Abstract
Objective
The SARS-CoV-2 (COVID-19) pandemic has profoundly impacted healthcare delivery and strained medical training. This study explores resident and faculty perceptions regarding the impact of the COVID-19 crisis on technical skill decay of surgical and anesthesia residents. We hypothesized that many residents perceived that their technical abilities diminished due to a short period of interruption in their training.
Design
An IRB-exempt, web-based cross-sectional survey distributed to residents and faculty
Setting
Two large academic tertiary medical centers, North Shore University Hospital and Long Island Jewish Medical Center, of the Northwell Health System in New York.
Participants
General surgery, anesthesiology, plastic surgery, cardiothoracic surgery, orthopedic surgery, oral maxillofacial surgery, urology, podiatry residents and faculty.
Results
All residents reported a significant impact on their training. Residents (82%) and faculty (94%) reported a significant reduction in case volumes due to the COVID-19 pandemic (p < 0.05). 64% of residents reported a reduction in technical skills, and 75% of faculty perceived a decrease in resident technical skills. Residents were concerned about fulfilling ACGME case requirements, however faculty were more optimistic that residents would achieve level-appropriate proficiency by the conclusion of their training. Both residents and faculty felt that resident critical care skills improved as a result of redeployment to COVID-19 intensive care units (66% and 94%). Additionally, residents reported increased confidence in their ability to care for critically ill patients and positive impact on professional competencies.
Conclusions
Effects of the COVID-19 pandemic on residency training are multi-dimensional. The majority of surgical and anesthesia residents perceived that their technical ability diminished as a result of skill decay, whereas other skillsets improved. Longitudinal surveillance of trainees is warranted to evaluate the effect of reduced operative volume and redeployment on professional competency.
KEY WORDS: COVID-19, residency training, skill decay, surgical education
COMPETENCIES: Medical Knowledge, Professionalism, Practice-Based Learning and Improvement, Systems-Based Practice
INTRODUCTION
The SARS-CoV-2 viral pandemic (COVID-19) outbreak that began in Wuhan, China, rapidly spread throughout the world and the United States, becoming one of the worst global pandemics ever experienced.1 New York was among the earliest and hardest hit areas, with over 200,000 reported cases by mid-June, 2020.2 Northwell Health, the largest health system in New York State, treated nearly 85,000 COVID-19 patients, including 16,000 hospitalized COVID-19 patients between March and Labor Day.3 Anticipating a rapid surge of critically ill COVID-19 patients, Northwell Health suspended all elective surgeries a week prior to the March 15, 2020 moratorium.4 As a result, Northwell Health Hospitals, including our flagship program hospitals North Shore University Hospital (NSUH) and Long Island Jewish Medical Center (LIJ), experienced an 85% reduction in operative case volume.5
Given the rapid onset and tremendous burden of COVID-19 patients requiring hospitalization and advanced care, dedicated COVID-19 intensive care units (COVID-ICUs) were created. On March 21, 2020, a multidisciplinary cohort of surgical and procedural residents were redeployed to provide care in these COVID-ICUs.6 Redeployment of residents to these units, together with the decline in elective surgical volume greatly impacted residents’ ability to continue with their traditional training. Particularly, concerns arose that residents would lack the necessary surgical and procedural volume to sustain operative abilities and would experience a phenomenon referred to as “skill decay.”
Skill decay reflects the loss of an acquired, trained skill due to a period of nonuse. It has been described in the context of surgical training related to residents taking gap years (as residents have experienced in research years), and related to surgical military personnel (as experienced in deployments). It also has been noted in other circumstances, such as parental, family or personal leaves of absence, whereby time away from a trained skill may impair long-term abilities. However, the effect of a short period of disruption in training, such as redeployment during the COVID pandemic, on technical skills of procedural-based trainees has not been evaluated.
Recognizing these disturbances in training, the ACGME loosened regulatory constraints by decreasing case requirements for graduating residents as well as extending timelines to achieve case numbers for those still in their training. However, it is still unclear the effect that this reduction in case volume will have on resident's ability to achieve case requirements, fulfill program milestones, and achieve technical competency over the coming years.7, 8, 9, 10, 11, 12, 13, 14, 15
To our knowledge, there is no objective data on the perceived effects of redeployment and decreased operative cases on residency training, particularly related to the impact on residents’ technical surgical-based skills. Our cohort of deployed residents were all trainees of “procedural-based” specialties (including surgical fields and anesthesia), and thus were uniquely affected by reduced case volumes. This study is the first to evaluate the perceptions of residents and faculty in this regard and advances current literature by identifying training concerns of residents and faculty unique to surgical fields when interruptions in traditional training occur. Thus, this work highlights some of the nuances of surgical education that may help guide programs affected by training interruptions, including past and present challenges imparted by the COVID-19 pandemic, and impact on modern residency training.
MATERIALS AND METHODS
On March 21, 2020, elective surgeries were cancelled by the state of New York and within days many residents and fellows were redeployed to COVID-ICUs through May 23, 2020. At NSUH and LIJ in Manhasset and Queens, New York, program directors of general surgery, anesthesiology and surgical subspecialties including plastic surgery, cardiothoracic surgery, orthopedic surgery, oral maxillofacial surgery, urology, and podiatry residency programs formed a consortium of procedural-based specialties called “Multidisciplinary Anesthesia/Surgical Trainees COVID Response Team (MASC).” Through the consortium, a restructuring plan was developed and residents were reorganized into skeleton teams to cover both their specialty services as well as up to 35% of the hospital's system newly created COVID-ICUs.6 All residents were equitably deployed regardless of individual training specialty or training level.
This study utilized an IRB-exempt, web-based, cross-sectional survey distributed to affected residents and faculty of the mentioned cohort consisting of general surgery, surgical subspecialty, and anesthesia residents. This group was studied as theses residents were all included in the pool of procedural residents available for redeployment and were all impacted by the loss of operative volume and deviation from usual technical skill training.6 Administered surveys were de-identified and conducted online through an email-distributed REDCap (Research Electronic Data Capture) survey. REDCap survey system only permits one response per unique resident or faculty. Surveys were distributed on June 5, 2020, 12 days after the end of redeployment, at which time residents and faculty returned from their redeployments and elective surgeries at NSUH and LIJ were resumed. At this time, cases numbers were near recovery to prepandemic volumes.
The resident survey captured resident demographics, training details, objective data reflecting redeployment, resident accounts of numbers of operations and procedures before and during the COVID-19 pandemic, as well as subjective perceptions of residents regarding the impact on residency training. The faculty survey paralleled the resident survey, and similarly captured demographic data, clinical practice details, objective data reflecting redeployments, numbers of operations and procedures before and during the COVID-19 pandemic, as well as subjective perceptions of faculty regarding the impact of the crisis on their trainees. The surveys were worded using inclusive terminology. As such, subjective questions aimed at assessing skill decay were applicable to all surgical specialty and anesthesia trainees in effort to assess their perception of loss of their respective, trained skills. The resident and faculty surveys are provided as supplements. (Supplements A and B)
Survey data was analyzed in Statistical Package for Social Sciences software (SPSS). Two-sided p-values with alpha=.05 were used. Distribution characteristics were tabulated using percentages for categorical variables. Paired t-tests were used for analysis of case and procedural volumes before and during the COVID-19 pandemic. Multivariable logistic regressions were used to evaluate for significant predictors of residency impact and skill decay.
RESULTS
Residents Responses
Surveys were distributed to 173 residents and 91 residents responded, representing 7 specialties for a total response rate of 53%. The resident respondents were R1 residents (29%), followed by R2 (25%), R3 (18%), R4 (10%), R5 (12%), R6 (3%), and research residents (3%). Most respondents were male (68%). The average resident age was 30 years old. (Table 1 ) With the exception of podiatry, all specialties experienced at least 50% redeployment, with larger residencies trending towards higher percentages of redeployment. (Table 2 ) The majority of responses were from general surgery residents (49%). The remainder of responses were from anesthesiology (13%), orthopedic (12%), urology (9%), plastic surgery (5%), cardiothoracic surgery (5%), and oral maxillofacial (3%) residents.
Table 1.
Resident Respondents – Age, Gender, and Clinical Year
| Average Age | 30 |
| Percent of Residents (%) | |
| Male | 68 % |
| R1 | 29 % |
| R2 | 25 % |
| R3 | 18 % |
| R4 | 10 % |
| R5 | 12 % |
| R6 | 3 % |
| Research | 3 % |
Table 2.
Resident Respondents – Specialty and Redeployment
| Total Resident Respondents | Response Rate per Specialty (%) | Percent Residents Redeployed (%) | |
|---|---|---|---|
| General Surgery | 45 | 68% | 69 % |
| Orthopedic Surgery | 11 | 50% | 91 % |
| Anesthesiology | 12 | 48% | 58 % |
| Urology | 8 | 53% | 75 % |
| Plastic Surgery | 5 | 38% | 80 % |
| Cardiothoracic Surgery | 5 | 83% | 100 % |
| Oral Maxillofacial Surgery | 2 | 12.5% | 50 % |
| Podiatry | 3 | 25% | 0 % |
Overall, the majority of residents were redeployed (70%). Of the general surgery residents who reported no redeployment (31%), the majority were either interns (43%) or R5 residents (36%). Of the redeployed residents, the greatest redeployment was to COVID-ICUs (100%). In supplement to covering COVID-ICUs, few residents reported additional redeployment to general surgical services (6%) and general medical services (2%). Specifically, all residents redeployed to COVID-ICUs were responsible for managing critical care patients, including managing respiratory failure, shock, renal failure, hematologic disorders, and providing specialized antiviral care in concert with supervising faculty. In addition, residents performed interventional procedures including airway management, chest tube insertion, and central and arterial line placement with appropriate faculty oversight.
Faculty Responses
Survey links were available to faculty members across all specialties studied, and we received 36 responses representing 4 specialties. Most respondents were male (86%). The average faculty age was 51 years old. (Table 3 ) The majority of responses were from general surgery faculty (72%), including faculty in acute care surgery, trauma surgery, surgical oncology, transplant surgery, vascular surgery, breast surgery, colorectal surgery, and endocrine surgery subspecialties. The remaining responses were from urology (22%), anesthesiology (3%), and podiatry (3%).
Table 3.
Faculty Respondents – Age, Gender, Specialty and Training
| Average Age | 51 |
| Percent of Faculty (%) | |
| Male | 86 % |
| Female | 14 % |
| General Surgery | 72 % |
| Urology | 22 % |
| Podiatry | 3 % |
| Anesthesiology | 3 % |
| Faculty with critical care training |
25 % |
Overall, 28% of faculty reported they were redeployed outside of their specialty. Of those redeployed, 60% were deployed to COVID-ICUs and 40% were deployed to cover general surgical services (including acute care general surgery). Faculty in COVID-ICUs were responsible for overseeing residents manage critical care patients. This similarly included managing respiratory failure, shock, renal failure, hematologic disorders, and providing specialized antiviral care. In addition, faculty supervised residents perform interventional procedures including airway management, chest tube, central line, and arterial line placement. Redeployed faculty covering general surgical services included consulting, admitting, operating on and caring for patients with emergent surgical issues and overseeing residents in these roles.
A total of 86% of faculty reported working with residents all of the time, 5% most of the time, and 9% some of the time prior to the COVID-19 pandemic. During the COVID-19 pandemic, 50% of faculty reporting that they continued to work with residents all of the time and the remainder of faculty reported working with residents less often.
Operative and Technical Training in Residency
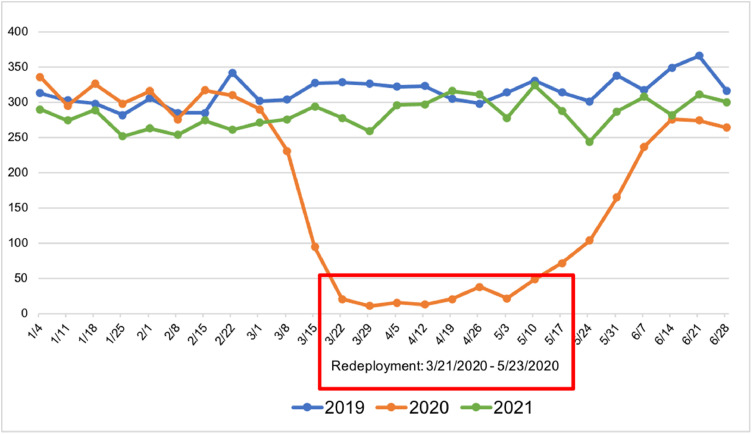
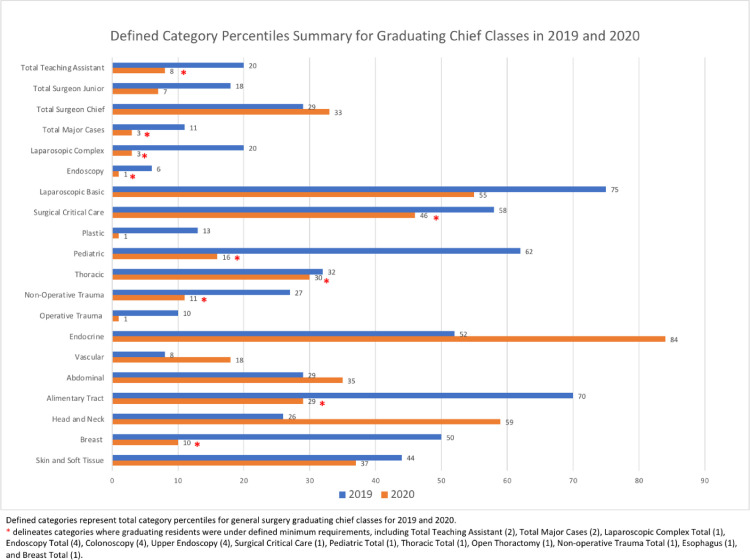
General surgery operative cases during the period of redeployment (March 21st through May 23rd, 2020) were significantly reduced compared to 2019 and 2021 at NSUH and LIJ. (Fig. 1 ) The graduating chief class for general surgery in 2020 had reduced case numbers for most defined categories compared to the graduating chief class of the year prior in 2019. At least three chief residents did not meet defined category minimums across 10 categories for general surgery in 2020. (Fig. 2 ) Residents self-report operative cases through ACGME case-logging system, and this remained consistent through the pandemic. Importantly, the chief class graduating at the height of the pandemic in 2020 was the first class to not meet all defined category minimums within the twenty-year history of our general surgery program.
Figure 1.
Operative cases before, during, and after the COVID-19 pandemic.
Figure 2.
Defined category percentiles summary for graduating chief classes in 2019 and 2020.
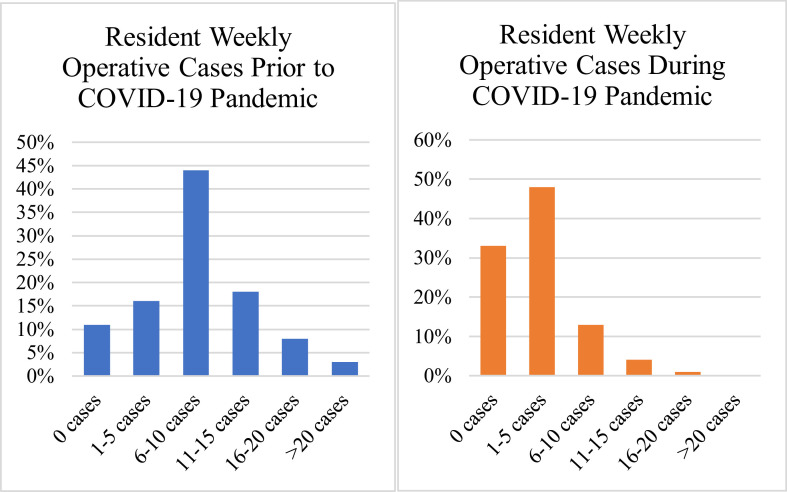
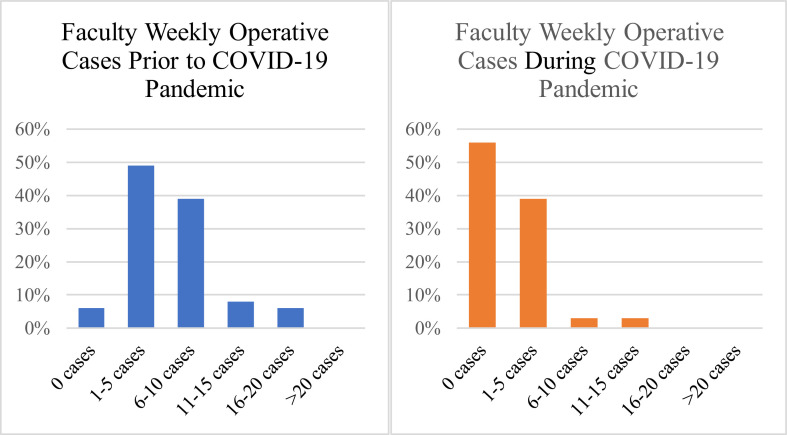
All surveyed residents felt that their training was significantly impacted due to COVID-19 pandemic. The majority of residents (82%) reported a reduction in case volumes. (Fig. 3 ) Residents reported significantly fewer operative cases per week during the COVID-19 pandemic (p < 0.05); however, they reported significantly greater number of procedures per week during the COVID-19 pandemic (p < 0.05). Relative reduction in case volume was not significantly different for each post-graduate year (PGY). The majority of faculty (94%) similarly reported a significant reduction in case volumes due to the COVID-19 pandemic (p < .05), and overall distribution of case volumes trended downwards. (Fig. 4 )
Figure 3.
Resident reported case volumes prior to and during the COVID-19 pandemic.
Figure 4.
Faculty reported case volumes prior to and during the COVID-19 pandemic.
The majority of residents (64%) perceived a reduction in technical operative and technical anesthesia-related skills. Likewise, a majority of faculty (75%) perceived that residents experienced a reduction in technical skill. Age, specialty, and clinical training year were not predictors of skill decay on regression analysis. Re-deployed residents were more likely to report skill decay than residents who were not re-deployed (p < 0.05).
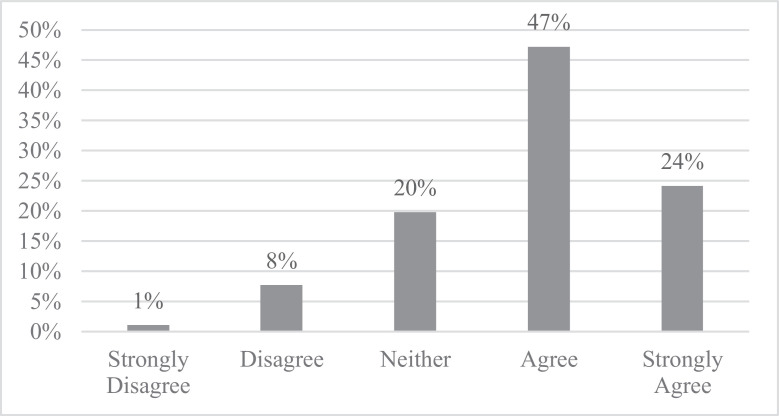
The majority of residents (71%) believed their operative training was negatively impacted by the COVID-19 pandemic. (Fig. 5 ) Resident concerns included return to the operating room with worse skill, surgical skill acquisition for progression to the next clinical year, ability to practice independently as an attending physician, and achievement of ACGME required case numbers. However, faculty were overall confident in residents’ ability to perform level-appropriate operations after the COVID-19 pandemic, as well as in their ability to practice independently after completion of surgical training.
Figure 5.
Resident responses to: “My operative training has been negatively impacted due to the effects of the COVID-19 pandemic.”
The majority of residents did not utilize simulation to maintain their technical skills (58%). Some residents reported using suture kits (39%), laparoscopic trainers (9%), robotic consoles (3%), mannequins (1%) and other specialty-specific trainers (3%) to maintain their operative skills.
Critical Care
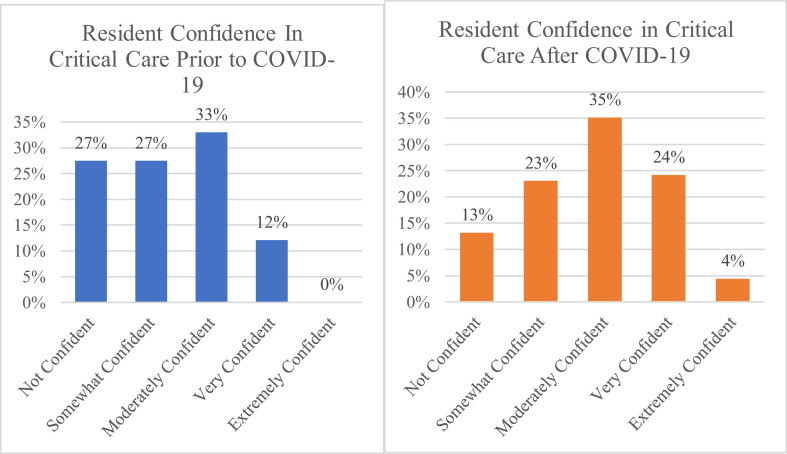
A total of 66% of redeployed residents felt that their critical care skills improved as result of redeployments related to the COVID-19 pandemic. Similarly, most faculty (94%) felt residents' critical care skills improved overall. A total of 55% of resident respondents believed performing critical care procedures helped maintain their operative skills. The majority of residents were more confident in their critical care skills as a result of the COVID-19 pandemic. (Fig. 6 )
Figure 6.
Resident confidence in critical care prior to and during COVID-19.
Health Care Team
Resident members of this procedural based cohort were able to fulfill the needs of the hospital through redeployments and reliance on the group. Redeployed residents (70%) identified working within a new environment on a team of physicians and advanced care providers from different specialties than their own.
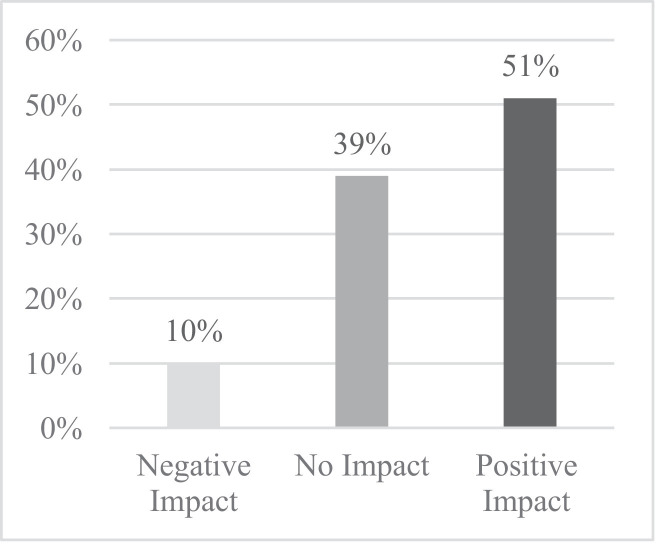
ACGME Core Competencies
Residents believed the COVID-19 pandemic had a positive overall impact on the ACGME core competencies, including patient care, medical knowledge, practice-based learning, interpersonal and communication skills, professionalism, and systems-based practice. (Fig. 7 )
Figure 7.
Overall resident perception on COVID-19 impact on ACGME core competencies.
DISCUSSION
Training of surgical and anesthesia housestaff at Northwell Health flagship hospitals was significantly disrupted by COVID-19. Redeployments to meet healthcare system needs uniquely affected surgical and procedural-based residents by taking them out of the operating room and deploying them to critical care units. Education in surgery, surgical subspecialties, and anesthesia is guided by carefully determined requirements, milestones, and robust operative experiences.16 Emphasis is placed on evaluating resident competency and progression, as well as ensuring adequate case volumes. As hospitals decreased operative cases by cancelling all elective surgeries and re-deploying workforces to areas of greater need, the traditional concept of surgical education within residency training shifted. In effort to ensure continued educational progression of residents, focus shifted to other areas of opportunity, including providing patient care, especially critical care, as well as supporting the development of other nontechnical professional competencies. Even with these opportunities, procedural-based residents experienced a “gap” in their customary training, particularly the growth of their operative technical skills. As a result, many of these residents believed the COVID-19 pandemic negatively impacted their residency training and resulted in skill decay.
Surgical residents commonly perceive technical skill decay upon return to operative duties after periods of nonuse.17 Typically, this phenomenon is reported in residents who take extended periods of time away from operating, such as experienced by residents during research years or during pursuit of advanced degrees. Overall, the greatest impact has revolved around the loss of intraoperative skills of residents, particularly increased loss of skill with more complex tasks and longer periods of non-use.18, 19, 20, 21 However, our data show that despite a much shorter period of non-use during the pandemic, procedural-based residents still perceived a decay in their skills. Uniquely, this introduces the theory that even short periods of non-use may result in perceived technical decline - a concept that has not been addressed in residency training.
A cornerstone of surgical education includes developing residents who are confident in their level-specific operative skill sets. The concerns residents expressed regarding returning to the operating room with worse skill, lacking the surgical skills for progression to the next clinical year, achieving proficiency to practice independently as an attending physician, and completing the ACGME required cases highlight the emphasis that exists on the technical components of surgical education. Residents affected by gaps in training due to a predetermined time period of operative pause (as experienced by research residents), return to their clinical duties with an anticipated volume of residual operative training, which in sum would be equal to a full-training experience. Conversely, many residents experiencing a gap in technical training due to the COVID-19 pandemic believed that the time lost in the operating room would not be regained, and the fear of the loss of potential operative cases may have contributed to fears of skill decay. Moreover, faculty concerns of resident skill decay capture the longstanding nature of the emphasis on technical operative development and volume in training. These views may represent a historical emphasis on technical prowess which persists at the heart of the culture of surgical education.
An additional component of modern surgical education is the utilization of simulation-based training. In response to the changing surgical environment surrounding COVID-19, many residency programs stressed the importance of simulation training to combat resident skill decay.21, 22, 23, 24 However, our residents, and residents nationwide, reported little to no use of surgical simulators over this time.25 This disconnect between potential benefit of utilization and reality may be due to lack of practical access to simulators, trainee stresses, and time constraints particularly during the COVID-19 pandemic. Despite the need for continued technical training, residents at large were unable to overcome barriers to practical utilization of simulation. The lack of more widespread use of simulation underscores the potential for addressing barriers to improve employment of simulation training in surgical residency moving forward. Potential solutions are greater utilization of protected academic time to provide time and resources for residents to work with simulators and greater integration of simulation into scheduled curriculum by program leadership to support its use.
Many programs describe institutional pressures felt regarding the fulfillment of training requirements for residents, including achievement of graduation requirements and case minimums.11 , 13 , 14 , 24, 25, 26, 27 Regulatory bodies, including the ACGME, aim to ensure the adequate training of residents through requirements and regulations. Programs must constantly evaluate resident experiences, including specific operative and procedural case numbers and categories. The decrease in operative cases placed additional pressure on programs to ensure their residents would fulfill these requirements. Although the ACGME allowed for programs to self-declare pandemic emergency status relieving some of this pressure, there remained widespread concern among residents and faculty alike in regards to the long-term implications of decreased operative case volumes and fulfillment of specialty-specific training requirements. Of declared concerns, our residents were most concerned with fulfilling ACGME required case numbers. Despite this concern, faculty still believed residents would achieve level-appropriate proficiency and be able to practice independently at the conclusion of their training. This suggests that the historic reliance on a “number of procedures” based approach may not be the optimal marker for determining procedural skill competency.
Although resident evaluation is complex and the optimal means for ensuring resident readiness for practice remains an area of debate, current practice relies on a comprehensive assessment comprised of core competencies and milestones, with the only objective surrogate marker for ensuring competency being the case requirement minimum. This requirement exists even though there is no data to support that a specific number of procedures equates with competence.28 New trends have suggested that implementing “Entrustable Professional Activities” (EPAs), whereby competencies are operationalized through applying them to clinical situations, may better capture resident capability.29 Our experience over the course of the pandemic provides a new perspective in support of the idea that although residents may self-perceive skill decay as a result of fewer cases, they may still achieve competency as assessed by faculty. Thus, this provides support for exploring new opportunities for resident evaluation, such as the use of EPAs. Learning from our institutions’ experience may help advocate for greater use of these methods in ensuring technical proficiency of surgical and procedural residents.
Despite education-related concerns from reduced case volumes, the overwhelming focus of the health system due to its location in the pandemic's epicenter remained on meeting COVID-19-related needs and the influx of critically ill patients. Although the purpose of re-deployments was to fulfill this need, there were unanticipated consequences greater than mere staffing of COVID-ICUs, as surgical residents gained more exposure and experience in caring for critically ill patients. Time spent in critical care units positively impacted surgical education in this way, allowing residents to gain greater skill and confidence in critical care management and in performing invasive bedside procedures. Residents perceived this as a positive impact on their operative and technical skill base - a finding that supplements the unforeseen benefits imparted by COVID-19 driven re-deployments.
There are additional unanticipated positive effects on resident education and professional development through the COVID-19 pandemic. Similar to other programs, we noted a positive impact of interdisciplinary experience on resident education. Many programs where residents were redeployed supported the exposure to other disciplines as positive opportunities for residents to enhance their knowledge-base and interoperability with other services.22 New roles for surgical residents in unfamiliar environments provided opportunities for residents to develop their leadership skills and ability to work in a team in response to the challenges imparted by different training environments.30
In addition, Northwell residents looked favorably on the impact of the COVID-19 pandemic on ACGME-core competencies, reflecting their outlook on navigating the healthcare system effectively as a competent physician. Despite stresses related to burdened healthcare systems, residents perceived their response to the pandemic regarding their competency in patient care, medical knowledge, practice-based learning, interpersonal and communication skills, professionalism, and systems-based practice as having a positive impact. This further highlights the resiliency of our residents, their ability to adapt to changes in the healthcare system, and their pursuit of educational growth despite a new training environment.
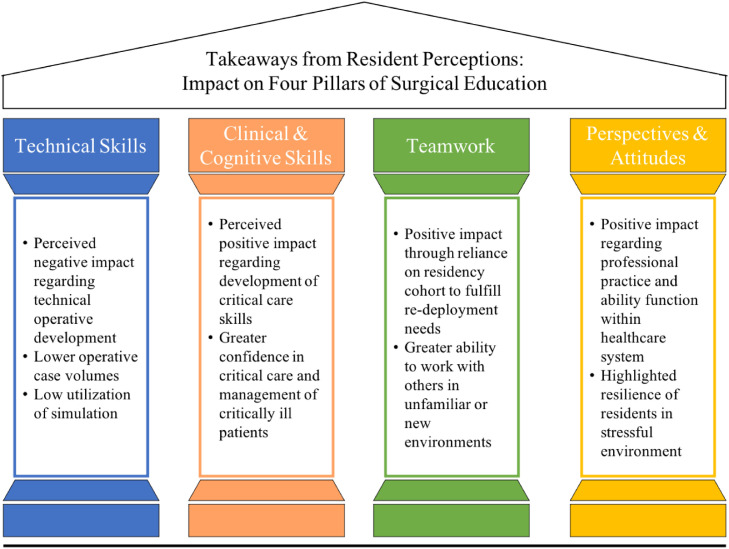
The COVID-19 pandemic has challenged, exposed, and highlighted many areas integral to surgical education including the importance of technical operative and procedural skill, but also the benefits gained by different training environments, teamwork and the importance of resident resilience and flexibility as physician members of healthcare systems. The impact of the pandemic can be seen not only on development of technical skill, but also across additional pillars of education for procedural specialties. (Fig. 8 ) Importantly, with the uncertainty in the future of our nation's state of health, our housestaff's response to the COVID-19 pandemic highlights the importance and necessity of program adaptability. Surgical and anesthesia-based education is constantly evolving, as programs strive to improve the training of residents to support their development into competent, confident, and capable physicians. Despite the expected negative impact of an unprecedented pandemic on residency training, Northwell housestaff demonstrate some of the best possible outcomes in their fluid approach to education through positive takeaways and support of the continued growth of residents while continuing to care for the needs of the community.
Figure 8.
Takeaways from resident perceptions on surgical education.
The limitations of this study are intrinsic to the survey study design. Recall bias could potentially affect our findings. To reduce this affect, our surveys were distributed soon after the end of redeployment. Furthermore, perceived technical skill decay and improvement in other competencies are self-reported by residents; however, faculty with experience in evaluating residents were also surveyed, and their responses provide additional information and validation on perceptions of resident skill. Follow up studies with objective measures to evaluate skill decay resulting from training interruptions are warranted to evaluate the effect on trainee competency.
In learning from our experience, programs may benefit from our unique findings. Periods of non-use, similar to time imparted by the pandemic, may cause trainees to experience skill decay. In these times, programs should stress various means for combatting decay, including taking advantage of procedural opportunities afforded by critical care experiences, as well as integrating simulation in a mindful way that allows for practical use and implementation. Furthermore, in the ways that they provide instruction, faculty should be cognizant that technical skills taught to residents need to be durable and last through such periods of limited- or non-use. Lastly, in times of reduced case numbers, program leadership should place greater value on developing other professional skillsets as highlighted by our pillars of surgical education, with reduced focus on quantity of cases, and heightened focus on quality of comprehensive training.
CONCLUSIONS
The COVID-19 pandemic had a major impact on resident training experience nationwide, which was particularly felt at Northwell hospitals located in the epicenter of the pandemic in New York. Despite a majority of procedural-based residents perceiving a negative impact on residency training regarding development of their technical surgical ability and perceived a skill decay, residents also experienced unanticipated positive development of supporting competencies integral to their education and practice. The disruption in surgical- and procedural-based training strained current education systems and exposed the need for new methods for evaluating technical skill-based proficiency. Thus, our findings not only highlight the major concerns of residents in surgical- and procedural-based fields, but also offer potential for positive takeaways for adapting focuses in residency education as a result of the COVID-19 pandemic.
AUTHOR CONTRIBUTIONS
Initial literature review, survey research design and creation, and submission for IRB-exemption was carried out primarily by the first three authors, including Colleen Nofi DO, Bailey Roberts MD, and Lyudmyla Demyan MD, as well as primary investigator Vihas Patel MD. Survey distribution and analysis of data was carried out primarily by Colleen Nofi DO, Bailey Roberts MD, Lyudmyla Demyan MD, and Nipun Sodhi MD. All authors (Colleen Nofi DO, Bailey Roberts MD, Lyudmyla Demyan MD, Nipun Sodhi MD, Danielle DePeralta MD, Andrea Zimmern MD, Judith Arohnson MD, Ernesto Molmenti MD, and Vihas Patel MD) contributed to interpretation of results and draft of the manuscript. Likewise, all authors equally provided critical review of the manuscript, including edits that in sum comprise the final manuscript for your review.
DECLARATION OF INTERESTS
None
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jsurg.2021.09.005.
Appendix. SUPPLEMENTARY INFORMATION
References
- 1.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for disease control and prevention. Coronavirus disease. (COVID-19) Cases in the U.S. 2019 https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html Accessed June 16, 2020. [Google Scholar]
- 3.Molinet J. Northwell Health. Northwell website patterns predict COVID-19 cases. September 29, 2020 https://www.northwell.edu/northwell-website-patterns-predict-covid-19-cases Accessed October 31, 2020. [Google Scholar]
- 4.de Blasio B. The City of New York Office of the Mayor. Emergency Executive Order No. 100. March 16, 2020 https://www1.nyc.gov/assets/home/downloads/pdf/executive-orders/2020/eeo-100.pdf Accessed June 16, 2020. [Google Scholar]
- 5.Lynam T. Northwell Health. To Reduce Risk of COVID-19, Northwell to Cancel Elective Surgeries in Hospital Settings. March 15, 2020 https://www.northwell.edu/news/the-latest/to-reduce-risk-of-covid-19-northwell-to-cancel-elective-surgeries-in-hospital-settings Accessed June 16, 2020. [Google Scholar]
- 6.Catalano MA, Coppa GF, Patel VM. Transitioning trainees from the operating room to the COVID-19 intensive care unit in New York–Correspondence. Int J Surg. 2020.;155(7):624–627. doi: 10.1016/j.ijsu.2021.105898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He K, Stolarski A, Whang E, Kristo G. Addressing general surgery residents’ concerns in the early phase of the COVID-19 pandemic. J Surgical Education. 2020;77:735–738. doi: 10.1016/j.jsurg.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nassar AH, Zern NK, McIntyre LK, Lynge D, Smith CA, Petersen RP, et al. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: the university of Washington experience. JAMA Surgery. 2020;155(7):624–627. doi: 10.1001/jamasurg.2020.1219. [DOI] [PubMed] [Google Scholar]
- 9.Lancaster EM, Sosa JA, Sammann A, Pierce L, Shen W, Conte MC, et al. Rapid response of an academic surgical department to the COVID-19 pandemic: implications for patients, surgeons, and the community. J Am College Surg. 2020;230:1064–1073. doi: 10.1016/j.jamcollsurg.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meneses E, McKenney M., Elkbuli A. Reforming our general surgery residency program at an Urban Level 1 trauma center during the COVID-19 pandemic: towards maintaining resident safety and wellbeing. The Am J Surg. 2020;220(4):847–849. doi: 10.1016/j.amjsurg.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fero KE, Weinberger JM, Lerman S, Bergman J. Perceived impact of urologic surgery training program modifications due to COVID-19 in the United States. Urology. 2020;143:62–67. doi: 10.1016/j.urology.2020.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scullen T, Mathkour M, Maulucci CM, Dumont AS, Bui CJ, Keen JR. Impact of the COVID-19 pandemic on neurosurgical residency training in New Orleans. World Neurosurgery. 2020;139:718–719. doi: 10.1016/j.wneu.2020.04.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huntley RE, Ludwig DC, Dillon JK. Early effects of COVID-19 on oral and maxillofacial surgery residency training—results from a National Survey. J Oral and Maxillofacial Surg. 2020;78(8):1257–1267. doi: 10.1016/j.joms.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosen GH, Murray KS, Greene KL, Pruthi RS, Richstone L, Mirza M. Effect of COVID-19 on urology residency training: a nationwide survey of program directors by the society of academic urologists. J Urol. 2020;204(5):1039–1045. doi: 10.1097/JU.0000000000001155. [DOI] [PubMed] [Google Scholar]
- 15.Nasca TJ. Accreditation Council for Graduate Medical Education. ACGME Response to Coronavirus (COVID19) March 18, 2020 https://acgme.org/Newsroom/NewsroomDetails/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19 Accessed June 16, 2020. [Google Scholar]
- 16.Accreditation Council for Graduate Medical Education. Defined Category Minimum Numbers for General Surgery Residents and Credit Role. May, 2019 https://www.acgme.org/Portals/0/DefinedCategoryMinimumNumbersforGeneralSurgeryResidentsandCreditRole.pdf Accessed June 16, 2020. [Google Scholar]
- 17.Gawad N, Allen M, Fowler A. Decay of competence with extended research absences during residency training: a scoping review. Cureus. 2019;11:e5971. doi: 10.7759/cureus.5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D'Angelo AD, Ray RD, Jenewein CG, Jones GF. Pugh CM. residents’ perception of skill decay during dedicated research time. J Surg Res. 2015;199:23–31. doi: 10.1016/j.jss.2015.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones GF, Forsyth K, Jenewein CG, Ray RD, DiMarco S, Pugh CM. Research residents’ perceptions of skill decay: effects of repeated skills assessments and scenario difficulty. The Am J Surg. 2017;213:631–636. doi: 10.1016/j.amjsurg.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Gannon SJ, Law KE, Ray RD, Nathwani JN, DiMarco SM, D'Angelo AD, Pugh CM. Do resident's leadership skills relate to ratings of technical skill? J Surg Res. 2016;206:466–471. doi: 10.1016/j.jss.2016.08.050. [DOI] [PubMed] [Google Scholar]
- 21.D'Angelo AD, D'angelo JD, Rogers DA, Pugh CM. Faculty perceptions of resident skills decay during dedicated research fellowships. Am J Surg. 2018;215:336–340. doi: 10.1016/j.amjsurg.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Kwon YS, Tabakin AL, Patel HV, Backstrand JR, Jang TL, Kim IY, et al. Adapting urology residency training in the COVID-19 era. Urology. 2020;141:15–19. doi: 10.1016/j.urology.2020.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stambough JB, Curtin BM, Gililland JM, Guild GN, Kain MS, Karas V, et al. The past, present, and future of orthopedic education: lessons learned from the COVID-19 pandemic. The J Arthroplasty. 2020;35(7):S60–S64. doi: 10.1016/j.arth.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumar A, Agarwal D. Commentary: restructuring residency training in ophthalmology during COVID-19 era: challenges and opportunities. Indian J Ophthalmol. 2020;68:1005. doi: 10.4103/ijo.IJO_1462_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zingaretti N, Contessi Negrini F, Tel A, Tresoldi MM, Bresadola V, Parodi PC. The impact of COVID-19 on plastic surgery residency training. Aesthetic Plastic Surg. 2020;44:1381–1385. doi: 10.1007/s00266-020-01789-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cho DY, Yu JL, Um GT, Beck CM, Vedder NB, Friedrich JB. The early effects of COVID-19 on plastic surgery residency training: the university of Washington experience. Plastic and Reconstructive Surg. 2020;146:447–454. doi: 10.1097/PRS.0000000000007072. [DOI] [PubMed] [Google Scholar]
- 27.Khusid JA, Weinstein CS, Becerra AZ, Kashani M, Robins DJ, Fink LE, et al. Well-being and education of urology residents during the COVID-19 pandemic: results of an American National Survey. Int J Clin Practice. 2020;74(9):e13559. doi: 10.1111/ijcp.13559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steiman J, Sullivan SA, Scarborough J, Wilke L, Pugh C, Bell RH, et al. Measuring competence in surgical training through assessment of surgical entrustable professional activities. J Surg Education. 2018;75:1452–1462. doi: 10.1016/j.jsurg.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 29.Stahl CC, Collins E, Jung SA, Rosser AA, Kraut AS, Schnapp BH, et al. Implementation of entrustable professional activities into a general surgery residency. J Surg Education. 2020;77:739–748. doi: 10.1016/j.jsurg.2020.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hirpara DH, Taylor B. Leadership proficiency in surgery: lessons from the COVID-19 pandemic. Canadian J Surg. 2020;63:E229–E230. doi: 10.1503/cjs.006020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.