FIGURE 1.
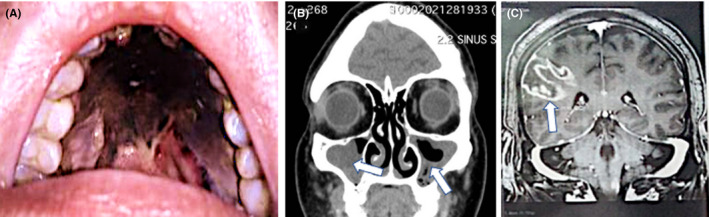
Clinical and radiological features of a 61‐year‐old female patient with poorly controlled diabetes mellitus (type 2) who was diagnosed with moderate‐severity COVID‐19 and invasive rhino‐orbital‐cerebral mucormycosis. The patient had received systemic corticosteroids and broad‐spectrum antibiotics for the management of severe COVID‐19 pneumonia. She eventually succumbed to the disease. On presentation, she had complete right‐sided ptosis, proptosis and complex ophthalmoplegia suggestive of orbital apex syndrome. There was also right peri‐orbital and hemifacial swelling and tenderness. The patient had dysphagia which necessitated the insertion of a nasogastric tube. (A) Examination of the oral cavity revealed the presence of black necrotic tissue involving the palate with pharyngeal extension consistent with an eschar. (B) Coronal CT scan of paranasal sinuses showing bilateral right more than left‐sided opacification of the maxillary sinuses with poor aeration. Gadolinium‐enhanced T1‐weighted axial magnetic resonance imaging demonstrates the presence of a heterogeneously enhancing intra‐orbital lesion with contiguous involvement of the right cavernous sinus. (C) Gadolinium‐enhanced T1‐weighted coronal magnetic resonance imaging of the brain demonstrates the presence of a right‐sided ring‐enhancing lesion suggestive of a fungal abscess
