FIGURE 1.
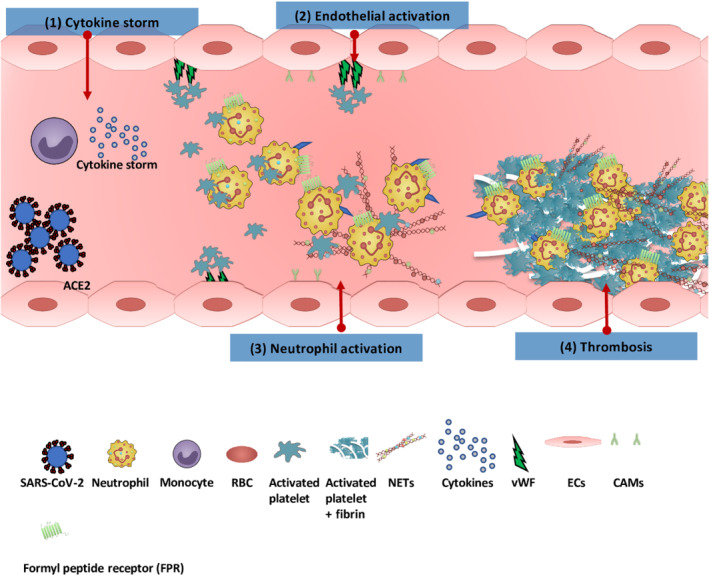
Thromboinflammation in coronavirus disease 2019 (COVID‐19). (1) Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) binds via the ACE2 expressed on the endothelial surface. The virus activates monocytes releasing a cytokine storm (including IL‐6, IL‐1β, IL‐2, IL‐6, IL‐7, IL‐8, IL‐10, IL‐17, TNF‐α, CCL2, CCL3, and CXCL10 , all of which correlate with adverse clinical outcomes). (2) The inflammatory effects of cytokines also activate vascular endothelial cells (ECs), disrupting endothelial function and integrity, which leads to increased platelet and neutrophil recruitment. (3) Increased neutrophil at inflammatory site results in increased expression of adhesion molecules such as L‐selectin, P‐selectin and intercellular adhesion molecule‐1 on ECs. Activated neutrophils release their neutrophil extracellular traps (NETs, which contain a backbone of DNA and citrullinated histone [H3Cit], cathepsin G and neutrophil elastase [NE]), which trap platelets, increasing their activation and aggregation; this in turn further activates neutrophils to produce more NETs. (4) This cycle of events triggers coagulation cascade activation, which in turn increases fibrin formation and thrombosis. CAMs, cellular adhesion molecules; RBC, red blood cell; vWF, von Willebrand factorIFFAHANDGAVINS3
