Abstract
Background
Neonatal mortality is a major global public health problem. Ethiopia is among seven countries that comprise 50 % of global neonatal mortality. Evidence on neonatal mortality in referred neonates is essential for intervention however, there is no enough information in the study area. Neonates who required referral frequently became unstable and were at a high risk of death. Therefore, this study aimed to assess the incidence and predictors of mortality among referred neonates.
Method
A prospective follow-up study was conducted among 436 referred neonates at comprehensive specialized hospitals in the Amhara regional state, North Ethiopia 2020. All neonates admitted to the selected hospitals that fulfilled the inclusion criteria were included. Face-to-face interviews, observations, and document reviews were used to collect data using a semi-structured questionnaire and checklists. Epi-data™ version 4.2 software for data entry and STATA™ 14 version for data cleaning and analysis were used. Variables with a p-value < 0.25 in the bi-variable logistic regression model were selected for multivariable analysis. Multivariable analyses with a 95% confidence level were performed. Variables with P < 0.05 were considered statistically significant.
Result
Over all incidence of death in this study was 30.6% with 95% confidence interval of (26.34–35.16) per 2 months observation. About 23 (17.83%) deaths were due to sepsis, 32 (24.80%) premature, 40 (31%) perinatal asphyxia, 3(2.33%) congenital malformation and 31(24.03%) deaths were due to other causes. Home delivery [AOR = 2.5, 95% CI (1.63–4.1)], admission weight < 1500 g [AOR =3.2, 95% CI (1.68–6.09)], travel distance ≥120 min [AOR = 3.8, 95% CI (1.65–9.14)], hypothermia [AOR = 2.7, 95% CI (1.44–5.13)], hypoglycemia [AOR = 1.8, 95% CI (1.11–3.00)], oxygen saturation < 90% [AOR = 1.9, 95% (1.34–3.53)] at admission time and neonate age ≤ 1 day at admission [AOR = 3.4, 95% CI (1.23–9.84) were predictors of neonatal death.
Conclusion
The incidence of death was high in this study. The acute complications arising during the transfer of referral neonates lead to an increased risk of deterioration of the newborn’s health and outcome. Preventing and managing complications during the transportation process is recommended to increase the survival of neonates.
Keywords: Referred neonate, Transportation, Referral, Predicting factors
Introduction
Neonatal mortality is the total number of children who died between birth and the 28th day of life. It consists of early neonatal mortality for deaths in the first week and late neonatal mortality for deaths in the following 3 weeks [1, 2]. On average 2.5 million newborns die within 28 days of life and account for 47% of the under 5 mortality in 2018. More than 99% of deaths occurred in developing countries. Sub-Saharan Africa carries more than 52% of neonatal mortality. Ethiopia is among the seven countries comprising 50% of the global neonatal mortality [3].
Global efforts that are currently underway have been declining neonatal mortality to 19 deaths per 1000 live births in 2015 to 18 deaths per 1000 live births in 2018. However, neonatal mortality remains unacceptably high in many low- and middle-income countries. The neonatal mortality rate in developing countries is more than eight times that in developed countries. In Sub-Saharan African countries neonatal death occurred in 28 deaths per 1000 live births. In Ethiopia according to the mini EDHS 2019, neonatal mortality in Ethiopia was 30 death/1000 live births [3, 4].
Worldwide, preterm birth complications, intrapartum birth complications and sepsis are the leading causes of neonatal death [5]. In Ethiopia, the top causes of neonatal death are asphyxia, complications related to prematurity and neonatal sepsis [4, 6]. Neonatal mortality related to instability or complications secondary to referral is another challenge and a worldwide health problem [7]. The severity of the problem varies from developed to developing countries [8].
The Ethiopian federal ministry of health planned to achieve neonatal mortality of < 12 deaths /1000 live births with a commitment to end preventable child death by 2030. Integrated management of neonatal and childhood illness (IMNCI), community-based nutrition (CBN), community-based newborn care (CBNC), increasing access and quality of primary health care services, early antenatal care and interventions such as referral of high-risk and sick babies to higher equipped facilities, increases in vaccination, skilled birth attendance and option B+ for PMTCT are among the strategies implemented by the government of Ethiopia. However, neonatal mortality still continues increase from 29 to 30 deaths per 1000 live births between 2016 and 2019 and varies across regions. According to research finding neonatal mortality in the Amhara regional state is 20.3% [4, 9–11].
In addition to major causes of neonatal death, some evidence in different parts of the world indicates acute physiologic complications like hypothermia, hypoglycemia, poor peripheral perfusion and other complications related to poor neonatal transport was another challenge for survival and good outcomes of referral neonates. The death occurred about 21.2–79.1% in hypothermic and 60–75.29% in poor peripheral perfusion neonates at admission [12, 13]. The incidence of death and hypoglycemia from referred neonates with oxygen saturation < 90% at admission was 60 and 14.6% respectively. The mortality risk of clinically unstable neonates at admission time was 5 times higher than those referred in a stable condition [14–16].
In resource-limited countries referral systems is not well established and referral neonates travel long distances without emergency care, resuscitation equipment and adequately trained personnel to get access to specialty care [17–19]. Many studies have shown that long-distance travel without emergency care and inadequate continuity of care during transfer, sociodemographic factors, neonatal and maternal factors and health-related factors affect the health of neonates [20–23]. Data on the incidence and predictive factors associated with mortality among referred neonates are a crucial and timely issues. Therefore, this study aimed to assess the incidence and predictors of neonatal mortality among referred neonates admitted to comprehensive and specialized hospitals in Amhara regional state, North Ethiopia 2020.
Method and materials
Study setting and design
A prospective follow-up study was conducted from October 1 to November 30, 2020, in neonatal intensive care units of comprehensive specialized and specialized hospitals in the Amhara regional state including Debre Markos and Felege Hiwot comprehensive specialized hospitals and Tibebe Ghion and Gonder specialized hospitals. Felege Hiwot and Tibebe Ghion hospital are found in Bahi Dar (the capital city of Amhara regional state) 565 km far from Addis Ababa. Debre Markos and Gonder hospitals are found to be 299 and 730 km respectively far from Addis Ababa. These Hospitals are final referral choices for other health institutions around that provide tertiary level neonatal care. Hospitals have neonatal intensive care units with 158 neonatal beds organized with necessary materials and equipment and mixed health professionals (neonatal and general nurse, general practitioners, pediatricians, and other staff). The major services include general neonatal care services, blood and exchange transfusion, phototherapy, and ventilation support such as continuous positive air pressure (CPAP).
Hospitals had an average of 454 two-months neonatal admissions referred from other health institutions around hospitals: Debre Markos, Felege Hiwot, Tibebe Ghion, and Gonder comprehensive specialized hospitals have an average of 86, 121, 106, and 141 referrals neonatal admission respectively. The Amhara regional state has only six comprehensive and two specialized hospitals in 2020. These hospitals may have many referred neonates. Geographically hospitals are far from many primary and secondary health centers and take a long time to transport referred neonates from catchment areas. That is why this setting was chosen as the study area.
Populations
All neonates referred to the comprehensive and specialized hospitals in the Amhara regional state from other health institutions in 2020 were the source population.
All referred neonates who were referred and transferred to study areas of hospitals and admitted in the neonatal intensive and emergency care units during the study period were taken as the study population.
Eligibility criteria
All inter referral neonates from other health facilities and admitted to the neonatal intensive and emergency care units were included.
All self-referral neonates who came by their preference without health professional decisions and all neonates readmitted after discharge with improvement were excluded.
Sample size determination
The Sample size was determined by the Fleiss formula using Epi Info7.2.1 by considering significant predicting variables from related works of literature (Table 1). Thus, sample size calculation was based on the following assumptions (Two-sided confidence level = 95%, power = 80% and ratio of exposure to non-exposure = 1:1) and from a prospective follow up study conducted on predictors of mortality in referred neonates with neonatal sepsis at a tertiary care center Maharashtra, India the proportion of neonatal death from hypothermic as exposed and non-hypothermic as non-exposed and odds ratio with non-response rate 10% [12].
Table 1.
sample size calculation to assess the incidence and predictors of neonatal mortality among referred neonates admitted to Comprehensive Specialized Hospitals in Amhara Regional State North, Ethiopia, 2020
| Significant factors associated with neonatal mortality | Proportion among exposure and non-exposure | Total sample size | Source |
|---|---|---|---|
| Capillary refill time: | |||
| > 3 s | P1 = 0.45 | 238 | (16) |
| < 3 s | q1 = 0.26 | ||
| Body temperature at admission time: | |||
| Hypothermic | P1 = 0.43 | 396 | |
| Non-hypothermic | q1 = 0.29 | ||
| Delivery conducted: | |||
| Unskilled birth attendant | P1 = 0.73 | 42 | (48) |
| Skilled birth attendants | q1 = 0.26 | ||
| Oxygen saturation < 90% | P1 = 0.36 | 92 | (24) |
| Oxygen saturation > 90% | q1 = 0.11 | ||
Where, n1 is the sample size.
p1 is the proportion of death among exposed.
q1 is the proportion of death among unexposed.
r ratio of unexposed to exposed.
p proportion of death from the total number of populations in the sample.
q = 1-p.
Zα/2 is standard normal deviation for two-tailed tests based on alpha level (relates to confidence interval level) and Z1-β is standard normal deviation for a one-tailed test based on beta level. Thus, by adding 10% non-response rate the final sample size was 436.
Sampling technique
All referred neonates admitted in NICUs in each hospital between October 1 to November 30, 2020, that meet the inclusion criteria and consented willingly to participate in the study were recruited. First, the total sample was proportionally allocated for each hospital and then individuals were entered into the study consecutively. The average referred neonatal admission in the previous 2 months in four hospitals was 454: Debre Markos, Felege Hiwot, Tibebe Ghion and Gonder Hospitals have an average of 86, 121, 106, and 141 referred neonatal admission respectively. Eighteen neonates were excluded from the study due to exclusion criteria. The selected participants were followed a maximum of 28 postnatal days from admission till the outcome of interest. The study was based on primary and secondary data.
Operational definitions
Referred neonates: are all sick neonates referred and transferred to study area hospitals from other health institutions for special care.
Incidence of referred neonatal mortality: is the probability of neonatal death referred from other health facilities from admission to the 28th day of birth.
Duration of transport: average time spent measured in minutes to transport neonate from last 11 referring health facilities to study hospitals as reported by the respondent.
Referral points: number of referral chain the neonate have before reaching Hospital.
Single referral point: having only one referral point from other health facilities.
Multiple referrals: two or more referral points from other health facilities.
Vital sign monitoring: is measuring and checking any vital signs during transportation of referred neonate.
Intra transport resuscitation: is any treatment given such as oxygen administration, fluid resuscitation, temperature monitoring, and breastfeed during transportation of referred neonate.
Data collection tool and procedure
Data collection tools were adapted from related works of literature and guidelines [21, 23–26] and prepared in the English language for the pretest. Data were collected by a semi-structured questionnaire and checklist for observation and chart review. Both primary and secondary data were used. The prepared tool comprised of socio-demographic, maternal and health, neonatal and referral factors.
Before the study, the period begins an adequate number of data collectors working in the NICU were assigned and taken one-day training. The questionnaires were pretested with 10% of participants before the actual data collection period to see consistency in the recording of variables and clarity of questions. Data were collected by eight nurses face to face interviewing of caregivers, observing and reviewing patient’s medical chart using semi-structured questioner with continuous supervision.
During admission, the current physiologic status of the neonate was evaluated and all necessary information was taken and followed from admission to 28 post-natal days. In the end, participants were classified as not died if the participant is improved and discharged, lost to follow up if communication ended before follow-up period and died if he/she died in hospital before completing follow up period [27]. The outcome was recorded as survived or died.
Data quality control
To achieve data quality the data collection tool was prepared by reviewing related works of literature. Before actual data collection, a pretest was done with 10% of participants at Finote Selam secondary hospital and the appropriateness of the data collection questionnaire and necessary modifications were made on the consistency of the recording of variables and clarity of questions. Staff nurses who were working in NICUs and preferably who had taken basic NICU training were involved in the data collection and one supervisor in each hospital was assigned. One-day training was given for both data collectors and supervisors concerning the data collection tool and data collection process. The supervisors were followed closely and supervise throughout the entire data collection period. The consistency in the recording of variables during follow-up was checked by taking a few patients and amendments were done on the data collection tool.
Data processing and analysis
Data were entered into Epi-data™ Version 4.2 after checking the completeness and consistency and then exported into STATA™ Version 14 for data recording, cleaning and analysis. Then after the outcome of each study participant was dichotomized into died or survived. A bi-variable logistic regression model was fitted for each explanatory variable. Moreover, those variables having a p-value < 0.25 in the Bivariable logistic regression model were selected for multivarible analysis. The odds ratio with its 95% confidence interval and p-values was calculated. In the multivariable logistic regression analysis explanatory variables with p-values < 0.05 were considered as statistically significant and predictors of mortality. Multicollinearity was checked by a variance inflation factor. Hosmer-Lemeshow goodness of fit test was conducted to ascertain whether the model was correctly specified or data conflicted with assumption was made by the model. The result was presented using tables, graphs, figures and text.
Results
Sociodemographic factors
In this study, there was 436 neonatal admission in NICUs of Debre Markose, Felege Hiwot, Tibebe Ghion and Gonder specialized hospitals. The analysis was done on a total of 422 patients. The response rate of this study was 100% with 216 (51.19%) of neonates being males and two hundred thirty-six (55.92%) from the rural area. The Median neonatal age at admission was 2 days with IQR 2–4 days. Two hundred fifty-nine (61.37%) neonates were admitted to NICUS within 2–7 days after birth. The mean (±SD) age of the mothers was 28 (±3.2) years. Two hundred nineteen (51.90%) mothers were 25–34 years age range. One hundred thirty-three (31.51%) neonates were born from mothers who can not read and write and 244(57.82%) mothers are housewives (Table 2).
Table 2.
Sociodemographic characteristics of referred neonates in Amhara regional state comprehensive specialized and specialized Hospitals from October 1 to December 30, 2020 (N = 422)
| Variables | Categories | Frequency | Percent (%) |
|---|---|---|---|
| Sex of neonate | Female | 206 | 48.81 |
| Male | 216 | 51.19 | |
| Age neonate (days) | ⦤ 1 day | 124 | 29.38 |
| 2–7 days | 259 | 61.37 | |
| 8–28 days | 39 | 7.35 | |
| Age of mother (years) | 15–19 | 31 | 7.35 |
| 20–24 | 91 | 21.56 | |
| 25–34 | 219 | 51.90 | |
| ≥35 | 81 | 19.19 | |
| Residence | Urban | 186 | 44.08 |
| Rural | 236 | 55.92 | |
| Maternal occupation | Housewife | 244 | 57.82 |
| Employee (GO and NGO) | 72 | 17.06 | |
| Private work | 106 | 25.12 | |
| Maternal education | Can’t read and write | 133 | 31.51 |
| Primary school | 104 | 24.64 | |
| Secondary school | 65 | 15.40 | |
| Higher education | 120 | 28.45 |
GO Government organization, NGO Non-Governmental Organization
Maternal and Health service-related factors
Almost half (48.34%) of neonates were delivered from mothers who completed four and more ANC visits. Two hundred forty-five (58.06%) and 259 (61.37%) neonates were delivered from multigravida and para (2–4) mothers respectively. Three hundred fourteen (73.41%) neonates were born in a health facility and attended by health personnel. Three hundred ten (73.46%) neonates are vaginal delivery (Table 3).
Table 3.
Maternal and health service factors of referred neonates in Amhara regional state comprehensive specialized and specialized Hospitals from October 1 to December 30, 2020 (N = 422)
| Variables | Categories | Frequency | Percent (%) |
|---|---|---|---|
| ANC follow up | 0 | 25 | 5.92 |
| 1 | 14 | 3.32 | |
| 2–3 | 179 | 42.42 | |
| ⦥4 | 204 | 48.34 | |
| Gravidity | 1 | 117 | 27.73 |
| 2–4 | 245 | 58.06 | |
| ⦥5 | 60 | 14.23 | |
| Parity | 1 | 117 | 27.73 |
| 2–4 | 259 | 61.37 | |
| ⦥5 | 46 | 10.90 | |
| Place of delivery | Home | 108 | 25.59 |
| Health facility | 314 | 73.41 | |
| Delivery mode | Spontaneous vaginal delivery | 310 | 73.46 |
| Cesarean section | 42 | 9.95 | |
| Device assisted | 70 | 16.59 | |
| Birth attendants | Traditional | 108 | 25.59 |
| Skilled | 314 | 74.41 | |
| APH | Yes | 18 | 4.27 |
| No | 404 | 95.73 | |
| PIH | Yes | 11 | 2.61 |
| No | 411 | 97.39 | |
| HIV status | Positive | 7 | 1.66 |
| Negative | 405 | 95.97 | |
| Unknown | 10 | 2.37 |
APH Antepartum Hemorrhage, PIH Pregnancy Induced Hemorrhage, HIV Human Immune Virus
Neonatal related factors
The mean (±SD) admission weight of neonates was 2333.18 (±312.5) gram. One hundred seventy-five (41.47%) neonates were admission weight 1500–2500 g range. During admission two hundred ninety-six (70.14%) neonates were hypothermic, one hundred ninety-eight (46.92%) had hypoglycemia and two hundred twenty-eight (54.03%) were peripheral oxygen saturation less than 90% measured at admission time. Two hundred-sixty four (62.55%) neonates were born after 37 weeks of pregnancy (Table 4).
Table 4.
Neonatal related factors of referred neonates in Amhara regional state comprehensive specialized and specialized Hospitals from October 1 to December 30, 2020 (N = 422)
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Admission weight (gm) | 1000–1500 | 74 | 17.53 |
| 1500–2500 | 175 | 41.47 | |
| ≥2500 | 173 | 41.00 | |
| CRT less than 3 s at admission | Yes | 45 | 10.66 |
| No | 377 | 89.34 | |
| Hypothermia at admission | Yes | 296 | 70.14 |
| No | 126 | 29.86 | |
| Types of pregnancy | Single | 353 | 83.65 |
| Twin | 69 | 16.35 | |
| Oxygen saturation at admission | Yes | 194 | 45.97 |
| No | 228 | 54.03 | |
| Gestational age | < 32 weeks | 55 | 13.03 |
| 32–36 Weeks | 103 | 24.40 | |
| ≥37 weeks | 264 | 62.55 | |
| Hypoglycemia at admission | Yes | 198 | 46.92 |
| No | 224 | 53.08 |
CRT Capillary Refill Time
Referral related factors
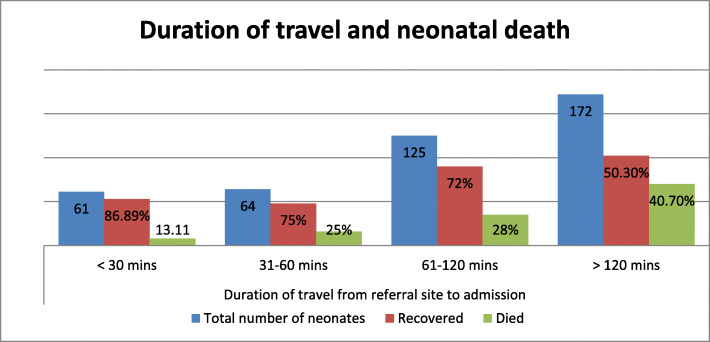
Three hundred eleven (73.70%) had been referred by ambulance. Three hundred twenty-six (77.25%) were followed by health personnel and 317(75.12%) had no intra-transport resuscitation. Two hundred twenty-five (53.32%) were vital signs checked during transfer. The mean distance travel was 107.77 with a range of 44.53–171.01 min. One hundred seventy-two (40.76%) neonates traveled ≥120 mins to access specialty care. About 25.83% of participants cross two or more referral points (Table 5).
Table 5.
Referral-related factors of referred neonates in Amhara regional state comprehensive specialized and specialized Hospitals from October 1 to December 30, 2020 (N = 422)
| Referral related factors | Response /Categories | Frequency | Percent (%) |
|---|---|---|---|
| Vital sign monitoring on transportation | Yes | 225 | 53.32 |
| No | 197 | 46.68 | |
| Referral notes | Yes | 387 | 91.71 |
| No | 35 | 8.29 | |
| Referred by Ambulance | yes | 311 | 73.70 |
| No | 111 | 26.30 | |
| Intra transport resuscitation | Yes | 105 | 24.88 |
| No | 317 | 75.12 | |
| Referral point | One | 313 | 74.17 |
| Two or more | 109 | 25.83 | |
| Health personnel with referred neonate | Yes | 326 | 77.25 |
| No | 96 | 22.75 | |
| Travel time (minutes) | ≤30 | 61 | 14.45 |
| 31–60 | 64 | 15.17 | |
| 61–120 | 125 | 29.62 | |
| ≥120 | 172 | 40.76 | |
| Resuscitation equipment (Ambubag and face mask) | Yes | 112 | 26.54 |
| No | 310 | 73.46 |
From the total of referred neonates 172 neonates travel > 120 mins of distance and 40.70% of neonates died. The graph shows referral neonates who travel long distances have a high probability of death than those who travel short distances (Fig. 1).
Fig. 1.
Shows duration of travel and referred neonatal deaths in each category in Amhara regional state comprehensive specialized and specialized Hospitals from Oct 1 to Dec 30, 2020 (N = 422)
Incidence of referred neonatal mortality
This result showed that the overall mortality rate was found to be 30.60 deaths per 100 referred neonates [95% CI: 26.34–35.16]. The incidence proportion of death respective to completed days was 34.68, 30.88, and 15.38% among neonates referred within 1, 2–7, and 8–28 completed days respectively. From total death 60 (46.51%) were males. About 23 (17.83%) deaths were due to sepsis, 32 (24.80%) premature, 40 (31%) perinatal asphyxia, 3(2.33%) congenital malformation and 31(24.03%) deaths were due to other causes.
Predictors of neonatal mortality
In the Bi-variable logistic regression analysis, variables having a p-value < 0.25 were fitted into the multivariable logistic regression analysis. Likewise, in the bi-variable analysis, place of delivery, mode of delivery, types of pregnancy, gestational age, hypothermia, hypoglycemia, oxygen saturation at admission, prolonged CRT, admission weight, distance traveled to reach referral hospital, age of neonate at admission, vital sign monitoring, mode of transportation, and residence were found to be a candidate for the multivariable logistic regression analysis.
Finally, in the multivariable logistic regression analysis, hypothermia, hypoglycemia and oxygen saturation < 90% at admission, distance to reach referral hospitals, admission weight, home delivery, and age of neonate at admission were found significant predictor of neonatal death among referred neonates who were admitted at NICUs of Amhara regional state comprehensive specialized and specialized hospitals.
This study showed referral neonates who were delivered at home by traditional birth attendants were 2.8 [AOR = 2.89, 95% CI:(1.64–4.77)] times higher risk of death than those who were delivered in the health facility by health professionals. Similarly, neonates who had admission weight less than 1500 g were 3.2 [AOR =3.2, 95% CI: (1.68–6.09)] times higher risk of death than those admission weights greater than 2500 g.
The present study also revealed that the odds of risk of death was 3.8 [AOR = 3.8, 95% CI: (1.65–9.14) times among those who were traveled more than 120 min to reach referral hospitals compared to neonates who travel < 30 min. Being hypothermic at admission time increases the risk of death by 2.7 times compared to non-hypothermic referred neonates [AOR = 2.7, 95%: CI (1.44–5.13).
Moreover, those neonates with oxygen saturation < 90% (SPO2) at admission time were a 1.9 [AOR = 1.9, 95% CI: (1.19–3.21)] times higher risk of death than counterparts. Hypoglycemia increases the risk of death by 1.8 times in hypoglycemic referred neonates compared to non-hypoglycemic referred neonates [AOR = 1.8, 95% CI: (1.11–3.00)].
The age of the neonate at admission time was also another significant predictor. Those neonates who referred before celebrating 1 day of birth were 3.4 [(AOR = 3.4, 95% CI: (1.23–9.84)] times at high risk of death than neonates who were referred after completing 7 days of birth (Table 6).
Table 6.
Bi-variable and multivariable logistic regression analysis to identify the predictors of neonatal mortality among referred neonates admitted in Amhara regional state comprehensive specialized and specialized Hospitals October 1 to December 30, 2020 (N = 422), North, Ethiopia
| Variables | Categories | Outcome status | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Death | Recovered | ||||
| Place of delivery | Home | 49 | 56 | 2.5(1.63–4.1) | 2.8(1.64–4.77)* |
| Health facility | 80 | 237 | 1 | 1 | |
| Mode of delivery | SVD | 102 | 208 | 2.08(0.93–4.67) | 1.17(0.46–2.97) |
| DA | 19 | 51 | 1.6(0.62–4.02) | 1. 18(0.40–3.45) | |
| C/S | 8 | 34 | 1 | ||
| Types of pregnancy | Twin | 33 | 36 | 2.4(1.44–4.16) | 1.24(0.60–2.53) |
| Single | 96 | 257 | 1 | 1 | |
| Gestational age | <32wks | 27 | 28 | 3.14(1.66–5.72) | 1.76(0.78–3.96) |
| 32–36 weeks | 39 | 64 | 1.48(1.27–3.26) | 1.67(0.88–3.16) | |
| ≥37 weeks | 62 | 202 | 1 | 1 | |
| Hypothermia at admission | Yes | 111 | 185 | 3.6(2.07–6.25) | 2.7(1.44–5.13) * |
| No | 18 | 108 | 1 | 1 | |
| Hypoglycemia at admission | Yes | 79 | 119 | 2.3(1.51–3.53) | 1.8(1.11–3.00) * |
| No | 50 | 174 | 1 | 1 | |
| Oxygen desaturation at admission | Yes | 78 | 116 | 2.3(1.52–3.56) | 1.9(1.19–3.21) * |
| No | 51 | 177 | 1 | 1 | |
| Prolonged CRT | Yes | 26 | 19 | 3.6(1.93–6.85) | 1.86(0.85–4.07) |
| No | 103 | 274 | 1 | 1 | |
| Admission weight | < 1500 g | 40 | 34 | 2.8(1.60–4.93) | 3.2(1.68–6.09) * |
| 1500-2500 g | 38 | 137 | 0.7(.40–1.078) | 0.91(.62–1.92) | |
| ≥2500 g | 51 | 122 | 1 | 1 | |
| Distance travelled | ≥120mins | 70 | 102 | 3.5(1.66–7.36) | 3.8(1.65–9.14) * |
| 60–120 min | 33 | 92 | 1.8 (0.83–4.01) | 2.15(0.85–5.41) | |
| 30–60 min | 16 | 48 | 1.7 (0.70–4.11) | 1.54(0.55–4.32) | |
| < 30 mins | 10 | 51 | 1 | 1 | |
| Age of neonate at admission | < 2 day | 43 | 81 | 2.9(1.13–7.51) | 3.4(1.23–9.84)* |
| 2–7 days | 80 | 179 | 2.4(1.95–6.10) | 2.3(0.96–5.71) | |
| 8–28 days | 6 | 33 | 1 | 1 | |
| Vital sign monitoring in transportation | No | 67 | 130 | 1.4(0.89–2.05) | 1.45(0.86–2.44) |
| Yes | 62 | 163 | 1 | 1 | |
| The mode of transportation is an ambulance | No | 44 | 67 | 1.7(1.11–2.75) | 1.58(0.75–4.50) |
| Yes | 85 | 226 | 1 | 1 | |
| Residence | Rural | 82 | 154 | 1.5(0.98–2.29) | 1.01(0.65–1.86) |
| Urban | 47 | 139 | 1 | ||
*significant atp < 0.05
SVD Spontaneous Vaginal Delivery, C/S Cesearen Section, DA Device Assisted
Discussion
The proportion of death among referred neonates admitted in comprehensive specialized and specialized hospitals neonatal intensive care unit in Amhara regional state was [(30.60%) 95% CI: 26.34–35.16)]. The incidence proportion of death was 34.68, 30.88, and 15.38% among neonates referred within 1, 2–7, and 8–28 days respectively. These findings were in line with studies conducted in Gondar comprehensive specialized hospital 28.8% [25], Mauritania 34.7% [28], and tertiary care teaching government hospitals in India 31.98 and 32.9% [8, 29]. However, study finding was higher than previous studies conducted in Ethiopia; Debre Markos referral hospital 21% [22], Amhara regional state referral hospitals 18.6% [21], Tigray 6.04% [30], referral hospital in southern Ethiopia [31] and Nekemte Referral Hospital 8.8% [32] in southern India; 22.8% [33], 20.75% [24], 18.36% [23] and Argentina 17.5% [34]. The higher incidence of death in the present study may be due to a lack of a well-established mobile neonatal intensive care unit with adequately trained manpower that replaces care in NICU of referral Hospitals. For some studies, this might be due to the difference in the study setting which is only referral admissions; vulnerable group, study period, and geographical area.
In contrast, the study finding was lower than previous studies conducted in Guinea 46.8% [19], University Hospital of the West Indies in Jamaica 36% [35], and Bangladesh 54.5% [36]. The discrepancy might be due to the study period and sample size for some studies and other study population was focused on only neonates who were most vulnerable groups [19].
In this study, home delivery was found to be an important predictor of neonatal mortality for those neonates referred to higher specialty care. This finding is in agreement with other previous studies conducted in Gondar Comprehensive Specialized Hospital [25], Bangladesh [36], and India [23]. The possible explanation could be related to a low level of care received at home without any skilled attendants during labor and immediately after birth [26, 37]. Seventy percent of newborns delivered at home in this study were passed two or more referrals, which made delay to receive life-saving interventions.
The present study also showed that the time taken to reach referral hospital > 2 h increases mortality significantly and was found to be an independent predictor for neonatal death. This finding was consistent with the previous studies conducted in Ethiopia [37], Ghana [38], Nigeria [39], and India [8, 13, 23, 40]. Distance to specialty care is an important risk factor for early neonatal mortality. Proximity to health services and a higher level of care associated with lower early neonatal mortality [26, 37].
Also, the present study shows neonates who had hypothermia and oxygen saturation < 90% during admission were at higher risk of death than those who had no hypothermia and oxygen saturation > 90%. Hypothermia and oxygen saturation < 90% during transportation was an independent predictor of neonatal death. This study is similar to a previous study conducted in Ethiopia [11], Mauritania [28], and India [2, 12]. Lack of emergency care on the way to higher centers, poor stabilization before referral and inadequate care during transport increase clinical instability [2, 41].
This study also found hypoglycemia as predicting factor for referred neonatal death. Neonates who have hypoglycemia at admission was 1.8 time at high risk of death than those who were not hypoglycemic. The study conducted in Ethiopia [25], India [40, 42] supports the present study. This may be due to long-distance travel without feeding babies during transportation (If feeding is not contraindicated for some disease pathology), especially for those > 120 mins of distance. Moreover, admission weight less than 1500 g was a predictor of referred neonatal mortality. This finding was similar to studies in India [2, 12] and Guinea [19]. This finding is supported by the clinical practice that very low birth weight neonates are highly affected and lead to death due to vulnerability to the occurrence of life-threatening complications like hypothermia, hypoglycemia, and risk for Hospital-acquired infections.
In this study, the age of neonates was also predicting factor for neonatal death. Neonates referred within 1 day after birth was 3.4 times at high risk than neonates who referred after 7 days of birth. This study was contradicted studies in India [12, 23]. The possible reason my in clinical practice the first 24 h are life-threatening period, referring neonate without pre-referral stabilization and well-established mobile NICU increase risk of death.
Conclusions
In general, the overall magnitude of referred neonatal mortality was 30.57% which was high. Referring without continuity of care similar to care in the NICU lead to a risk of aggravation of the newborn’s condition. The acute neonatal physiology is affected during the transport and adversely affects the outcome. Vital sign monitoring and early recognition of acute physiology of newborns and managing complications, help recovery and decrease mortality. Admission weight, hypothermia, hypoglycemia, travel distance 120 and greater than 120 min, oxygen saturation, age of neonate at admission, and home delivery were independent predictors of mortality. Referring neonates by ambulance accompanied by skilled personnel and emergency resuscitation equipment through close communication and establish a system or referral network that would facilitate transfers to reduce travel and waiting time was recommended. Information pertaining to the time of hospitalization, baby’s temperature and breastfeeding status during transportation which is pertinent to know the hypothermia and hypoglycemia were not addressed in this study.
Acknowledgments
The authors thank Debre Markose University for approval of ethical clearance, technical and financial support of this study. Then, we would like to thank all study participants who participated in this study for their commitment to responding to our interviews and observations. Lastly, we are indebted to each department’s health offices for their assistance and permission to undertake the research.
Abbreviations
- ANC
Antenatal Care
- CBN
Community Based Nutrition
- CBNC
Community based New Born Care
- CEOMNC
Comprehensive Emergency Obstetric Management Newborn Care
- CPAP
Continuous Positive Air Pressure
- CRT
Capillary Refill Time
- CSH
Comprehensive Specialized Hospital
- DMCSH
Debre Markose Comprehensive Specialized Hospital
- EDHS
Ethiopian Demographic Health Survey
- FHCSH
Felege Hiwot Comprehensive Specialized Hospital
- GCSH
Gonder Comprehensive Specialized Hospital
- NETS
Neonatal Emergency Transport Service
- KMC
Kangaroo Mother Care
- LAMA
Left Against Medical Advice
- MDG
Millennium Development Goal
- NETSs
Newborn Emergency Transport Services
- NGOs
Non-Governmental Organization
- NICU
Neonatal Intensive Care Unit
- NMR
Neonatal Mortality Rate
- PNC
Post Natal Care
- SDG
Sustainable Development Goal
- SSA
Sub-Saharan Africa
- SVD
Spontaneous Vaginal Delivery
- TGCSH
Tibebe Gion Comprehensive Specialized Hospital
- TRIPS
Transport Risk Index of Physiologic Stability
- TOPS
Temperature, Oxygen saturation, Perfusion and Blood sugar
- UNICEF
United Nations International Children’s Emergency Fund
Authors’ contributions
All authors involved in Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing-original draft, Writing – review & editing.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Availability of data and materials
On reasonable requests, the full data set and other materials related to this study can be obtained from the corresponding author.
Declarations
Ethics approval and consent to participate
The proposal was approved by the research ethics and approval committee of Debre Markos University health science College with the reference number of HSC/R/C/ser/Co/42/13/13. An official letter of co-operation was written to Debre Markos, Tibebe Gion, Felege Hiwot, and Gonder Comprehensive and Specialized Hospital to facilitating the study. Respondents were provided information on the purpose of the study, its procedures, and their right to refuse or decline participation in the study at any time. Consent was obtained from the study participant’s parents or caregivers and confidentiality was assured as the information they give did not used for any purpose other than the study.
Consent for publication
Not applicable.
Competing interests
There is no competing interest declared by the author.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sankar MJ, Natarajan CK, Das RR, Agarwal R, Chandrasekaran A, Paul VK. When do newborns die? A systematic review of timing of overall and cause-specific neonatal deaths in developing countries. J Perinatol. 2016;36(1):S1–S11. doi: 10.1038/jp.2016.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buch PM, Makwana AM, Chudasama RK, Doshi SK. Status of newborn transport in periphery and risk factors of neonatal mortality among referred newborns. J Phram Biomed Sci. 2012;16:1–6. [Google Scholar]
- 3.Hug L, Alexander M, You D, Alkema L. For child UI. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 2019;7(6):e710–e720. doi: 10.1016/S2214-109X(19)30163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health FDRoE-Mo . Ethiopia: Mini demographic and Health survey. 2019. [Google Scholar]
- 5.Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, Casey DC, Charlson FJ, Chen AZ, Coates MM, Coggeshall M, Dandona L, Dicker DJ, Erskine HE, Ferrari AJ, Fitzmaurice C, Foreman K, Forouzanfar MH, Fraser MS, Fullman N, Gething PW, Goldberg EM, Graetz N, Haagsma JA, Hay SI, Huynh C, Johnson CO, Kassebaum NJ, Kinfu Y, Kulikoff XR, Kutz M, Kyu HH, Larson HJ, Leung J, Liang X, Lim SS, Lind M, Lozano R, Marquez N, Mensah GA, Mikesell J, Mokdad AH, Mooney MD, Nguyen G, Nsoesie E, Pigott DM, Pinho C, Roth GA, Salomon JA, Sandar L, Silpakit N, Sligar A, Sorensen RJD, Stanaway J, Steiner C, Teeple S, Thomas BA, Troeger C, VanderZanden A, Vollset SE, Wanga V, Whiteford HA, Wolock T, Zoeckler L, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, Abreu DMX, Abu-Raddad LJ, Abyu GY, Achoki T, Adelekan AL, Ademi Z, Adou AK, Adsuar JC, Afanvi KA, Afshin A, Agardh EE, Agarwal A, Agrawal A, Kiadaliri AA, Ajala ON, Akanda AS, Akinyemi RO, Akinyemiju TF, Akseer N, Lami FHA, Alabed S, al-Aly Z, Alam K, Alam NKM, Alasfoor D, Aldhahri SF, Aldridge RW, Alegretti MA, Aleman AV, Alemu ZA, Alexander LT, Alhabib S, Ali R, Alkerwi A', Alla F, Allebeck P, al-Raddadi R, Alsharif U, Altirkawi KA, Martin EA, Alvis-Guzman N, Amare AT, Amegah AK, Ameh EA, Amini H, Ammar W, Amrock SM, Andersen HH, Anderson BO, Anderson GM, Antonio CAT, Aregay AF, Ärnlöv J, Arsenijevic VSA, Artaman A, Asayesh H, Asghar RJ, Atique S, Avokpaho EFGA, Awasthi A, Azzopardi P, Bacha U, Badawi A, Bahit MC, Balakrishnan K, Banerjee A, Barac A, Barker-Collo SL, Bärnighausen T, Barregard L, Barrero LH, Basu A, Basu S, Bayou YT, Bazargan-Hejazi S, Beardsley J, Bedi N, Beghi E, Belay HA, Bell B, Bell ML, Bello AK, Bennett DA, Bensenor IM, Berhane A, Bernabé E, Betsu BD, Beyene AS, Bhala N, Bhalla A, Biadgilign S, Bikbov B, Abdulhak AAB, Biroscak BJ, Biryukov S, Bjertness E, Blore JD, Blosser CD, Bohensky MA, Borschmann R, Bose D, Bourne RRA, Brainin M, Brayne CEG, Brazinova A, Breitborde NJK, Brenner H, Brewer JD, Brown A, Brown J, Brugha TS, Buckle GC, Butt ZA, Calabria B, Campos-Nonato IR, Campuzano JC, Carapetis JR, Cárdenas R, Carpenter DO, Carrero JJ, Castañeda-Orjuela CA, Rivas JC, Catalá-López F, Cavalleri F, Cercy K, Cerda J, Chen W, Chew A, Chiang PPC, Chibalabala M, Chibueze CE, Chimed-Ochir O, Chisumpa VH, Choi JYJ, Chowdhury R, Christensen H, Christopher DJ, Ciobanu LG, Cirillo M, Cohen AJ, Colistro V, Colomar M, Colquhoun SM, Cooper C, Cooper LT, Cortinovis M, Cowie BC, Crump JA, Damsere-Derry J, Danawi H, Dandona R, Daoud F, Darby SC, Dargan PI, das Neves J, Davey G, Davis AC, Davitoiu DV, de Castro EF, de Jager P, Leo DD, Degenhardt L, Dellavalle RP, Deribe K, Deribew A, Dharmaratne SD, Dhillon PK, Diaz-Torné C, Ding EL, dos Santos KPB, Dossou E, Driscoll TR, Duan L, Dubey M, Duncan BB, Ellenbogen RG, Ellingsen CL, Elyazar I, Endries AY, Ermakov SP, Eshrati B, Esteghamati A, Estep K, Faghmous IDA, Fahimi S, Faraon EJA, Farid TA, Farinha CSS, Faro A, Farvid MS, Farzadfar F, Feigin VL, Fereshtehnejad SM, Fernandes JG, Fernandes JC, Fischer F, Fitchett JRA, Flaxman A, Foigt N, Fowkes FGR, Franca EB, Franklin RC, Friedman J, Frostad J, Fürst T, Futran ND, Gall SL, Gambashidze K, Gamkrelidze A, Ganguly P, Gankpé FG, Gebre T, Gebrehiwot TT, Gebremedhin AT, Gebru AA, Geleijnse JM, Gessner BD, Ghoshal AG, Gibney KB, Gillum RF, Gilmour S, Giref AZ, Giroud M, Gishu MD, Giussani G, Glaser E, Godwin WW, Gomez-Dantes H, Gona P, Goodridge A, Gopalani SV, Gosselin RA, Gotay CC, Goto A, Gouda HN, Greaves F, Gugnani HC, Gupta R, Gupta R, Gupta V, Gutiérrez RA, Hafezi-Nejad N, Haile D, Hailu AD, Hailu GB, Halasa YA, Hamadeh RR, Hamidi S, Hancock J, Handal AJ, Hankey GJ, Hao Y, Harb HL, Harikrishnan S, Haro JM, Havmoeller R, Heckbert SR, Heredia-Pi IB, Heydarpour P, Hilderink HBM, Hoek HW, Hogg RS, Horino M, Horita N, Hosgood HD, Hotez PJ, Hoy DG, Hsairi M, Htet AS, Htike MMT, Hu G, Huang C, Huang H, Huiart L, Husseini A, Huybrechts I, Huynh G, Iburg KM, Innos K, Inoue M, Iyer VJ, Jacobs TA, Jacobsen KH, Jahanmehr N, Jakovljevic MB, James P, Javanbakht M, Jayaraman SP, Jayatilleke AU, Jeemon P, Jensen PN, Jha V, Jiang G, Jiang Y, Jibat T, Jimenez-Corona A, Jonas JB, Joshi TK, Kabir Z, Kamal R, Kan H, Kant S, Karch A, Karema CK, Karimkhani C, Karletsos D, Karthikeyan G, Kasaeian A, Katibeh M, Kaul A, Kawakami N, Kayibanda JF, Keiyoro PN, Kemmer L, Kemp AH, Kengne AP, Keren A, Kereselidze M, Kesavachandran CN, Khader YS, Khalil IA, Khan AR, Khan EA, Khang YH, Khera S, Khoja TAM, Kieling C, Kim D, Kim YJ, Kissela BM, Kissoon N, Knibbs LD, Knudsen AK, Kokubo Y, Kolte D, Kopec JA, Kosen S, Koul PA, Koyanagi A, Krog NH, Defo BK, Bicer BK, Kudom AA, Kuipers EJ, Kulkarni VS, Kumar GA, Kwan GF, Lal A, Lal DK, Lalloo R, Lallukka T, Lam H, Lam JO, Langan SM, Lansingh VC, Larsson A, Laryea DO, Latif AA, Lawrynowicz AEB, Leigh J, Levi M, Li Y, Lindsay MP, Lipshultz SE, Liu PY, Liu S, Liu Y, Lo LT, Logroscino G, Lotufo PA, Lucas RM, Lunevicius R, Lyons RA, Ma S, Machado VMP, Mackay MT, MacLachlan JH, Razek HMAE, Magdy M, Razek AE, Majdan M, Majeed A, Malekzadeh R, Manamo WAA, Mandisarisa J, Mangalam S, Mapoma CC, Marcenes W, Margolis DJ, Martin GR, Martinez-Raga J, Marzan MB, Masiye F, Mason-Jones AJ, Massano J, Matzopoulos R, Mayosi BM, McGarvey ST, McGrath JJ, McKee M, McMahon BJ, Meaney PA, Mehari A, Mehndiratta MM, Mejia-Rodriguez F, Mekonnen AB, Melaku YA, Memiah P, Memish ZA, Mendoza W, Meretoja A, Meretoja TJ, Mhimbira FA, Micha R, Millear A, Miller TR, Mirarefin M, Misganaw A, Mock CN, Mohammad KA, Mohammadi A, Mohammed S, Mohan V, Mola GLD, Monasta L, Hernandez JCM, Montero P, Montico M, Montine TJ, Moradi-Lakeh M, Morawska L, Morgan K, Mori R, Mozaffarian D, Mueller UO, Murthy GVS, Murthy S, Musa KI, Nachega JB, Nagel G, Naidoo KS, Naik N, Naldi L, Nangia V, Nash D, Nejjari C, Neupane S, Newton CR, Newton JN, Ng M, Ngalesoni FN, de Dieu Ngirabega J, Nguyen QL, Nisar MI, Pete PMN, Nomura M, Norheim OF, Norman PE, Norrving B, Nyakarahuka L, Ogbo FA, Ohkubo T, Ojelabi FA, Olivares PR, Olusanya BO, Olusanya JO, Opio JN, Oren E, Ortiz A, Osman M, Ota E, Ozdemir R, PA M, Pain A, Pandian JD, Pant PR, Papachristou C, Park EK, Park JH, Parry CD, Parsaeian M, Caicedo AJP, Patten SB, Patton GC, Paul VK, Pearce N, Pedro JM, Stokic LP, Pereira DM, Perico N, Pesudovs K, Petzold M, Phillips MR, Piel FB, Pillay JD, Plass D, Platts-Mills JA, Polinder S, Pope CA, Popova S, Poulton RG, Pourmalek F, Prabhakaran D, Qorbani M, Quame-Amaglo J, Quistberg DA, Rafay A, Rahimi K, Rahimi-Movaghar V, Rahman M, Rahman MHU, Rahman SU, Rai RK, Rajavi Z, Rajsic S, Raju M, Rakovac I, Rana SM, Ranabhat CL, Rangaswamy T, Rao P, Rao SR, Refaat AH, Rehm J, Reitsma MB, Remuzzi G, Resnikoff S, Ribeiro AL, Ricci S, Blancas MJR, Roberts B, Roca A, Rojas-Rueda D, Ronfani L, Roshandel G, Rothenbacher D, Roy A, Roy NK, Ruhago GM, Sagar R, Saha S, Sahathevan R, Saleh MM, Sanabria JR, Sanchez-Niño MD, Sanchez-Riera L, Santos IS, Sarmiento-Suarez R, Sartorius B, Satpathy M, Savic M, Sawhney M, Schaub MP, Schmidt MI, Schneider IJC, Schöttker B, Schutte AE, Schwebel DC, Seedat S, Sepanlou SG, Servan-Mori EE, Shackelford KA, Shaddick G, Shaheen A, Shahraz S, Shaikh MA, Shakh-Nazarova M, Sharma R, She J, Sheikhbahaei S, Shen J, Shen Z, Shepard DS, Sheth KN, Shetty BP, Shi P, Shibuya K, Shin MJ, Shiri R, Shiue I, Shrime MG, Sigfusdottir ID, Silberberg DH, Silva DAS, Silveira DGA, Silverberg JI, Simard EP, Singh A, Singh GM, Singh JA, Singh OP, Singh PK, Singh V, Soneji S, Søreide K, Soriano JB, Sposato LA, Sreeramareddy CT, Stathopoulou V, Stein DJ, Stein MB, Stranges S, Stroumpoulis K, Sunguya BF, Sur P, Swaminathan S, Sykes BL, Szoeke CEI, Tabarés-Seisdedos R, Tabb KM, Takahashi K, Takala JS, Talongwa RT, Tandon N, Tavakkoli M, Taye B, Taylor HR, Ao BJT, Tedla BA, Tefera WM, Have MT, Terkawi AS, Tesfay FH, Tessema GA, Thomson AJ, Thorne-Lyman AL, Thrift AG, Thurston GD, Tillmann T, Tirschwell DL, Tonelli M, Topor-Madry R, Topouzis F, Towbin JA, Traebert J, Tran BX, Truelsen T, Trujillo U, Tura AK, Tuzcu EM, Uchendu US, Ukwaja KN, Undurraga EA, Uthman OA, Dingenen RV, van Donkelaar A, Vasankari T, Vasconcelos AMN, Venketasubramanian N, Vidavalur R, Vijayakumar L, Villalpando S, Violante FS, Vlassov VV, Wagner JA, Wagner GR, Wallin MT, Wang L, Watkins DA, Weichenthal S, Weiderpass E, Weintraub RG, Werdecker A, Westerman R, White RA, Wijeratne T, Wilkinson JD, Williams HC, Wiysonge CS, Woldeyohannes SM, Wolfe CDA, Won S, Wong JQ, Woolf AD, Xavier D, Xiao Q, Xu G, Yakob B, Yalew AZ, Yan LL, Yano Y, Yaseri M, Ye P, Yebyo HG, Yip P, Yirsaw BD, Yonemoto N, Yonga G, Younis MZ, Yu S, Zaidi Z, Zaki MES, Zannad F, Zavala DE, Zeeb H, Zeleke BM, Zhang H, Zodpey S, Zonies D, Zuhlke LJ, Vos T, Lopez AD, Murray CJL. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Central Statistical Agency (CSA) [Ethiopia] and ICF. AddisAbaba: Ethiopia Demographic and Health Survey 2016; 2016.
- 7.Tyson J, Kennedy K. Variations in mortality rates among Canadian neonatal intensive care units: interpretation and implications. Cmaj. 2002;166(2):191–192. [PMC free article] [PubMed] [Google Scholar]
- 8.Manikyamba D, Madhavi N, Reddy MS, Satyavani A. Status of Neonatal Transport and Impact of Facilitated Referral on the Outcome of Transported Sick Newborns: At Tertiary Care Hospital. 2015. [Google Scholar]
- 9.Health FDRoE-Mo . Ethiopia: national strategy for newborn and child survival. 2016. [Google Scholar]
- 10.Health FMo . National Newborn and child survival strategy document brief summary 2015/16–2019/20. Addis Ababa: FMOH; 2015. [Google Scholar]
- 11.Asmare Y, Shibabaw W, Yirga T, Dargie A, Hab-tewold TD. The magnitude of neonatal mortality and its predictors in Ethiopia: a systematic review and meta-analysis. bioRxiv. 2019;1:626879. [Google Scholar]
- 12.Meshram RM, Gajimwar VS, Bhongade SD. Predictors of mortality in outborns with neonatal sepsis: a prospective observational study. Niger Postgrad Med J. 2019;26(4):216. doi: 10.4103/npmj.npmj_91_19. [DOI] [PubMed] [Google Scholar]
- 13.Narang M, Kaushik JS, Sharma AK, Faridi MM. Predictors of mortality among the neonates transported to referral Centre in Delhi, India. Indian J Public Health. 2013;57(2):100–104. doi: 10.4103/0019-557X.115003. [DOI] [PubMed] [Google Scholar]
- 14.Choudhury P, Bagga A, Chugh K, Ramji S. Principles of pediatric and neonatal emergencies: JAYPEE BROTHERS MEDICAL PUBLISHERS PVT. LTD.; 2011.
- 15.Cloherty JP, Eichenwald EC, Stark AR. Manual of neonatal care. Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 16.World Health Organization . World health statistics 2016: monitoring health for the SDGs sustainable development goals. World Health Organization; 2016. [Google Scholar]
- 17.Abdulraheem MA, Tongo OO, Orimadegun AE, Akinbami OF. Neonatal transport practices in Ibadan, Nigeria. Pan Afr Med J. 2016;24(1). 10.11604/pamj.2016.24.216.8651. [DOI] [PMC free article] [PubMed]
- 18.Niermeyer S, Domek G. Neonatal transport in developing country settings: A systematic review. 2016. [Google Scholar]
- 19.Sory DI, Sory D, N’fanly C, Ibrahima D, Mamoudou BE, Moussa C, Kleiner MR, Telly S. Neonatal mortality associated with the referral of low birth weight newborns to the Institute of Child Nutrition and Health (INSE) Open J Pediatr. 2019;9(4):287–295. doi: 10.4236/ojped.2019.94027. [DOI] [Google Scholar]
- 20.Sabzehei MK, Basiri B, Shoukohi M, Torabian S, Razavi Z. Factors affecting the complications of interhospital transfer of neonates referred to the neonatal intensive care unit of Besat hospital in 2012–2013. J Clin Neonatol. 2016;5(4):238. doi: 10.4103/2249-4847.194169. [DOI] [Google Scholar]
- 21.Mengistu BA, Yismaw AE, Azene ZN, Mihret MS. Incidence and predictors of neonatal mortality among neonates admitted in Amhara regional state referral hospitals, Ethiopia: prospective follow up study. BMC Pediatr. 2020;20(1):1–4. doi: 10.1186/s12887-020-02031-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alebel A, Wagnew F, Petrucka P, Tesema C, Moges NA, Ketema DB, Melkamu MW, Hibstie YT, Temesgen B, Bitew ZW, Tadesse AA. Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: a prospective cohort study. BMC Pediatr. 2020;20(1):1–1. doi: 10.1186/s12887-020-1963-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sachan R, Singh A, Kumar D, Yadav R, Singh DK, Shukla KM. Predictors of neonatal mortality referred to a tertiary care teaching institute: a descriptive study. Indian J Child Health. 2016;3(2):154–158. doi: 10.32677/IJCH.2016.v03.i02.016. [DOI] [Google Scholar]
- 24.Begum A, Ashwani N, Kumar CS. TOPS: a reliable and simplified tool for predicting mortality in transported neonates. IOSR J Dent Med Sci. 2016;15:53–58. [Google Scholar]
- 25.Yismaw AE, Gelagay AA, Sisay MM. Survival and predictors among preterm neonates admitted at University of Gondar comprehensive specialized hospital neonatal intensive care unit, Northwest Ethiopia. Ital J Pediatr. 2019;45(1):1–1. doi: 10.1186/s13052-018-0597-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pandita KK. Distance from referral hospital as a risk factor for mortality and length of stay of neonates admitted in a tertiary care hospital. Int J Commun Med Public Health. 2019;6(11):4912. doi: 10.18203/2394-6040.ijcmph20195079. [DOI] [Google Scholar]
- 27.Demissie BW, Abera BB, Chichiabellu TY, Astawesegn FH. Neonatal hypothermia and associated factors. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weddih A, Ahmed ML, Sidatt M, Abdelghader N, Abdelghader F, Ahmed A, bouh Regad S, Makhalla K, Heukelbach J, Barkat A. Prevalence and factors associated with neonatal mortality among neonates hospitalized at the National Hospital Nouakchott, Mauritania. Pan Afr Med J. 2019;34. [DOI] [PMC free article] [PubMed]
- 29.Bokade CM, Meshram RM. Morbidity and mortality patterns among outborn referral neonates in Central India: prospective observational study. J Clin Neonatol. 2018;7(3):130. doi: 10.4103/jcn.JCN_27_18. [DOI] [Google Scholar]
- 30.Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region, northern Ethiopia: prospective cohort study. BMC Pregnancy Childbirth. 2016;16(1):1–3. doi: 10.1186/s12884-016-0994-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orsido TT, Asseffa NA, Berheto TM. Predictors of neonatal mortality in neonatal intensive care unit at referral Hospital in Southern Ethiopia: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):1–9. doi: 10.1186/s12884-019-2227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roro EM, Tumtu MI, Gebre DS. Predictors, causes, and trends of neonatal mortality at Nekemte Referral Hospital, east Wollega Zone, western Ethiopia (2010–2014). Retrospective cohort study. PloS One. 2019;14(10):e0221513. doi: 10.1371/journal.pone.0221513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verma SK, Nagaura CP, Goyal VK, Raheja KK, Singh A, Sharma P, Bishnoi RK, Sachdev K. Status of transported neonates and evaluation of tops as a survival score. Indian J Neonatal Med Res. 2017;5(2).
- 34.Goldsmit G, Rabasa C, Rodríguez S, Aguirre Y, Valdés M, Pretz D, Carmona D, López Tornow S, Fariña D. Risk factors associated to clinical deterioration during the transport of sick newborn infants. Arch Argent Pediatr. 2012;110(4):304–309. doi: 10.5546/aap.2012.304. [DOI] [PubMed] [Google Scholar]
- 35.Henry S, Trotman H. Challenges in neonatal transport in Jamaica: a resource-limited setting. J Trop Pediatr. 2017;63(4):307–313. doi: 10.1093/tropej/fmw095. [DOI] [PubMed] [Google Scholar]
- 36.Baidya M, Shirin M, Saha LC. Transport factors affecting the outcome of referred neonates admitted in a tertiary care hospital. Bangl J Child Health. 2017;41(3):159–164. doi: 10.3329/bjch.v41i3.36951. [DOI] [Google Scholar]
- 37.McKinnon B, Harper S, Kaufman JS, Abdullah M. Distance to emergency obstetric services and early neonatal mortality in E thiopia. Tropical Med Int Health. 2014;19(7):780–790. doi: 10.1111/tmi.12323. [DOI] [PubMed] [Google Scholar]
- 38.Tette E, Nuertey BD, Akaateba D, Gandau NB. The transport and outcome of sick outborn neonates admitted to a regional and district hospital in the upper west region of Ghana: a cross-sectional study. Children. 2020;7(3):22. doi: 10.3390/children7030022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abdulraheem MA, Tongo OO, Orimadegun AE, Akinbami OF Neonatal transport practices in Ibadan. Niger Pan Afr Med J. 2016;20:24(1). doi: 10.11604/pamj.2016.24.216.8651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rao SK, Bajaj N, Rawat A. Pre transport factors and transport quality affecting the neonatal outcome. J Evol Med Dent Sci. 2015;4(12):1991–1996. doi: 10.14260/jemds/2015/287. [DOI] [Google Scholar]
- 41.Kumar PP, Kumar CD, Shaik F, Yadav S, Dusa S, Venkatlakshmi A. Transported neonates by a specialist team—how STABLE are they. Indian J Pediatr. 2011;78(7):860–862. doi: 10.1007/s12098-010-0362-0. [DOI] [PubMed] [Google Scholar]
- 42.Sundrani EJ, Katariya U, Mulye S, Yadav D, Patel DS, Sundrani O. Effect of current neonatal transport services on short term outcome of outborn neonates. J Evol Med Dent Sci. 2019;8(1):81–88. doi: 10.14260/jemds/2019/18. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
On reasonable requests, the full data set and other materials related to this study can be obtained from the corresponding author.