et al., 2011; Ridde et al., 2012b; Sidze et al., 2015; Boukhalfa et al., 2016; Ganaba et al., 2016; Edu et al., 2017) in addition to constrained equipment and other consumables (Nabyonga-Orem et al., 2008; Witter et al., 2011; Ganaba et al., 2016). Despite the shortages, the interviewed HCWs painted a rosy picture of the drug situation in Morocco (Boukhalfa et al., 2016) and Nepal (Witter et al., 2011). One study showed that there was no negative impact on the availability of drugs despite increased care-seeking behaviour by the patients after removal of fees (Steinhardt et al., 2011).
Other quality elements
Four studies highlighted the roles of traditional birth attendants (TBA) as an influencer or a hinder to the achievement of QoC (Chama-Chiliba and Koch, 2014; Ganle et al., 2014; Vallières et al., 2016; Edu et al., 2017). Two studies showed that the choice to be attended to by TBA, rather than skilled personnel in the health facility, particularly in the rural areas could not be adjusted by the changes in the cost of delivery (Chama-Chiliba and Koch, 2014; Vallières et al., 2016). The negative experiences of delivery under the new policy were pushing the mothers to TBAs (Ganle et al., 2014). One study showed that some mothers chose to deliver in health centres rather than through TBAs because of the poor QoC that was received in a previous pregnancy conducted by TBAs (Edu et al., 2017).
Cost elements of free maternal care
This section reports on the elements of cost of maternal care from the perspective of the managers, service providers, and users through thematic analysis.
Out-of-pocket (OOP) expenditures
Twenty-three of the reviewed studies showed that households in different countries still bear the burden of OOP expenditure despite the implementation of FM policies (Nahar and Costello, 1998; Khan, 2005; Kruk et al., 2008; Masiye et al., 2010; Witter et al., 2010; Luwei et al., 2011; Nimpagaritse and Bertone, 2011; Witter et al., 2011; Ameur et al., 2012; Bennis and De Brouwere, 2012; Witter et al., 2012; Arsenault et al., 2013; Ridde et al., 2013; Delamou et al., 2015; Ravit et al., 2015; Ridde et al., 2015; Boukhalfa et al., 2016; Chama-Chiliba and Koch, 2016; Ganaba et al., 2016; Lange et al., 2016; Vallières et al., 2016; Witter et al., 2016; Chankham et al., 2017; Edu et al., 2017). Some of the costs families are bearing include food (Nahar and Costello, 1998; Khan, 2005; Witter et al., 2011; Bennis and De Brouwere, 2012; Witter et al., 2012; Ravit et al., 2015; Boukhalfa et al., 2016; Chama-Chiliba and Koch, 2016), drugs and other medical supplies (Nahar and Costello, 1998; Khan, 2005; Kruk et al., 2008; Witter et al., 2010; Luwei et al., 2011; Arsenault et al., 2013; Ridde et al., 2013; Ravit et al., 2015; Boukhalfa et al., 2016; Lange et al., 2016; Vallières et al., 2016; Witter et al., 2016; Chankham et al., 2017), laboratory and other diagnostic tests (Nahar and Costello, 1998; Khan, 2005; Kruk et al., 2008; Witter et al., 2011), lodging or accommodation of the mothers or their accompanying relatives (Kruk et al., 2008; Witter et al., 2010; Chama-Chiliba and Koch, 2016; Witter et al., 2016), transport (Nahar and Costello, 1998; Khan, 2005; Kruk et al., 2008; Witter et al., 2010; Bennis and De Brouwere, 2012; Arsenault et al., 2013; Ravit et al., 2015; Vallières et al., 2016; Witter et al., 2016; Edu et al., 2017), either because it was not part of the policy or was part but caused significant burden, blood transfusions (Witter et al., 2011; Ravit et al., 2015; Lange et al., 2016), wound cleaning (Witter et al., 2011; Lange et al., 2016), and other complications (Witter et al., 2010). Other causes of OOP were referral (Bennis and De Brouwere, 2012), issuance of a child with a birth certificate (Ridde et al., 2013), a family certificate to be able to access the free services (Nimpagaritse and Bertone, 2011), care of new-born (Lange et al., 2016; Witter et al., 2016), hiring nurse aid (Nahar and Costello, 1998), and hospital admission fee (Khan, 2005). One study estimated the opportunity cost of for temporarily ceasing work as a result of hospitalisation (Bennis and De Brouwere, 2012).
The OOP paid by the households differed based on type and complexity of delivery (Nahar and Costello, 1998; Witter et al., 2007; Luwei et al., 2011; Ravit et al., 2015; Boukhalfa et al., 2016), type of hospital (Bennis and De Brouwere, 2012; Ganaba et al., 2016), distance to the hospital (Arsenault et al., 2013), area or residence whether rural or urban (Ravit et al., 2015), income level and education (Nahar and Costello, 1998; Khan, 2005), and the type of interviewee (Ameur et al., 2012; Ridde et al., 2012b, Ridde et al., 2013). For instance, mothers who underwent CS and complicated delivery had more OOP than those who had a normal delivery or assisted birth (Luwei et al., 2011; Boukhalfa et al., 2016). Also, the average cost of giving birth was lower in the district hospital than the regional hospital as regional hospitals were specialised hospitals (Ganaba et al., 2016). Mothers who were living closer to the health facility were paying less OOP than those living far (Arsenault et al., 2013), and women in rural areas spent more (Ravit et al., 2015). In Bangladesh, 21% of interviewed families revealed that they were spending more than half their monthly income on maternal care, while 27% reported spending 1–8 times the income (Nahar and Costello, 1998). Also, couples with better income and education were more willing to pay OOP expenditure (Nahar and Costello, 1998). There has been differing opinion between the amounts and causes of OOP expenditure between the HCWs and patients (Ameur et al., 2012; Ridde et al., 2012b, Ridde et al., 2013) with the patients overstating the cost and HCW indicating that lack of the essential materials was due to implementation gap of the policy which created the shortages (Ameur et al., 2012).
Catastrophic expenditure
Five studies highlighted the element of catastrophic expenditure (Witter et al., 2012; Arsenault et al., 2013; The World Bank, 2013; Ganle et al., 2014; Dalinjong et al., 2017). Catastrophic expenditure is the consequence of suffering the burden of disease by households whose OOP spending in healthcare is more than a certain threshold of household income (Ekman, 2007; Li et al., 2012). Highlighted cause of catastrophic expenditure was expensive, lengthy drug therapies required particularly for eclampsia and post-partum infections (Arsenault et al., 2013), and emergency blood transfusion (Arsenault et al., 2013; Dalinjong et al., 2017) hospitalisation cost, consultation, lab test, transport, meals during inpatient visit (Dalinjong et al., 2017), and other cost related to the policy-making healthcare spending more expensive than the food (Witter et al., 2012). Others were the prohibitive cost of travelling to the health care facility to seek free treatment or for free birth was making them choose to self-medicate over the visit (Ganle et al., 2014). The World Bank (2013) showed that the mode of delivery determined OOP spending in childbirth (whether vaginal or CS), choice of institution (whether public or private), cultural practices, and level of the health facility.
The financial effect of the policy on facilities
Nine studies highlighted the financial effects free policies had on the facilities (Witter et al., 2007; Witter et al., 2011; Witter et al., 2012; The World Bank, 2013; Chama-Chiliba and Koch, 2016; Witter et al., 2016; Dalinjong et al., 2017; Ensor et al., 2017). Due to funding differences, facilities in Morocco had a considerable increase of healthcare budget to support the implementation of the free caesarean policy (Witter et al., 2016), while in Sudan, facilities were facing a shortfall in funding, particularly remote ones (Witter et al., 2012). Different reimbursement strategies incentivised the facilities differently. For instance, Zambian facilities faced higher ANC uptake due to reduced direct costs that the patients used to face before the policy, and they reported that their income that they had been using to incentivise TBAs, buying cleaning agents, and food for inpatients had been reduced by the policy (Chama-Chiliba and Koch, 2016). The reimbursement rates of the new maternal policy in Laos PDR resulted in a marginal decrease in revenue for every delivery for their hospitals although it was predicted that a future increase in demand for delivery would increase revenue for the hospital (The World Bank, 2013). Equally, while Nepal’s policy reimbursed health facilities a higher amount for CS, there was no perverse incentive for the hospitals to choose CS over normal delivery (Ensor et al., 2017).
Health facilities in Ghana reported experiencing delayed reimbursement of funds meant for the free services and were thus faced with inadequate supplies and higher OOP for patients (Dalinjong et al., 2017). Equally, there was a disproportionate reimbursement to facilities based on regions and complexities of deliveries (Witter et al., 2007). Also, the difference in reimbursements was caused by some regions billing based on materials used rather than the government fixed rates, while others were structuring their reimbursement plans to cater for things like training of the TBAs (Witter et al., 2007). Facilities reported that they had lost incomes from petty sales to women (Witter et al., 2007). Despite the policy in Ethiopia, some facilities were requesting patients to pay for normal delivery or buy birth-related supplies, and others were performing emergency delivery only when there were advanced payments made (Luwei et al., 2011). In Nepal, facilities received adequate money to cover the cost of essential services and even had a surplus which they were using to incentivise their staff for excellent performance and improving the outlook of the hospitals (Witter et al., 2011).
Informal payments or tips
The review had mixed findings on informal payments from eight studies (Khan, 2005; Masiye et al., 2010; Bennis and De Brouwere, 2012; Boukhalfa et al., 2016; Lange et al., 2016; Vallières et al., 2016; Witter et al., 2016; Edu et al., 2017). Reasons commonly identified for a tip and informal payment were to get favours and preferential treatment (Witter et al., 2016), for performing routine activities such as pushing the patient’s trolley to and from the labour/operation room by security guards, and for HCWs to shave patients before delivery/surgery, give them enemas, and get favours such as having a bucket of hot water (Khan, 2005). In other cases, especially in hospitals that had scarce resources, patients tipped the HCWs to skip long waiting queues (Vallières et al., 2016). Other payments were either overtly or covertly asked from patients by HCWs without giving clear reasons (Lange et al., 2016). In other cases, it was not linked to the actual care (Bennis and De Brouwere, 2012; Boukhalfa et al., 2016), and in others, it existed in the form of under the table charges (Edu et al., 2017).
Survival tactics
Eight studies highlighted the survival tactics that families were adapting to meet the OOP (Nahar and Costello, 1998; Khan, 2005; Kruk et al., 2008; Bennis and De Brouwere, 2012; Witter et al., 2012; Arsenault et al., 2013; Witter et al., 2016; Dalinjong et al., 2017). Some of the methods included using savings (Witter et al., 2012; Witter et al., 2016; Dalinjong et al., 2017), seeking help from other family members (Nahar and Costello, 1998; Khan, 2005; Witter et al., 2016), handouts and loan from money lenders (Nahar and Costello, 1998; Khan, 2005; Bennis and De Brouwere, 2012; Witter et al., 2012), and selling both household and personal stuff such as carpets, chicken, jewellery (Nahar and Costello, 1998; Khan, 2005; Kruk et al., 2008; Bennis and De Brouwere, 2012; Dalinjong et al., 2017). Besides, some were selling livestock (Nahar and Costello, 1998; Khan, 2005; Dalinjong et al., 2017), others sold land, asked for an advance from employers, dug into their business capital, and sold rice or food (Nahar and Costello, 1998; Khan, 2005), or as is in Mali, sought support from the relatives living abroad and while the poor borrowed from friends and relatives (Kruk et al., 2008; Witter et al., 2012; Arsenault et al., 2013). In Tanzania, mothers decided to cut down on their spending (Kruk et al., 2008), while in Sudan, some families chose not to receive care at all, which was even more detrimental to their lives (Witter et al., 2012).
Equity concerns from FM policies
Eleven studies showed that despite the policies being free or were subsidised to mothers, there was a difference in the benefits received based on wealth categories (Khan, 2005; Asante et al., 2007; Witter et al., 2007; Ameur et al., 2012; Ridde et al., 2012a; Arsenault et al., 2013; The World Bank, 2013; Ganle et al., 2014; Philibert et al., 2014; Ganaba et al., 2016; Witter et al., 2016). The studies showed a difference in access to normal or emergency care (Ganaba et al., 2016), level of exemption, whether fully or partially (Ameur et al., 2012; Ridde et al., 2012a), selection of type of facility, whether private or public (Witter et al., 2016), and effects and amounts of OOPs on maternal care (Asante et al., 2007; Witter et al., 2007; Arsenault et al., 2013; The World Bank, 2013) based on wealth quantiles of the mothers. Families in rural areas in Bangladesh, for instance, had more difficulty paying the extra cost than urban households (Khan, 2005). Equally, the satisfaction level with provision of services differed based on wealth level with poor women being more satisfied (Philibert et al., 2014).
Overall expenditure of the policy and sustainability
Only four studies highlighted concepts of the overall expenditure of the policy (Witter et al., 2010; Witter et al., 2011; Ganaba et al., 2016; Witter et al., 2016). All the four studies showed that the funds allocated for the FM policies were adequately covering the cost of the essential services. Some of the policies were implemented in phases as a strategy of ensuring sustainability. Additionally, the policies reviewed were financed domestically and were potentially sustainable, mainly if they were implemented thoroughly (Witter et al., 2016).
Discussion
To the best of our understanding, this is first integrative review that has been done to analyse the effects of the FM policies on the quality and cost outcomes. The study reviewed the roles of FM policies on aspects of provision and experience of QoC following into the WHO standards for improving maternal and child health (World Health Organisation, 2016) and the cost aspects. Overall, the studies are heterogenic and uses mixed approaches to evaluate quality and costs of maternal care with all of them being in LICs and LMICs. The results have demonstrated that there are several forms of FM policies whose overall goal is to provide access to skilled birth attendance to the pregnant mothers.
There is adequate evidence to show that the policies have significantly played a role in improving the elements of provision of quality care. Our findings reveal that FM policies are associated with positive outcomes of evidence-based practices such as improved screening for key diseases such as syphilis and HIV in pregnancy, measuring vital statistics at ANC, reducing perinatal complications, and improving immunisation. The outcomes are in line with the achievement of SDG goals 3.1 and 3.2 (United Nations Development Programme, 2016; United Nations, 2017a), and previous studies have highlighted their importance (Villar et al., 2001; Lassi and Bhutta, 2015; Newman Owiredu et al., 2015; Singh et al., 2019a). Equally, the results show that there is very little evidence of FM policies implementing actionable information systems. While previous researchers have demonstrated that properly designed information system in maternal care could incentivise the measurement of quality care, provision of a central-based reporting tool that can potentially influence organisations’ performance and satisfaction with services (The Transforming Maternity Care Vision Team et al., 2010; Frøen et al., 2016; Koblinsky et al., 2016), it is still a gap within the FM policies that need to be strengthened. On the other hand, findings of this study suggest that majority of the FM policies have gaps in the referral system leading to poor quality outcomes. The referral systems seem to be influenced by the reimbursement strategies that are playing a role in altering the QoC especially where some hospitals may have been holding on to patients despite not being able to meet the needs. While a sound referral system is a prerequisite to proper management of complications and achievement of international quality standards, higher-level facilities may be burdened with complications and conditions that can be effectively managed at the lower level hospitals, which is a challenge of the FM policies (Akande, 2004). Studies have shown that efficient system should be one that moves patients up the referral ladders from a lower- to higher-level facilities after providing requisite care at the lower level (Kruk et al., 2018; Singh et al., 2019b, Daniels and Abuosi, 2020).
The experience of care by the women, who are the target of the FM policies, is significant. Our findings show that the women’s positive cumulative experience, while utilising the services under the FM policies, could encourage them to either return for subsequent delivery or impel them to seek care elsewhere. Due to the ripple effect created by good word of mouth based of good experience, others could be encouraged to seek care. FM policies are likely to successfully boost the women’s experience through excellent communication between HCWs and the mothers, which would eventually translate to the perception of respect, preservation of dignity, and feeling of sufficient emotional support (Hulton et al., 2000). However, communication and emotional support are a universal issue and not just related to FM policy. Several studies have shown a litany of factors that create positive maternal care experience. For example, interpersonal skills such as respect, courtesy, and dignity, attentiveness, rational qualities more than technical skills, decisiveness are some qualities that have been listed (Hulton et al., 2000; Hulton et al., 2007; Sharon Morad, 2013; Karkee et al., 2014; Machira and Palamuleni, 2018). Our findings show that increased utilisation and impracticable policy expectation that HCWs are faced with in FM policies are causing increased workload resulting to a breakdown of communication to the mothers leading to a perception of disrespect and abysmal emotional support. Some procedures or actions that mothers are subjected to during delivery take long to heal and may be difficult to undo (Hulton et al., 2000; Lange et al., 2016). Therefore, for a desirable experience of care, the mothers should understand the treatment action and feel that their concerns are adequately addressed (Hulton et al., 2000). From the policies, HCWs were perceived to be pushing women to unnecessary procedures which may have been due to asymmetry of information and a possibility that they wanted to reap the benefits of the reimbursements of the polices. Participative decision-making between patients and HCWs has been shown to build trust and preserve dignity (World Health Organisation, 2013; Zirak et al., 2017) hence can be implemented by the FM policies.
There are two elements: HCWs and essential resources, which are cross-cutting on provision and experience of care. Our results have shown that HCWs play a significant role; thus, their competence and motivations, although affected by several factors, allow for the provision of better routine care under the FM policies. The motivation of HCWs is multi-faceted and has been studied by several authors (Sato et al., 2017; Kok et al., 2018; Musinguzi et al., 2018). Our review highlighted that outcome of QoC could be altered by challenges such as include unequal distribution of staff in different regions, availability of requisite infrastructure, and incentives. Equally, the review showed that the supply of essential medication and equipment to hospitals, particularly after the implementation of FM policy, is a challenge and affects QoC. Many FM policies may be lacking critical inputs before implementation; thus, when faced with an increase in the number of users especially those who had not been previously targeted, could put pressure on available resources. Some designs of the FM policies may not be catering for replenishing strategies of the resources; therefore, a collusion cause or ripple effect may result from the increased number of patients leading to poor quality of service and dissatisfaction. Other studies have also shown similar trends (El-Khoury et al., 2011; Touré et al., 2012).
The review revealed that TBAs still play an essential role in society, and some women prefer them to midwives in hospitals despite FM policies. TBAs have the potential to alter the intended progress envisaged by most FM policies; hence, there is a need to involve them intelligently. Some of the TBAs are retired nurses and women prefer them because they provide better personal relationships and individualised attention during birth which many hospitals lack because of the increased number of deliveries because of the free policies. Other research has shown that some pregnant mothers perceive hospital staff and services poorly hence choose to deliver through the support of TBA (Oyerinde et al., 2013). While research has shown the mothers lack of resources is a contributor to TBA visits, the role of free policies should be to relieve the mothers of the payment burden.
Our review elucidated adequate evidence of the financial implications of the FM policies on patients, providers and managers, and facilities. While the goals of the policy are to improve access to skilled birth and protect mothers from financial catastrophe, the review has shown that the free policies have, in most cases, reduced family expenditure on healthcare; however, they have not eliminated OOP payment. OOP payments from patients worsened the equity gap and hindered access (Abel-Smith and Rawal, 1992; Wagstaff and Doorslaer, 2001; Ensor and Ronoh, 2005; Borghi et al., 2006; Parkhurst et al., 2006; Powell-Jackson et al., 2010). Due to lack of intelligent monitoring systems, there are informal payments that could be eliminated by developing systems that support financial transparency and professionalism among HCWs, besides reviewing incentives. Some of the strategies have been supported in informal payment research (Lewis, 2007; Kaitelidou et al., 2013; Baji et al., 2015; Baji et al., 2017). Also, there is a need for adequate consideration to be put to enhance sustainability of the policies especially in the design phase.
Avenues for future research
Several studies have used different designs to show the gaps in QoC and outcomes and changes in the cost accompanying FM policies but have not shown whether the policies are the cause. Therefore, we propose that mixed-method studies or econometrics studies with intervention and control groups could be used to fully attribute the policies to changes in quality and cost of care. Also, with the debate around UHC taking shape, more political economy studies could be conducted to evaluate potential factors and designs of FM policies that can maximise on the QoC, utilisation, and cost through effective coverage measure.
Limitations of the study
There are some limitations of the evidence from the review. For instance, our analysis was descriptive in nature, and alternate methods such as meta-analysis were not possible due to policy interventions, multiple outcomes, and the heterogeneity of studies. Also, we reviewed all studies without prior limitations of dates till 2018. There is a possibility that some studies related to our subject may have been published after 2018, but we wanted to focus on the period that captures best the discourse of initiation of UHC. Equally, some FM policies may have changed in design throughout the pilot periods or implementations, and we wanted to limit the heterogeneity.
Conclusion
There is a gap in quality care and outcomes of the FM policies that can adequately be reduced if the design of the policies actively invests in quality as significant objective rather than just enhancing utilisation. The policies can reduce the financial burden of the households if well implemented and sustainably funded. Besides, they may also contribute to the relative decline in inequity between the rich and poor though not independently. In order to achieve the SDG and UHC goals that seek to ensure that everyone who requires healthcare is able to access quality service without suffering catastrophic expenditure, our study proposes the following (Table 3).
Table 3.
Lessons for universal health coverage
| 1. HCWs should be at the centre of designing of the policies. Since their motivation is multifaceted, both intrinsic and extrinsic motivation factors could be included in the design phase of the policies. 2. Design of FM policies should incorporate a complimentary transport strategy that would reduce the overall OOP cost of delivery, particularly for the patients. 3. Properly equip the already existing hospitals and efficiently fund them to be able to provide quality and cost-efficient services. 4. Eliminate demeaning cultural practices, educate mothers, and improve access to quality care for all would eliminate socio-economic inequalities besides moving routine services nearer to potential users. 5. Have a better-targeted approach that would not only enhance fiscal sustainability but also reduce equity challenges. For free policies to achieve its intended objective, there was a need to improve supply-side readiness by increasing its management capacity. 6. Integrate the FM program into the public health system to enhance coverage and widen access; however, the operationalisation should have both the poor and the rich in mind aiming for equitable distribution. 7. To lessen the disparity in the delivery of FM services and eliminate inequalities, the policy designers should allocate resources based on need rather than on the size of the population. And the policy should push the benefit packages to the vulnerable population in the society especially the poor living in remote areas 8. Enhance awareness of the policy through a better communication channel to reach out better to the disadvantaged and more impoverished people especially within the rural communities 9. Implementation of a functional information system is imperative in integrating monitoring and evaluation system that will solve issues of referral and communication. 10. Provide professional development and education of HCWs to ensure their knowledge of the FM policy is up to date and their interpersonal skills are enhanced. |
Acknowledgements
The authors are grateful to Anna Peckham, who helped with the literature searches, access to database and development of MESH terms; Paul Ouma for GIS mapping; and Vanessa Abrahamson for reading through the draft manuscript.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S1463423621000529.
click here to view supplementary material
Financial support
The Commonwealth Scholarship Commission supports BO’s PhD study.
Conflict of interests
The authors declare that they had no competing interests.
Authors’ contribution
BO was involved in the conception and design, data extraction, data synthesis, data analysis, and drafted the manuscript and participated in its revision. SK supervised the work of BO and participated in drafting this manuscript. SP reviewed the manuscript and contributed to the revision.
Ethical approvals
The study is part of a PhD work at the Centre for Health Services Studies conducted by the first author. Ethical approval for the overall study was provided by School of Social Policy Sociology and Social Research Student Research Ethics Committee and AMREF Health Africa Ethics and Scientific Review Committee (REF: AMREF – ESRC P537/2018).
Availability of data and material
All data sets used and or analysed during the study are available from the corresponding author on a reasonable request.
References
- Abel-Smith B and Rawal P (1992) Can the poor afford ‘free’ health services? A case study of Tanzania. Health Policy and Planning 7, 329–341. [Google Scholar]
- Akande T (2004) Referral system in Nigeria: study of a tertiary health facility. Annals of African Medicine 3, 130–133. [Google Scholar]
- Ameur AB, Ridde V, Bado AR, Ingabire MG and Queuille L (2012) User fee exemptions and excessive household spending for normal delivery in Burkina Faso: the need for careful implementation. BMC Health Services Research 12, 412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amu NJ (2005) The role of women in Ghana’s economy. Accra, Ghana: Friedrich Ebert Stiftung. [Google Scholar]
- Arsenault C, Fournier P, Philibert A, Sissoko K, Coulibaly A, Tourigny C, Traore M and Dumont A (2013) Emergency obstetric care in Mali: catastrophic spending and its impoverishing effects on households. Bulletin of the World Health Organization 91, 207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asante FA, Chikwama C, Daniels A and Armar-Klemesu M (2007) Evaluating the economic outcomes of the policy of fee exemption for maternal delivery care in Ghana. Ghana Medical Journal 41, 110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baji P, Pavlova M, Gulácsi L and Groot W (2015) Does the implementation of official user charges help to eradicate informal payments – lessons to be learnt from the Hungarian experience. Frontiers in Public Health 3, 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baji P, Rubashkin N, Szebik I, Stoll K and Vedam S (2017) Informal cash payments for birth in Hungary: are women paying to secure a known provider, respect, or quality of care? Social Science & Medicine 189, 86–95. [DOI] [PubMed] [Google Scholar]
- Bennis I and De Brouwere V (2012) Fee exemption for caesarean section in Morocco. Archives of Public Health 70, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borghi J, Ensor T, Neupane BD and Tiwari S (2006) Financial implications of skilled attendance at delivery in Nepal. Tropical Medicine & International Health 11, 228–237. [DOI] [PubMed] [Google Scholar]
- Bosu WK, Bell J, Armar-Klemesu M and Tornui J (2007) Effect of delivery care user fee exemption policy on institutional maternal deaths in the Central and Volta Regions of Ghana. Ghana Medical Journal 41, 118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boukhalfa C, Abouchadi S, Cunden N and Witter S (2016) The free delivery and caesarean policy in Morocco: how much do households still pay? Tropical Medicine and International Health 21, 245–252. [DOI] [PubMed] [Google Scholar]
- Carrera JM (2007) Maternal mortality in Africa. Journal of Perinatal Medicine 35, 266–277. [DOI] [PubMed] [Google Scholar]
- Chama-Chiliba CM and Koch SF (2014) Assessing regional variations in the effect of the removal of user fees on institutional deliveries in rural Zambia [Online]. University of Pretoria. Retrieved from https://www.up.ac.za/media/shared/61/working_papers/wp_2014_17.pdf [Accessed 21 August 2018]. [Google Scholar]
- Chama-Chiliba CM and Koch SF (2016) An assessment of the effect of user fee policy reform on facility-based deliveries in rural Zambia. BMC Research Notes 9, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chankham T, Yamamoto E, Reyer JA, Arafat R, Innoukham K, Panome S, Hongkham D, Bounfeng P, Anonh X and Hamajima N (2017) Knowledge of free delivery policy among women who delivered at health facilities in Oudomxay Province, Lao PDR. Nagoya Journal of Medical Science 79, 135–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christmals CD and Gross JJ (2017) An Integrative literature review framework for post graduate nursing research reviews. European Journal of Research in Medical Sciences 5, 7–15. [Google Scholar]
- Critical Appraisal Skills Programme (2017. a) CASP case control study checklist [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_afbfc99848f64537a53826e1f5b30b5c.pdf [Accessed 24 October 2017]. [Google Scholar]
- Critical Appraisal Skills Programme (2017. b) CASP clinical prediction rule checklist [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_a2f74f6cd2f24bd684bb26efe7ad7196.pdf [Accessed 24 October 2017]. [Google Scholar]
- Critical Appraisal Skills Programme (2017. c) CASP cohort study checklist [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_5ad0ece77a3f4fc9bcd3665a7d1fa91f.pdf [Accessed 24 October 2017]. [Google Scholar]
- Critical Appraisal Skills Programme (2017. d) CASP diagnostic test study [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_5f100f2d207a462a8dd552bfb6090d60.pdf [Accessed 24 October 2017]. [Google Scholar]
- Critical Appraisal Skills Programme (2017. e) CASP economic evaluation checklist [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_861b48c94b654b82a84250ca684d9186.pdf [Accessed 24 October 2017]. [Google Scholar]
- Critical Appraisal Skills Programme (2017. f) CASP qualitative research checklist [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_25658615020e427da194a325e7773d42.pdf [Accessed 24 October 2017]. [Google Scholar]
- Critical Appraisal Skills Programme (2017. g) CASP randomised controlled trial checklist [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_4239299b39f647ca9961f30510f52920.pdf [Accessed 24 October 2017]. [Google Scholar]
- Critical Appraisal Skills Programme (2017. h) CASP systematic review checklist [Online]. Critical Appraisal Skills Programme. Retrieved from http://docs.wixstatic.com/ugd/dded87_7e983a320087439e94533f4697aa109c.pdf [Accessed 24 October 2017]. [Google Scholar]
- Dalinjong PA, Wang AY and Homer CSE (2017) The operations of the free maternal care policy and out-of-pocket payments during childbirth in rural Northern Ghana. Health Economics Review 7, 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels AA and Abuosi A (2020) Improving emergency obstetric referral systems in low and middle income countries: a qualitative study in a tertiary health facility in Ghana. BMC Health Services Research 20, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delamou A, Dubourg D, Beavogui AH, Delvaux T, Kolie JS, Barry TH, Camara BS, Edginton M, Hinderaker S and De Brouwere V (2015) How has the free obstetric care policy impacted unmet obstetric need in a rural health district in Guinea? PLoS One 10, e0129162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A (1988) The quality of care: how can it be assessed? The Journal of the American Medical Association 260, 1743–1748. [DOI] [PubMed] [Google Scholar]
- Donabedian A (1990) The seven pillars of quality. Archives of Pathology and Laboratory Medicine 114, 1115–1118. [PubMed] [Google Scholar]
- Dossou JP, Cresswell JA, Makoutodé P, De Brouwere V, Witter S, Filippi V, Kanhonou LG, Goufodji SB, Lange IL, Lawin L, Affo F and Marchal B (2018) ‘Rowing against the current’: the policy process and effects of removing user fees for caesarean sections in Benin. BMJ Global Health 3, e000537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edu BC, Agan TU, Monjok E and Makowiecka K (2017) Effect of free maternal health care program on health-seeking behavior of women during pregnancy, intra-partum and postpartum periods in Cross River State of Nigeria: a mixed method study. Open Access Macedonian Journal of Medical Sciences 5, 370–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekman B (2007) Catastrophic health payments and health insurance: some counterintuitive evidence from one low-income country. Health Policy 83, 304–313. [DOI] [PubMed] [Google Scholar]
- El-Khoury M, Gandaho T, Arur A, Keita B and Nichols L (2011) Improving access to life saving maternal health services: the effects of removing user fees for caesareans in Mali. Bethesda: Health Systems 20, 20. [Google Scholar]
- Ensor T, Bhatt H and Tiwari S (2017) Incentivizing universal safe delivery in Nepal: 10 years of experience. Health Policy and Planning 32, 1185–1192. [DOI] [PubMed] [Google Scholar]
- Ensor T and Ronoh J (2005) Effective financing of maternal health services: a review of the literature. Health Policy 75, 49–58. [DOI] [PubMed] [Google Scholar]
- Frøen JF, Myhre SL, Frost MJ, Chou D, Mehl G, Say L, Cheng S, Fjeldheim I, Friberg IK and French S (2016) eRegistries: Electronic registries for maternal and child health. BMC Pregnancy and Childbirth 16, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrysch S and Campbell OM (2009) Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth 9, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganaba R, Ilboudo PGC, Cresswell JA, Yaogo M, Diallo CO, Richard F, Cunden N, Filippi V and Witter S (2016) The obstetric care subsidy policy in Burkina Faso: what are the effects after five years of implementation? Findings of a complex evaluation. BMC Pregnancy and Childbirth 16, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganle JK, Parker M, Fitzpatrick R and Otupiri E (2014) A qualitative study of health system barriers to accessibility and utilization of maternal and newborn healthcare services in Ghana after user-fee abolition. BMC Pregnancy and Childbirth 14, 434–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, Lopez AD, Lozano R and Murray CJ (2010) Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. The Lancet 375, 1609–1623. [DOI] [PubMed] [Google Scholar]
- Hulton L, Matthews Z and Stones RW (2000) A framework for the evaluation of quality of care in maternity services. Highfield, Southamton: University of Southamton. [Google Scholar]
- Hulton LA, Matthews Z and Stones RW (2007) Applying a framework for assessing the quality of maternal health services in urban India. Social Science & Medicine 64, 2083–2095. [DOI] [PubMed] [Google Scholar]
- Kaitelidou DC, Tsirona CS, Galanis PA, Siskou OC, Mladovsky P, Kouli EG, Prezerakos PE, Theodorou M, Sourtzi PA and Liaropoulos LL (2013) Informal payments for maternity health services in public hospitals in Greece. Health Policy 109, 23–30. [DOI] [PubMed] [Google Scholar]
- Karkee R, Lee A and Pokharel PK (2014) Women’s perception of quality of maternity services: a longitudinal survey in Nepal. BMC Pregnancy & Childbirth, 14, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley E and Hurst J (2006) Health care quality indicators project: conceptual framework paper [Online]. Organisation for Economic Co-operation and Development. Retrieved from http://thuvien.thanglong.edu.vn:8081/dspace/bitstream/DHTL_123456789/3992/1/No.%2023%20Healthcare%20quality%20indicators%20project%20%E2%80%93%20Conceptual%20framework%20paper.pdf [Accessed 13th May 2018]. [Google Scholar]
- Kenya Ministry of Health (2015) Status of implementation of free maternity services in the devolved health systems in Kenya [Online]. Nairobi: Kenya Ministry of Health. Retrieved from http://publications.universalhealth2030.org/uploads/free_maternal_health_services_report_feb_2015_final1_doc_.pdf [Accessed 25 May 2020]. [Google Scholar]
- Khan SH (2005) Free does not mean affordable: maternity patient expenditures in a public hospital in Bangladesh. Cost Effectiveness and Resource Allocation 3, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblinsky M, Moyer CA, Calvert C, Campbell J, Campbell OMR, Feigl AB, Graham WJ, Hatt L, Hodgins S, Matthews Z, McDougall L, Moran AC, Nandakumar AK and Langer A (2016) Quality maternity care for every woman, everywhere: a call to action. The Lancet 388, 2307–2320. [DOI] [PubMed] [Google Scholar]
- Kok MC, Vallières F, Tulloch O, Kumar MB, Kea AZ, Karuga R, Ndima SD, Chikaphupha K, Theobald S and Taegtmeyer M (2018) Does supportive supervision enhance community health worker motivation? A mixed-methods study in four African countries. Health Policy and Planning 33, 988–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koroma MM, Kamara SS, Bangura EA, Kamara MA, Lokossou V and Keita N (2017) The quality of free antenatal and delivery services in Northern Sierra Leone. Health Research Policy and Systems 15, 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-Dewan S, Adeyi O, Barker P, Daelmans B and Doubova SV (2018) High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health 6, e1196–e1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk ME, Mbaruku G, Rockers PC and Galea S (2008) User fee exemptions are not enough: out-of-pocket payments for ‘free’ delivery services in rural Tanzania. Tropical Medicine and International Health 13, 1442–1451. [DOI] [PubMed] [Google Scholar]
- Lagarde M, Barroy H and Palmer N (2012). Assessing the effects of removing user fees in Zambia and Niger. Journal of Health Services Research & Policy 17, 30–36. [DOI] [PubMed] [Google Scholar]
- Lange IL, Kanhonou L, Goufodji S, Ronsmans C and Filippi V (2016) The costs of ‘free’: experiences of facility-based childbirth after Benin’s caesarean section exemption policy. Social Science & Medicine 168, 53–62. [DOI] [PubMed] [Google Scholar]
- Lassi ZS and Bhutta ZA (2015) Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database of Systematic Reviews. 11, CD007754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis M (2007) Informal payments and the financing of health care in developing and transition countries. Health Affairs 26, 984–997. [DOI] [PubMed] [Google Scholar]
- Li Y, Wu Q, Xu L, Legge D, Hao Y, Gao L, Ning N and Wan G (2012) Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance. Bulletin of the World Health Organization 90, 664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightman ES and Lightman N (2017) Social policy in Canada. Canada, Toronto: Oxford University Press. [Google Scholar]
- Luwei P, Gandhi M, Admasu K and Keyes EB (2011) User fees and maternity services in Ethiopia. International Journal of Gynecology and Obstetrics 115, 310–315. [DOI] [PubMed] [Google Scholar]
- Machira K and Palamuleni M (2018) Women’s perspectives on quality of maternal health care services in Malawi. International Journal of Women’s Health 10, 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masiye F, Chitah BM, Chanda P and Simeo F (2008) Removal of user fees at primary health care facilities in Zambia: a study of the effects on utilisation and quality of care. Regional Network for Equity in Health in East and Southern Africa Discussion Paper (ed.) EQUINET Discussion Paper Series 57. Harare: EQUINET, UCT HEU. [Google Scholar]
- Masiye F, Chitah BM and McIntyre D (2010) From targeted exemptions to user fee abolition in health care: experience from rural Zambia. Social Science & Medicine 71, 743–750. [DOI] [PubMed] [Google Scholar]
- Mekonnen Y and Mekonnen A (2003) Factors influencing the use of maternal healthcare services in Ethiopia. Journal of Health, Population, and Nutrition 21, 374–382. [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P and Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (Prisma-P) 2015 statement. Systematic Reviews 4, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musinguzi C, Namale L, Rutebemberwa E, Dahal A, Nahirya-Ntege P and Kekitiinwa A (2018) The relationship between leadership style and health worker motivation, job satisfaction and teamwork in Uganda. Journal of Healthcare Leadership 10, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabyonga-Orem J, Karamagi H, Atuyambe L, Bagenda F, Okuonzi SA and Walker O (2008) Maintaining quality of health services after abolition of user fees: a Uganda case study. BMC Health Services Research 8, 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahar S and Costello A (1998) The hidden cost of ‘free’maternity care in Dhaka, Bangladesh. Health Policy and Planning 13, 417–422. [DOI] [PubMed] [Google Scholar]
- Newman Owiredu M, Newman L, Nzomo T, Conombo Kafando G, Sanni S, Shaffer N, Bucagu M, Peeling R, Mark J and Diop Toure I (2015) Elimination of mother-to-child transmission of HIV and syphilis: a dual approach in the African Region to improve quality of antenatal care and integrated disease control. International Journal of Gynecology & Obstetrics 130, S27–S31. [DOI] [PubMed] [Google Scholar]
- Nimpagaritse M and Bertone MP (2011) The sudden removal of user fees: the perspective of a frontline manager in Burundi. Health Policy and Planning 26, ii63–ii71. [DOI] [PubMed] [Google Scholar]
- Oyeneyin LO, Akintan AL, Aderoba AK and Owa OO (2017) Maternal mortality ratio in a tertiary hospital offering free maternity services in South-western Nigeria–a five-year review. Tropical Journal of Obstetrics and Gynaecology 34, 112. [Google Scholar]
- Oyerinde K, Harding Y, Amara P, Garbrah-Aidoo N, Kanu R, Oulare M, Shoo R and Daoh K (2013) A qualitative evaluation of the choice of traditional birth attendants for maternity care in 2008 Sierra Leone: implications for universal skilled attendance at delivery. Maternal and Child Health Journal 17, 862–868. [DOI] [PubMed] [Google Scholar]
- Parkhurst JO, Rahman SA and Ssengooba F (2006) Overcoming access barriers for facility-based delivery in low-income settings: insights from Bangladesh and Uganda. Journal of Health, Population, and Nutrition 24, 438. [PMC free article] [PubMed] [Google Scholar]
- Philibert A, Ridde V, Bado A and Fournier P (2014) No effect of user fee exemption on perceived quality of delivery care in Burkina Faso: a case-control study. BMC Health Services Research 14, 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell-Jackson T, Tiwari S, Neupane B and Singh M (2010) An early evaluation of the Aama free delivery care programme. Kathmandu: Support to the Safe Motherhood Programme (SSMP)). [Google Scholar]
- Ravit M, Philibert A, Tourigny C, Traore M, Coulibaly A, Dumont A and Fournier P (2015) The hidden costs of a free caesarean section policy in West Africa (Kayes Region, Mali). Maternal and Child Health Journal 19, 1734–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridde V (2003) Fees-for-services, cost recovery, and equity in a district of Burkina Faso operating the Bamako Initiative. Bulletin of the World Health Organization 81, 532–538. [PMC free article] [PubMed] [Google Scholar]
- Ridde V, Agier I, Jahn A, Mueller O, Tiendrebeogo J, Ye M and De Allegri M (2015) The impact of user fee removal policies on household out-of-pocket spending: evidence against the inverse equity hypothesis from a population based study in Burkina Faso. The European Journal of Health Economics 16, 55–64. [DOI] [PubMed] [Google Scholar]
- Ridde V and Diarra A (2009) A process evaluation of user fees abolition for pregnant women and children under five years in two districts in Niger (West Africa). BMC Health Services Research 9, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridde V, Kouanda S, Bado A, Bado N and Haddad S (2012. a) Reducing the medical cost of deliveries in Burkina Faso is good for everyone, including the poor. PLoS One 7, e33082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridde V, Kouanda S, Yameogo M, Kadio K and Bado A (2013) Why do women pay more than they should? a mixed methods study of the implementation gap in a policy to subsidize the costs of deliveries in Burkina Faso. Evaluation and Program Planning 36, 145–152. [DOI] [PubMed] [Google Scholar]
- Ridde V and Morestin F (2010) A scoping review of the literature on the abolition of user fees in health care services in Africa. Health Policy and Planning 26, 1–11. [DOI] [PubMed] [Google Scholar]
- Ridde V, Queuille L, Kafando Y and Robert E (2012. b) Transversal analysis of public policies on user fees exemptions in six West African countries. BMC Health Services Research 12, 409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridde V, Robert E and Meessen B (2012. c) A literature review of the disruptive effects of user fee exemption policies on health systems. BMC Public Health 12, 289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa F, Bagnasco A, Aleo G, Kendall S and Sasso L (2017) Resilience as a concept for understanding family caregiving of adults with Chronic Obstructive Pulmonary Disease (COPD): an integrative review. Nursing Open 4, 61–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato M, Maufi D, Mwingira UJ, Leshabari MT, Ohnishi M and Honda S (2017) Measuring three aspects of motivation among health workers at primary level health facilities in rural Tanzania. PloS One 12, e0176973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharon Morad B (2013) Dignity in maternity care. Evidence Based Midwifery 11, 67. [Google Scholar]
- Sidze EM, Fenenga C, Amendah DD, Maina TM, Mutua MK, Mulupi SK, Van Der List M and Elbers C (2015) Are free maternal healthcare services programs an impediment to quality care? An examination of the Kenyan experience. African Population and Health Research Center 5, 1–10. [Google Scholar]
- Singh S, Doyle P, Campbell OM and Murthy G (2019. b) Management and referral for high-risk conditions and complications during the antenatal period: knowledge, practice and attitude survey of providers in rural public healthcare in two states of India. Reproductive Health 16, 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh L, Dubey R, Singh S, Goel R, Nair S and Singh P (2019. a) Measuring quality of antenatal care: a secondary analysis of national survey data from India. BJOG: An International Journal of Obstetrics & Gynaecology 126, 7–13. [DOI] [PubMed] [Google Scholar]
- Stanton ME, Higgs ES and Koblinsky M (2013) Investigating financial incentives for maternal health: an introduction. Journal of Health, Population, and Nutrition 31, S1. [PubMed] [Google Scholar]
- Steinhardt LC, Aman I, Pakzad I, Kumar B, Singh LP and Peters DH (2011) Removing user fees for basic health services: a pilot study and national roll-out in Afghanistan. Health Policy and Planning 26, ii92–ii103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Transforming Maternity Care Vision Team, Carter MC, Corry M, Delbanco S, Foster TCS, Friedland R, Gabel R, Gipson T, Jolivet RR and Main E (2010) 2020 vision for a high-quality, high-value maternity care system. Women’s Health Issues 20, S7–S17. [DOI] [PubMed] [Google Scholar]
- The World Bank (2013) Maternal health out-of-pocket expenditure and service readiness in Lao PDR : evidence for the national free maternal and child health policy from a household and health center survey. Washington, DC: World Bank. [Google Scholar]
- Torraco RJ (2005) Writing integrative literature reviews: guidelines and examples. Human Resource Development Review 4, 356–367. [Google Scholar]
- Touré L, Fofana S, Koné S and Sanogo Y (2012) La mise en œuvre de la politique de gratuité de la césarienne. Étude comparative dans 3 sites d’enquête, L’abolition du paiement des services de santé en Afrique de l’Ouest (Burkina Faso, Mali, Niger). Miseli-Mali.
- United Nations (2017. a) The sustainable development goals report 2017 [Online]. New York: United Nations. Retrieved from https://unstats.un.org/sdgs/files/report/2017/TheSustainableDevelopmentGoalsReport2017.pdf [Accessed 17 October 2017]. [Google Scholar]
- United Nations (2017. b) Sustainable development goals: 17 goals that transform our world [Online]. New York: United Nations. Retrieved form http://www.un.org/sustainabledevelopment/health/ [Accessed 17 October 2017]. [Google Scholar]
- United Nations Development Programme (2016) Sustainable development goals. Geneva: UNDP. [Google Scholar]
- Vallières F, Cassidy EL, McAuliffe E, Gilmore B, Bangura AS and Musa J (2016) Can Sierra Leone maintain the equitable delivery of their Free Health Care Initiative? The case for more contextualised interventions: results of a cross-sectional survey. BMC Health Services Research 16, 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doorslaer E, O’donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, Harbianto D, Herrin AN, Huq MN and Ibragimova S (2006) Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. The Lancet 368, 1357–1364. [DOI] [PubMed] [Google Scholar]
- Villar J, Ba’aqeel H, Piaggio G, Lumbiganon P, Belizán JM, Farnot U, Al-Mazrou Y, Carroli G, Pinol A and Donner A (2001) WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. The Lancet 357, 1551–1564. [DOI] [PubMed] [Google Scholar]
- Wagstaff A and Van Doorslaer EK (2001) Paying for health care: quantifying fairness, catastrophe, and impoverishment, with applications to Vietnam, 1993–98. Washington, DC: The World Bank. [DOI] [PubMed] [Google Scholar]
- Wechkunanukul K, Grantham H and Clark RA (2017) Global review of delay time in seeking medical care for chest pain: an integrative literature review. Australian Critical Care 30, 13–20. [DOI] [PubMed] [Google Scholar]
- Whittemore R and Knafl K (2005) The integrative review: updated methodology. Journal of Advanced Nursing 52, 546–553. [DOI] [PubMed] [Google Scholar]
- Witter S (2010) Mapping user fees for health care in high-mortality countries–evidence from a recent survey. [Online]. London: HLSP Institute. Available: https://eresearch.qmu.ac.uk/bitstream/handle/20.500.12289/3026/Witter.pdf?sequence=1 [Accessed 19 February 2018]. [Google Scholar]
- Witter S, Arhinful DK, Kusi A and Zakariah-Akoto S (2007) The experience of Ghana in implementing a user fee exemption policy to provide free delivery care. Reproductive Health Matters 15, 61–71. [DOI] [PubMed] [Google Scholar]
- Witter S, Boukhalfa C, Cresswell JA., Daou Z, Filippi V, Ganaba R, Goufodji S, Lange IL, Marchal B, Richard F and Team FE (2016) Cost and impact of policies to remove and reduce fees for obstetric care in Benin, Burkina Faso, Mali and Morocco. International Journal for Equity in Health 15, 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witter S, Dieng T, Mbengue D, Moreira I and De Brouwere V (2010) The national free delivery and caesarean policy in Senegal: evaluating process and outcomes. Health Policy and Planning 25, 384–392. [DOI] [PubMed] [Google Scholar]
- Witter S, Garshong B and Ridde V (2013) An exploratory study of the policy process and early implementation of the free NHIS coverage for pregnant women in Ghana. International Journal for Equity in Health 12, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witter S, Ilboudo PG, Cunden N, Boukhalfa C, Makoutode P and Daou Z (2017) Delivery fee exemption and subsidy policies: how have they affected health staff? findings from a four-country evaluation. Health Policy and Planning 32, 236–247. [DOI] [PubMed] [Google Scholar]
- Witter S, Khadka S, Nath H and Tiwari S (2011) The national free delivery policy in Nepal: early evidence of Its effects on health facilities. Health Policy and Planning 26, ii84–ii91. [DOI] [PubMed] [Google Scholar]
- Witter S, Khalid Mousa K, Abdel-Rahman ME, Hussein Al-Amin R and Saed M (2012) Removal of user fees for caesareans and under-fives in northern Sudan: a review of policy implementation and effectiveness. International Journal of Health Planning and Management 28, e95–e120. [DOI] [PubMed] [Google Scholar]
- World Health Organisation (2013) Exploring patient participation in reducing health-care-related safety risks. Copenhagen, Denmark: World Health Organisation Regional Office for Europe. [Google Scholar]
- World Health Organisation (2016) Standards for improving quality of maternal and newborn care in health facilities [Online]. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World Health Organisation. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/249155/9789241511216-per.pdf [Accessed 8th March 2019]. [Google Scholar]
- World Health Organisation (2019) Trends in maternal mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization. [Google Scholar]
- Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P and Evans T (2007) Protecting households from catastrophic health spending. Health Affairs 26, 972–983. [DOI] [PubMed] [Google Scholar]
- Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J and Murray CJ (2003) Household catastrophic health expenditure: a multicountry analysis. The Lancet 362, 111–117. [DOI] [PubMed] [Google Scholar]
- Yorks L (2008) What we know, what we don’t know, what we need to know—integrative literature reviews are research. Los Angeles, CA: SAGE Publications. [Google Scholar]
- Zirak M, Ghafourifard M and Mamaghani EA (2017) Patients’ dignity and its relationship with contextual variables: a cross-sectional study. Journal of Caring Sciences 6, 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S1463423621000529.
click here to view supplementary material