FIGURE 1.
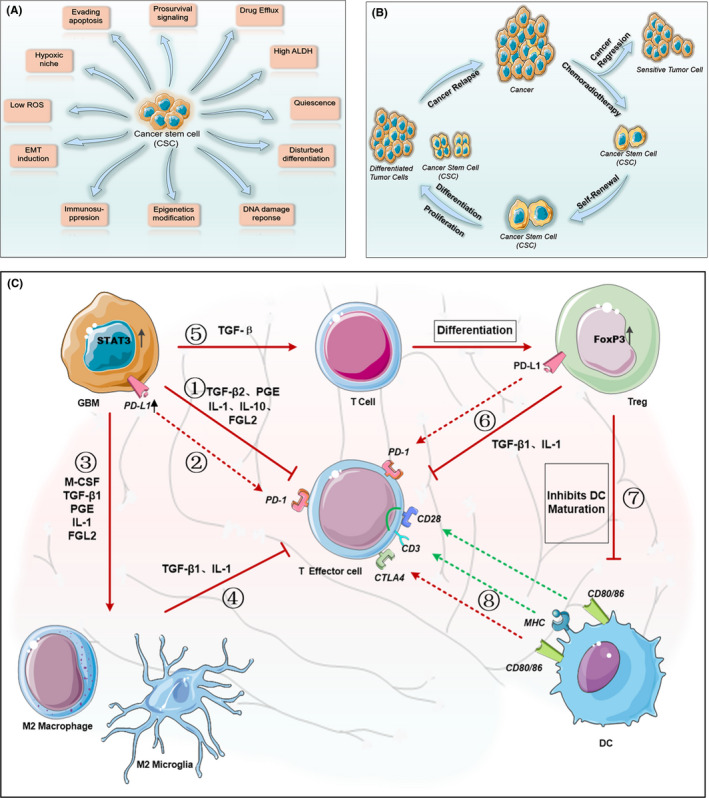
Characteristics of tumor stem cells and composition of immunosuppressive microenvironment in glioblastoma. Cancer stem cells (CSCs) are the main cause of tumor resistance and recurrence. (A) current research shows that the drug resistance mechanisms of tumor stem cells can be divided into 11 aspects. (B) After standard treatment, most of the sensitive tumor cells are cleared. However, tumor stem cells undergo self‐renewal, proliferation, and differentiation through complex mechanisms to escape host defense, and eventually lead to tumor recurrence. Therefore, targeting tumor stem cells to eradicate the tumor is a promising treatment. (C) Glioblastoma immunosuppressive microenvironment. Driven by increased expression of STAT3, glioblastoma cells (1) Secrete immunosuppressive factors such as TGF‐β2, PGE, IL‐1, IL‐10, and FGL2, which are involved in suppressing the activity of effector cells. (2) Up‐regulate PD‐L1 expression on their surface, which binds to PD‐1 on the effector cells and further inhibits effector cell activity. (3) Produce M‐CSF, TGF‐β1 and IL‐10 to polarize macrophages and microglia to immunosuppressive M2 phenotype. (4) M2 tumor‐associated macrophages secrete TGF‐β1 and IL‐10, which are also involved in suppressing effector T cells. (5) TGF‐β secreted by glioma cells causes T cells to express FoxP3 and differentiate into Treg cells. (6) Treg cells secrete TGF‐β1 and IL‐10 and expresses PD‐L1, which further suppress immunoreactive T cells. (7) Treg cells with high expression of FoxP3 inhibit the maturation of dendritic cells and hinder the effective presentation of antigen upon activation by costimulatory signals of CD80/86 and CD28. (8) The MHC molecules of dendritic cells present antigens to effector T cells and induce antigen‐specific immunity. However, CD80/86 may also inhibit the activity of effector T cells by binding to the highly expressed CTLA4 receptor. ROS: reactive oxygen species, ALDH: acetaldehyde dehydrogenase, EMT: epithelial–mesenchymal transition, TGF‐β: Transforming Growth Factor‐β, PGE: Prostaglandin E, IL: interleukin, FGL2: fibrinogen‐like protein 2, PD‐L1: programmed death ligand 1, PD‐1: programmed death 1, M‐CSF: macrophage colony‐stimulating factor, MHC: major histocompatibility complex
