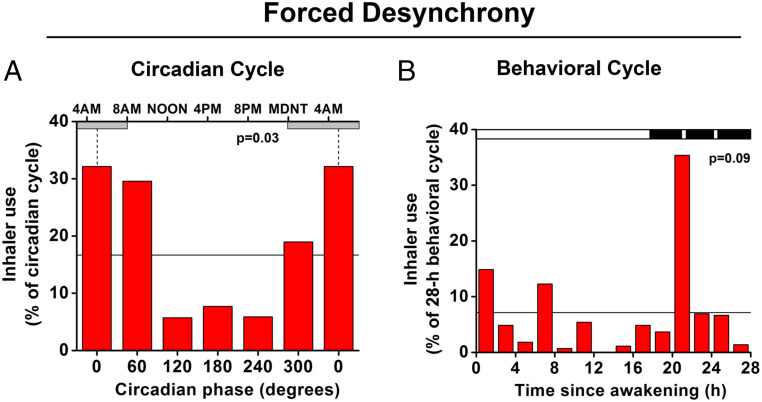
Fig. 5.
Endogenous circadian rhythm in rescue medication. (A) Average distribution of beta2-adrenergic agonist inhaler use across the circadian cycle. Data were derived during the FD protocol from the eight asthma participants who used bronchodilator rescue medication during this protocol. There was a significant rhythm in bronchodilator rescue medication use, which was four times more likely to occur during the biological night (circadian bins 300°, 0°, and 60°; CBT minimum shown by vertical dotted lines at 0° = ∼5:00 AM; gray horizontal bars represent average habitual sleep episodes) than during the biological day (bins 120°, 180°, and 240°). The horizontal line indicates expected relative frequency of inhaler use assuming no circadian rhythm (100/6 circadian phase bins = 16.7%). The P value represents the significance of the circadian effect from nonparametric ANOVA. Note: the first and last bars are double-plotted to make it easier to visualize rhythmicity. B shows effects on inhaler use of the 28-h sleep/wake schedule, averaged across all circadian phases. The black bar represents the sleep period interspersed with three awakenings for pulmonary function measurements. The horizontal line indicates expected relative frequency of inhaler use assuming no effect of time (100/14 2-h bins = 7.1%). There was no overall significant effect of time into the sleep/wake schedule (P = 0.09), yet there was a sharp peak in rescue-inhaler use at the time of the first awakening from sleep, coincident with worst pulmonary function (Fig. 3 E and F).