Abstract
Policy Points.
Mayoral officials’ opinions about the existence and fairness of health disparities in their city are positively associated with the magnitude of income‐based life expectancy disparity in their city.
Associations between mayoral officials’ opinions about health disparities in their city and the magnitude of life expectancy disparity in their city are not moderated by the social or fiscal ideology of mayoral officials or the ideology of their constituents.
Highly visible and publicized information about mortality disparities, such as that related to COVID‐19 disparities, has potential to elevate elected officials’ perceptions of the severity of health disparities and influence their opinions about the issue.
Context
A substantive body of research has explored what factors influence elected officials’ opinions about health issues. However, no studies have assessed the potential influence of the health of an elected official's constituents. We assessed whether the magnitude of income‐based life expectancy disparity within a city was associated with the opinions of that city's mayoral official (i.e., mayor or deputy mayor) about health disparities in their city.
Methods
The independent variable was the magnitude of income‐based life expectancy disparity in US cities. The magnitude was determined by linking 2010‐2015 estimates of life expectancy and median household income for 8,434 census tracts in 224 cities. The dependent variables were mayoral officials’ opinions from a 2016 survey about the existence and fairness of health disparities in their city (n = 224, response rate 30.3%). Multivariable logistic regression was used to adjust for characteristics of mayoral officials (e.g., ideology) and city characteristics.
Findings
In cities in the highest income‐based life expectancy disparity quartile, 50.0% of mayoral officials “strongly agreed” that health disparities existed and 52.7% believed health disparities were “very unfair.” In comparison, among mayoral officials in cities in the lowest disparity quartile 33.9% “strongly agreed” that health disparities existed and 22.2% believed the disparities were “very unfair.” A 1‐year‐larger income‐based life expectancy disparity in a city was associated with 25% higher odds that the city's mayoral official would “strongly agree” that health disparities existed (odds ratio [OR] = 1.25; P = .04) and twice the odds that the city's mayoral official would believe that such disparities were “very unfair” (OR = 2.24; P <.001).
Conclusions
Mayoral officials’ opinions about health disparities in their jurisdictions are generally aligned with, and potentially influenced by, information about the magnitude of income‐based life expectancy disparities among their constituents.
Keywords: health disparities, urban health, small area estimation, local policymaking
Public policies shape patterns in population health, and many of the most influential policies are enacted by elected officials—individual actors who make policy decisions.1 For this reason, while policies have been the focal point of most health policy research, elected officials have also been the focus of substantive inquiry at the intersection of politics and health.2 Such studies survey,3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 interview,15, 18, 19, 20, 21, 22, 23, 24, 25 and observe26, 27, 28, 29 elected officials with the goal of understanding what they think about specific health issues, what they do to address them, and why they think and act as they do. These studies have contributed to theories about health policymaking and informed practices to promote evidence‐informed health policymaking.30
A shortcoming of this body of research about health policymaking, however, is an almost exclusive focus on elected officials without considering the health characteristics of their constituents. Virtually no prior research has examined the extent to which elected officials’ opinions about a health issue are aligned with the epidemiology of that issue among the population that they represent. Addressing this knowledge gap is important to advancing theory and practice about evidence‐informed policymaking. The current study begins to address this by calculating the difference in life expectancy between census tracts in the first and fourth quartiles of median household income within 224 cities and assessing the association between the magnitude of these life expectancy disparities and the opinions of mayoral officials in those cities about the existence and fairness of health disparities in their cities.
Heath disparities—defined as differences in health between socially advantaged and disadvantaged groups31—are one particular issue that warrants attention in policymaking. Health disparities are readily quantifiable, persistent, and pervasive within and between geopolitical jurisdictions in the United States.32, 33, 34, 35 Because elected officials make policy decisions that can exacerbate or attenuate health disparities, it is important for them to be aware of, and concerned about, such disparities among their constituents.34, 36, 37, 38, 39, 40
A 2016 survey of mayoral officials (i.e., mayors and their deputy mayors) in 230 US cities found that these policymakers had limited awareness of health disparities and that their opinions varied dramatically by ideology.3 These results were consistent with prior public opinion research about health disparities.41, 42, 43, 44, 45, 46, 47, 48 However, the extent to which elected officials’ opinions about health disparities might be influenced by the magnitude of the disparities in their cities is unknown. There is a rationale to hypothesize that elected officials are more aware of, and concerned about, health disparities in cities where the magnitude of disparity is larger than other cities, as well as a rationale to hypothesize the opposite.
On the one hand, political science theory related to agenda setting suggests that elected officials are likely to be most aware of, and concerned about, health disparities in jurisdictions where such disparities are most severe.49, 50 As the magnitude of the disparities increases, it is plausible that there is more media coverage, constituent concern, and local health department initiatives related to the disparities. This dynamic could create an “information environment” in which health disparities become more salient to elected officials, which in turn shapes their opinions.51, 52, 53 However, empirical evidence for such a dynamic in health policymaking is limited. One study of state legislatures found that the odds of a bill being introduced to restrict nonmedical exemptions for school‐entry vaccines increased with the incidence of vaccine‐preventable disease in that state.54 In contrast, multiple studies found that the introduction or passage of obesity prevention bills in state legislatures was not associated with state obesity prevalence.55, 56, 57, 58 A limitation of these studies is that they have all focused on behavior at the aggregate legislature (not legislator) level, and none assessed associations between legislators’ opinions about a health issue and the epidemiology of that issue among their constituents.
Alternatively, some theory and research suggest that elected officials might be least aware of, and concerned about, health disparities in jurisdictions where those disparities are most severe.36, 59, 60, 61 Rodriguez59 posits that the presence of health disparities can contribute to the election of representatives who are unaware of, and indifferent to, the health challenges of socially disadvantaged segments of their constituency. This could occur because excess morbidity and mortality among socially disadvantaged groups (i.e., health disparity populations) reduce their political participation and consequently skew election outcomes in favor of more ideologically conservative candidates.60, 61, 62, 63 For example, excess mortality among US Blacks between 1970 and 2004 may have led to Republicans winning seven US Senate elections and 11 gubernatorial elections that would have been won by Democrats if Black‐white mortality disparities did not exist.61
This dynamic would support an inverse relationship between the magnitude of health disparities in a jurisdiction and elected officials’ awareness and concern about such disparities because conservatives are significantly less aware of and concerned about disparities than liberals.3, 41, 42, 43, 44, 45, 46, 47, 48, 64, 65 For example, in the 2016 survey of mayoral officials, 17.6% of socially conservative mayoral officials “strongly agreed” that health disparities existed in their city compared with 61.2% of socially liberal mayoral officials.”3 Also, 20.2% of fiscally conservative mayoral officials believed that such disparities in their city were “very unfair,” while 73.3% of fiscally liberal mayoral officials expressed that belief. Associations between ideology and opinions about health disparities persisted after adjusting for other characteristics of mayoral officials, but those associations could be confounded by the magnitude of health disparities in a given official's city.
Study Aims
The current study begins to address an important gap in health policy research by shedding light on the extent to which elected officials’ opinions about a health issue are aligned with the epidemiological reality of that issue among their constituents. The study aims were to determine if and how the magnitude of income‐based life expectancy disparity within a city was associated with the opinions of that city's mayoral officials about the existence and fairness of health disparities in the city, and to determine if such associations were moderated by the ideology of the mayoral official or the ideology of their city's residents.
Mayoral officials are an important group of policymakers because they influence policy agendas, city spending decisions, and the distribution of resources for health among a city's population.3, 66, 67, 68 To our knowledge, this is the first study to link data on elected officials’ opinions about a health issue with empirical data about that issue among their constituents.
Methods
Survey Data
Data on mayoral officials’ opinions about health disparities were collected through a survey conducted in September through December 2016.3 The mayoral officials were not sent any information about the magnitude of health disparities in their city, or any other epidemiological information, in the survey recruitment materials. The mayor of each US city with a 2015 population equal to or greater than 50,000 (758 cities) was sent two paper versions of the survey, sent seven emails with a link to a web‐based version of the survey, and called up to 20 times to complete the survey over the telephone. Data were collected by SSRS, a survey research firm. Recruitment materials stated that it was preferred for the mayor to complete the survey but their deputy mayor was permitted to complete it as an alternate. The survey was completed by 230 mayoral officials (101 mayors, 129 deputy mayors or equivalent), for a response rate of 30.3%, which is considered good for elected officials69 and was higher than the response rate for other national surveys of elected officials about health issues conducted since 2014.4, 5, 6, 7, 14, 17
Survey data from mayors and deputy mayors were analyzed together because there were no significant differences between the two types of respondents in terms of their opinions about the existence of health disparities (P = .53) or fairness of health disparities (P = .44).3 The study was approved by the Drexel University Institutional Review Board. Additional details about the survey and its results are published elsewhere.3
Nonrespondent analysis (Online Appendix Table A) revealed small but statistically significant differences between cities whose mayoral official completed the survey and cities whose mayoral official did not. Specifically, in the respondents’ cities, the average median household income was lower ($59,235 vs $63,674; P = 0.01); the magnitude of income‐based life expectancy disparity was greater (5.03 years vs 4.71 years; P ˂.01), population size was smaller (132,904 vs 176,897; P = .05); the proportion of cities from the Western US Census region was smaller (30.4% vs 41.5%; P = .02); the percentage of the city population composed of racial/ethnic minority groups was lower (43.3% vs 48.4%; P = .005); and constituent ideology was slightly more liberal (–0.11 vs –0.07, measured on a scale from –1.0 [very liberal] to +1.0 [very conservative]; P = .02). Details about the measurement of these city characteristics are provided later in this article.
No available data allowed us to directly assess differences in the characteristics of survey respondents and nonrespondents. However, to assess whether constituent ideology could be interpreted as an indicator of the mayoral official's ideology, we examined correlations between city constituent ideology70 and self‐reported measures of social and fiscal ideology71—each treated as seven‐point continuous variables—among mayoral officials who completed the survey (details about these measures are provided later). We found moderately strong and statistically significant correlations between constituent ideology and mayoral official social ideology (r = 0.46; P <.0001) and fiscal ideology (r = 0.41; P <.0001). This is consistent with prior research that found the city constituent ideology measure was correlated with the ideology of city governments, measured via the extent to which city tax policies were regressive.70 Taken together, these findings suggest that the magnitude of differences in constituent ideology between the cities governed by survey respondents and those governed by nonrespondents may reasonably approximate the magnitude of differences in ideology between mayoral officials who completed the survey and those who did not.
Because the survey designers assumed that many respondents would be unfamiliar with the term “health disparities,” the survey assessed opinions about such disparities by asking about differences in health between “socially advantaged” and “socially disadvantaged” groups. Drawing from scholarship on operational definitions of health disparity,31, 72, 73, 74 the following text was provided in the survey:
Next are questions about the health of socially advantaged and socially disadvantaged groups. In this questionnaire, socially disadvantaged groups are defined as those that, on average, have less wealth, power, and prestige in a society [emphasis included in survey text]. Examples of groups that have historically been socially disadvantaged in the United States include racial and ethnic minorities, people with low incomes, and people with low levels of education.
Dependent Variables
The primary dependent variable was a mayoral official's opinion about the existence of health disparities in their city. This was assessed by asking, “To what extent do you agree with the statement that socially advantaged groups are in better health than disadvantaged groups in your city?” (1 = “strongly agree,” 2 = “agree,” 3 = “disagree,” 4 = “strongly disagree”). The response data were collapsed into a dichotomous variable (“strongly agree”: yes/no) because only 5.5% of respondents indicated that they “disagree” or “strongly disagree.”
The secondary dependent variable was a mayoral official's belief about the fairness of health disparities in their city. This was used as an indicator of concern about health disparities because prior research has shown that perceptions of health disparities being unfair are a strong predictor of support for government intervention to address these disparities.65 Mayoral officials’ opinions about the fairness of health disparities was assessed by asking, “To what extent do you think that differences in health between socially advantaged and disadvantaged groups in your city are fair?” (1 = “very unfair,” 2 = “somewhat unfair,” 3 = “somewhat fair,” 4 = “very fair”). The response data were collapsed into a three‐level ordinal variable (“very unfair,” “somewhat unfair,” “fair”) with “fair” being composed of respondents who indicated that health disparities were “somewhat fair” (23.6%) of “very fair” (4.2%).
Independent Variable
The primary independent variable was the magnitude of income‐based life expectancy disparity within each mayoral official's city. This was used as the measure of health disparity because life expectancy is a macro indicator of population health.75 Chetty and colleagues35 and the Health Inequality Project76 have estimated an income‐based life expectancy disparity at the US county and metropolitan statistical area levels, but these data were not suitable for our analyses because they do not align with the geopolitical boundaries of mayoral officials’ jurisdictions. The City Health Dashboard project used small‐area estimation techniques to generate measures of morbidity and mortality by race and ethnicity for 500 US cities, and these measures can be used to generate city‐level indicators of health disparity.77 However, small sample sizes and missing data significantly limited the utility of these estimates for our study.
Given the limitations of extant data sources, we created a new data set of city‐level income‐based life expectancy disparity estimates. To generate these estimates, we created a data set that linked 2010‐2015 census tract–level estimates of life expectancy from the US Small‐Area Life Expectancy Estimates Project78 with census tract median household income data from the US Census Bureau for all US cities with a 2015 population estimate equal to or greater than 50,000 (758 cities, the sample frame of the mayoral official survey3). We first identified all census tracts in each of the 758 cities (33,351 tracts). Life expectancy data were missing for 11.0% of these tracts—including in all cities in Wisconsin and Maine (13 cities)—and median household income data were missing for 1.2% of tracts. Cities were excluded from analysis if data on life expectancy or median household income were unavailable, and census tracts were excluded from the city‐level analysis if data were missing for either of these variables. This resulted in a total of 224 cities, and 8,434 census tracts, where the mayoral official had completed the survey.
For each of the 224 cities, we determined the distribution of census tract median household incomes within the city and assigned each tract to a within‐city income quartile rank (first quartile = highest income tracts within the city, fourth quartile = lowest income tracts within the city). To robustly account for variability in the number of census tracts with available data in each city, we used empirical Bayes estimation with random effects to produce estimates of life expectancy for income quartiles within each city, accounting for variation in city‐level life expectancy between cities.79, 80 Specifically, we used multilevel linear regression (level 1 = census tract, level 2 = city) to model census tract life expectancy as a function of income quartile (modeled with an indicator for each quartile), with a random city‐level intercept as well as a random slope for each quartile indicator. Coefficients and appropriate random components were used to derive an empirical Bayes life expectancy value for each income quartile within each city. Finally, we calculated an absolute measure of income‐based life expectancy disparity for each city by subtracting the fourth quartile life expectancy estimate from the first income quartile life expectancy estimate.
The income‐based life expectancy disparity measure for each of the 745 cities included in our analytic sample is provided in Appendix File 1. As shown in Appendix Table B, we explored correlations between our city health disparity measure and the other aforementioned publicly available measures of city health disparity. Our disparity measure was moderately correlated with the Health Inequality Project's metropolitan statistical area–level measure of income‐based life expectancy disparity76 (r = 0.39; P <.0001) as well as a measure of racial low birthweight disparity that we calculated using City Health Dashboard data77 (r = 0.23; P <.0001).
Covariates
To assess mayoral officials’ social and fiscal ideologies, the survey used items from National Election Study Survey questionnaires.71 Mayoral officials separately indicated how they “usually think of [themselves] when it comes to […] ‘social’ and ‘fiscal’ issues” (1 = “extremely liberal,” 7 = “extremely conservative”). Ratings of 1, 2, and 3 were coded as “liberal,” ratings of 4 were coded as “moderate,” and ratings of 5, 6, and 7 were coded as “conservative.”
Mayoral officials’ education and years of service were also assessed. The survey asked mayoral officials to indicate “the highest level of education that [they] completed,” and their responses were coded as “college or less,” “master's degree,” or “doctoral degree.” Mayoral officials also reported “how many years [they] have served in [their] current position,” and this was coded using an empirically derived cut point of <3 years or ≥3 years.
At the city level, we included constituent ideology as a covariate because prior research has shown that decision‐making in local governments often reflects the ideology of constituents within the locality.81, 82 The American Ideology Project70 was the source of the constituent ideology estimates, which were derived from data about the “ideal point” policy preferences from 275,000 participants in the Annenberg National Election Study and the Cooperative Congressional Election Study survey between 2000 and 2011. In the American Ideology Project, Tausanovitch and Warshaw used Bayesian multilevel regression with poststratification methods to generate a constituent ideology score for 1,502 US cities with a population equal to or greater than 25,000, even when survey samples sizes were small within these cities. The constituent ideology score ranges from –1.0 (very liberal) to +1.0 (very conservative).
We included estimates of the proportion of each city's population composed of racial/ethnic minority groups because a prior, separate analysis of the survey data set found that this variable was significantly associated with mayoral officials’ opinions about the effect of stress on health disparities.83 The current study's data on race/ethnicity were obtained from the US Census and operationalized as the percentage of the city's population that was not non‐Hispanic white.
Analysis
Descriptive statistics characterized mayoral officials’ opinions about the existence and fairness of health disparities in their city. We used a two‐way independent sample t test to compare differences in the average (mean) magnitude of income‐based life expectancy disparity between cities whose mayoral official “strongly agreed” that health disparities exist in their city and cities whose mayoral official did not, and we used analysis of variance (ANOVA) to compare the differences in the average (mean) magnitude of income‐based life expectancy disparity among cities whose mayoral officials believed that health disparities were “very unfair,” “somewhat unfair,” or “fair.” These analyses also assessed differences in the magnitude of income‐based life expectancy disparity by the demographic characteristics (e.g., ideology) of the city's mayoral official.
To view the data a different way, we calculated the distribution of magnitudes of income‐based life expectancy disparity across the 224 cities whose mayoral officials completed the survey and assigned each city to a within‐sample city‐level disparity quartile rank (first quartile = smallest disparity, fourth quartile = largest disparity). We then used chi‐square tests to compare the proportions of mayoral officials across quartiles who “strongly agreed” that health disparities existed in their city and who believed that health disparities were “very unfair.”
Finally, we used multivariable logistic regression to assess associations between the magnitude of income‐based life expectancy disparity in cities and mayoral officials’ opinions about health disparities in their city. We ran unadjusted models and models adjusting separately for mayoral official social and fiscal ideology, as well as the percentage of the city's population composed of racial/ethnic minority groups. We also used interaction terms to determine whether associations between the magnitude of income‐based life expectancy disparity and mayoral official opinions about health disparities were moderated by either mayoral official ideology or constituent ideology. We did not include the mayoral demographic variables of highest level of education and years in current position in the regression analysis because these variables were not meaningfully associated with the magnitude of the income‐based life expectancy disparity in the mayoral official's city (i.e., the primary independent variable) or officials’ opinions about the existence and fairness of health disparities in their city (i.e., dependent variables).
Sensitivity Analysis
In the sensitivity analysis, we operationalized the magnitude of income‐based life expectancy (the primary independent variable) in a different way to account for the magnitude of income disparities between cities. We used the same empirical Bayes approach as in the main analysis but estimated the effect of a $10,000 increase in census tract median household income on census tract life expectancy within each city. We then calculated z scores of this income‐based life expectancy disparity for each city and used it as the independent variable in logistic regression models with mayoral officials’ opinions about health disparities as the dependent variable.
Results
In the entire sample of 745 cities for which income‐based life expectancy disparity estimates were calculated, the mean life expectancy in census tracts in the highest‐income (first) quartile of a city was 4.81 years longer than in census tracts in the lowest‐income (fourth) quartile (standard deviation [SD] = 1.28). In the 224 cities where a mayoral official completed the survey, the mean life expectancy was 5.03 years longer in the first quartile than in the fourth (SD = 1.28) (Table 1). Among the mayoral officials who participated in the survey, 41% “strongly agreed” that health disparities existed in their city, 32.9% believed that such disparities were “very unfair,” 39.4% believed they were “somewhat unfair,” and 27.8% believed the disparities were “somewhat fair” or “very fair” (i.e., “fair”). Although “strongly agreeing” that health disparities existed was statistically significantly associated with believing that health disparities were “very unfair” (χ2 = 11.94; P ˂.001), there was only moderate overlap in the mayoral officials who held both of these opinions: Among mayoral officials who “strongly agreed” that health disparities existed in their city, 46.1% believed that these disparities were “very unfair.” Conversely, among mayoral officials who believed that health disparities were “very unfair,” 57.8% “strongly agreed” that such disparities existed.
Table 1.
Characteristics of Survey Participants and Their Cities, n = 224
| Findings | |
|---|---|
| Mayoral official characteristics | |
| Opinions about health disparities | |
| Believe that health disparities exist in their city, % | |
| Strongly disagree | 0.5 |
| Disagree | 5.0 |
| Agree | 53.6 |
| Strongly agree | 41.0 |
| Believe that health disparities in their city are unfair, % | |
| Very unfair | 32.9 |
| Somewhat unfair | 39.4 |
| Somewhat fair | 23.6 |
| Very fair | 4.2 |
| Demographics | |
| Years in professional position, % | |
| <3 | 31.4 |
| ≥3 | 68.6 |
| Highest education level, % | |
| College or less | 45.2 |
| Master's degree | 40.3 |
| Doctoral degree | 14.5 |
| Social ideology, % | |
| Liberal | 43.7 |
| Moderate | 32.1 |
| Conservative | 24.2 |
| Fiscal ideology, % | |
| Liberal | 13.1 |
| Moderate | 27.1 |
| Conservative | 59.8 |
| City characteristics | |
| Population size, mean (SD) | 132,904 (135,393) |
| US Census region, % | |
| Northeast | 12.1 |
| Midwest | 25.0 |
| South | 32.6 |
| West | 30.4 |
| Life expectancy (years), mean (SD) | 78.5 (2.7) |
| Median household income (dollars), mean (SD) | 59,235 (19,655) |
| Magnitude of income‐based life expectancy disparity (years),a mean (SD) | 5.03 (1.28) |
| City constituent ideology score, mean (SD) | –0.11 (0.28) |
| Percentage of city population composed of racial/ethnic minority groups, mean (SD) | 43.3 (21.6) |
The disparity is defined as the difference in income‐based life expectancy, in years, between census tracts in the first and fourth income quartiles within a city.
There were no significant differences in the magnitude of income‐based life expectancy disparity between cities when the mayoral officials were stratified by their demographic characteristics (Table 2). However, the magnitude of income‐based life expectancy disparity was significantly associated with the mayoral official's opinions about the existence and fairness of health disparities in their city. In cities where the mayoral official “strongly agreed” that health disparities existed in their city, the mean magnitude of income‐based life expectancy disparity was 7% (0.36 years) greater than in cities where the mayoral official did not “strongly agree” (5.25 years vs 4.89 years; P = .04) (Table 2). Similarly, in cities where the mayoral official believed that health disparities were “very unfair,” the income‐based life expectancy disparity was 13% (0.7 years) greater than in cities where the mayoral official believed that health disparities were “somewhat unfair,” and 22% (1.11 years) greater than in cities where the mayoral official believed that health disparities were “fair” (5.62 years vs 4.92 years vs 4.51, respectively; P <.001 for all differences).
Table 2.
Mean Magnitude of Income‐Based Life Expectancy Disparity Stratified by Mayoral Officials’ Opinions about Health Disparities in Their City and Mayoral Officials’ Demographic Characteristics, n = 224
| Magnitude of City‐Level Income‐Based Life Expectancy Disparity, yearsa | P | |
|---|---|---|
| Opinions about the health disparities | ||
| Strong agreement that health disparities exist in their city | ||
| Yes | 5.25 | .04 |
| No | 4.89 | |
| Believe that health disparities in their city are unfair | ||
| Very unfair | 5.62 | <.001 |
| Somewhat unfair | 4.92 | |
| Fair | 4.51 | |
| Demographics | ||
| Time in professional position, years | ||
| <3 | 5.19 | .26 |
| ≥3 | 4.96 | |
| Highest education level | ||
| College or less | 4.83 | .11 |
| Master's degree | 5.23 | |
| Doctoral degree | 5.06 | |
| Social ideology | ||
| Liberal | 5.14 | .42 |
| Moderate | 5.00 | |
| Conservative | 4.86 | |
| Fiscal ideology | ||
| Liberal | 5.44 | .09 |
| Moderate | 5.11 | |
| Conservative | 4.89 |
The disparity is defined as the difference in income‐based life expectancy, in years, between census tracts in the first and fourth income quartiles within a city.
P values are from analyses of variance.
Similar associations were observed when mayoral officials were stratified according to their city's within‐sample quartile rank of income‐based life expectancy disparity (Figure 1). Among mayoral officials in cities within the fourth quartile of disparity magnitude (largest disparity; range, 5.75‐9.65 years), 50% “strongly agreed” that health disparities existed in their city, compared to 33.9% of mayoral officials in the first quartile of disparity magnitude (smallest disparity; range, 2.02–4.12 years) (P = .17) (Figure 1, Panel A). Similarly, 52.7% of mayoral officials in the fourth quartile of disparity magnitude believed that health disparities in their city were “very unfair,” compared to 22.2% of mayoral officials in the first quartile of disparity magnitude (P <.001) (Figure 1, Panel B). The differences between Panels A and B in Figure 1 reflect the fact that there was only moderate overlap between the mayoral officials who “strongly agreed” that health disparities existed and those who believed that health disparities were “very unfair.”
Figure 1.
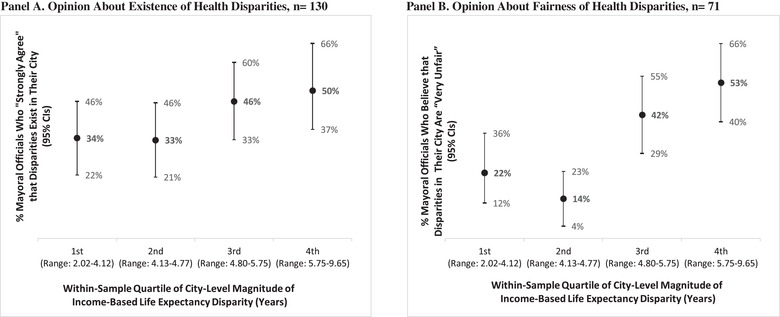
Mayoral Officials’ Opinions About Health Disparities in Their City, Stratified by the Magnitude of Income‐Based Life Expectancy in Their City
P = .17 for chi‐square test. P <.001 for chi‐square test.
With every one‐year increase in the magnitude of income‐based life expectancy disparity within a city, the odds of that city's mayoral official “strongly agreeing” that health disparities exist in their city increased by 25% (odds ratio [OR] = 1.25; 95% confidence interval [CI], 1.01‐1.55) (Table 3). This association was very similar in the sensitivity analysis (OR = 1.28; 95% CI, 0.97‐1.68; Appendix Table C, Model 1). In the main analysis, the association between the magnitude of income‐based life expectancy disparity and mayoral officials’ beliefs about the existence of health disparities was slightly stronger after adjusting for the proportion of the city's population that was composed of racial/ethnicity minority groups (adjusted odds ratio [aOR] = 1.32; 95% CI, 1.06‐1.64), and the association approached significance after adjusting for the official's social ideology (aOR = 1.26; 95% CI, 1.00‐1.59) and fiscal ideology (aOR = 1.23; 95% CI, 0.98‐1.54). The association between the magnitude of income‐based life expectancy disparity in a mayoral official's city and their opinion about the existence of health disparities was not moderated by their social ideology (interaction term P = .44), fiscal ideology (interaction term P = .59), or constituent ideology (interaction term P = .11).
Table 3.
Odds of a Mayoral Official Strongly Agreeing That Health Disparities Exist in Their City
| Model 1a | Model 2b | Model 3c | Model 4d | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | aOR | 95% CI | P | aOR | 95% CI | P | aOR | 95% CI | P | |
| Magnitude of income‐based life expectancy disparity (per one‐year increase in income‐based life expectancy disparity)e | 1.25 | 1.01−1.55 | .04 | 1.23 | 0.98−1.54 | .07 | 1.26 | 1.00−1.59 | .05 | 1.32 | 1.06−1.64 | .02 |
| Fiscal ideology (compared to fiscal conservatives) | ||||||||||||
| Fiscally liberal | 3.16 | 1.36−7.37 | .01 | 2.88 | 1.23−6.78 | .02 | − | − | − | − | − | − |
| Fiscally moderate | 2.19 | 1.16−4.13 | .02 | 2.12 | 1.12−4.02 | .02 | − | − | − | − | − | − |
| Social ideology (compared to social conservatives) | ||||||||||||
| Socially liberal | 6.77 | 3.02−15.14 | <.001 | − | − | − | 6.56 | 2.91−14.76 | <.001 | − | − | − |
| Socially moderate | 1.97 | 0.84−4.63 | .12 | − | − | − | 1.92 | 0.81−4.55 | .14 | − | − | − |
| Percentage of city population composed of racial/ethnic minority groups (per 1% increase in city's minority population) | 1.02 | 1.00−1.03 | .02 | − | − | − | − | − | − | 1.02 | 1.01−1.03 | .01 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
Model 1 is unadjusted.
Model 2 is adjusted for city life expectancy disparity and mayoral official fiscal ideology.
Model 3 is adjusted for city life expectancy disparity and mayoral official social ideology.
Model 4 is adjusted for city life expectancy disparity and percentage of city population that is racial/ethnic minority.
The disparity is defined as the difference in income‐based life expectancy, in years, between census tracts in the first and fourth income quartiles within a city.
Table 4 demonstrates that with every one‐year increase in the magnitude of income‐based life expectancy disparity within a city, the odds of the mayoral official believing that health disparities in their city were “very unfair,” compared to “fair,” doubled (OR = 2.24; 95% CI, 1.59‐3.14). As shown in the data for Model 1 in Appendix Table D, this association remained significant in the sensitivity analysis (OR = 2.90; 95% CI, 1.89‐4.46). In the main analysis, the association between the magnitude of income‐based life expectancy disparity and beliefs about the fairness of health disparities was similar after adjusting for (a) the proportion of the city's population from racial/ethnic minority groups (aOR = 2.45; 95% CI, 1.71‐3.52), (b) social ideology (aOR = 2.23; 95% CI, 1.55‐3.22), and (c) fiscal ideology (aOR = 2.17; 95% CI, 1.51‐3.12). The association between the magnitude of income‐based life expectancy disparity in a mayoral official's city and their belief about the fairness of health disparities was not moderated by their (a) social ideology (interaction term P = .47), (b) fiscal ideology (interaction term P = .79), or (c) constituent ideology (interaction term P = .51).
Table 4.
Odds of a Mayoral Official Believing That Health Disparities in Their City Are Very Unfair (Compared to Fair)
| Model 1a | Model 2b | Model 3c | Model 4d | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | aOR | 95% CI | P | aOR | 95% CI | P | aOR | 95% CI | P | |
| Magnitude of income‐based life expectancy disparity (per one‐year increase in income‐based life expectancy disparity)e | 2.24 | 1.59−3.14 | <.001 | 2.17 | 1.51−3.12 | <.001 | 2.23 | 1.55−3.22 | <.001 | 2.45 | 1.71−3.52 | <.001 |
| Fiscal ideology (compared to fiscal conservatives) | ||||||||||||
| Fiscally liberal | 16.15 | 3.49−74.86 | <.001 | 15.60 | 3.19−76.35 | .00 | − | − | − | − | − | − |
| Fiscally moderate | 2.54 | 1.11−5.82 | .03 | 2.37 | 0.99−5.68 | .05 | − | − | − | − | − | − |
| Social ideology (compared to social conservatives) | ||||||||||||
| Socially liberal | 11.40 | 3.63−35.84 | <.001 | − | − | − | 11.16 | 3.39−36.70 | <.001 | − | − | − |
| Socially moderate | 2.85 | 0.89−9.09 | .08 | − | − | − | 2.52 | 0.75−8.43 | .13 | − | − | − |
| Percentage of city population composed of racial/ethnic minority groups (per 1% increase in city's minority population) | 1.01 | 1.00−1.03 | .16 | − | − | − | − | − | − | 1.02 | 1.01−1.04 | .01 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
Model 1 is unadjusted.
Model 2 is adjusted for city life expectancy disparity and mayoral official fiscal ideology.
Model 3 is adjusted for city life expectancy disparity and mayoral official social ideology.
Model 4 is adjusted for city life expectancy disparity and percentage of city population that is racial/ethnic minority.
The disparity is defined as the difference in income‐based life expectancy, in years, between census tracts in the first and fourth income quartiles within a city.
Similar, albeit weaker, associations were observed when mayoral officials who believed that health disparities were “somewhat unfair” were compared to those who believed health disparities were “fair” (results not shown in tables). With every one‐year increase in the magnitude of income‐based life expectancy disparity, the odds of the mayoral official believing that health disparities in their city were “somewhat unfair” compared to “fair,” increased by 45% (OR = 1.44; 95% CI, 1.05‐2.00).
Discussion
This study is the first, to our knowledge, to examine how elected officials’ opinions about a health issue align with the epidemiological reality of that issue among their constituents. We found that mayoral officials were more aware of the existence of health disparities and perceived health disparities as more unfair in cities where the magnitude of income‐based life expectancy disparity was larger. Although the mechanisms underlying this relationship are unobserved, it is possible that health disparities are more salient to elected officials in cities with larger disparities because these officials are exposed to more information about the disparities (e.g., via local news media, constituent communication, and government reports). This dynamic could in turn increase the visibility of, and enhance perceptions about the severity of, health disparities among elected officials and influence their opinions about the issue.
This line of reasoning is consistent with political science research and theory about issue salience and agenda setting.49, 50 For example, studies have shown that the volume of media coverage about an issue is predictive of the amount of legislative attention it receives (e.g., the number of bills introduced to address it).51, 52, 53 The notion that the magnitude of disparities within a city influences mayoral opinions about those disparities is also supported by our observation of a dose‐response relationship between the magnitude of income‐based life expectancy disparity and the intensity of the mayoral official's fairness belief. For example, the average magnitude of income‐based life expectancy disparity was significantly larger in cities where the mayoral official believed that health disparities were “very unfair” (5.62 years) than in cities where the official believed health disparities were “somewhat unfair” (4.92 years), and the average magnitude of income‐based life expectancy disparity in the cities where the official believed health disparities were somewhat unfair was significantly larger than in cities where the mayoral official believed they were “fair” (4.51 years).
Our results should be considered within the context of prior studies that found no association between state obesity prevalence and state legislature activity to address the issue.55, 56, 57, 58 Our results may differ because these prior studies were limited to associations between obesity prevalence and legislative action at the state legislature level, not opinions at the legislator level. It is possible that elected officials’ opinions about a health issue are often aligned with the epidemiology of that issue while their legislative behaviors are not because these behaviors are influenced by a wide range of factors (e.g., political strategy, finances).
Our findings also diverge from research and theory suggesting that health disparities could skew election outcomes in favor of conservative candidates, who are typically less aware of and less concerned about health disparities.3, 41, 42, 43, 44, 45, 46, 47, 48, 64, 65 We found that the magnitude of income‐based life expectancy disparity was larger in cities where the mayoral official was fiscally liberal (5.44 years) than in cities where the official was moderate (5.11 years) or conservative (4.89 years); however, this finding is not significant (P = .09). One reason why our findings are inconsistent with the prior work of Rodriguez and colleagues59 might be that we focus on cities, where the dynamics of electoral politics are likely different at the local than state and federal levels.84
Our results reinforce prior research suggesting that ideology is among the most influential determinants of elected officials’ opinions about health issues.85, 86, 87 Although the strength of associations between income‐based life expectancy disparity and mayoral officials’ opinions about health disparities were significant, the magnitude of these associations was smaller than the magnitude of the associations between ideology and opinions about health disparities. For example, while we found that a one‐year larger income‐based life expectancy disparity was independently associated with two times higher odds of a mayoral official believing that health disparities were “very unfair” (relative to “fair”), a socially liberal mayoral official had 12 times higher odds of believing that health disparities were “very unfair” (relative to “fair”) than a socially conservative official.
Other studies of elected officials have found that ideology is a substantially stronger predictor of opinions about health issues than constituent characteristics. For example, a 2017 survey‐based study found that liberal ideology was much more strongly associated with a state legislator's support for behavioral health parity laws than relevant characteristics of their state's population (e.g., the percentage of the population covered by insurance who would benefit from the laws, opioid overdose death rate).16 While our study suggests that evidence about epidemiology of health issues could potentially influence elected officials’ opinions, it also reinforces the importance of tailoring data summaries about population health problems and strategies to address them for audiences with different ideologies.7, 88, 89
Our study highlights several areas for future research. First, there would be value to assessing whether the volume of local news media coverage about health disparities mediates the observed association between the magnitude of income‐based life expectancy disparity and mayoral officials’ opinions.90, 91 News coverage is a probable, but unobserved, mechanism responsible for the study findings. It would also be worth exploring whether the robustness of local news media environments (e.g., the number of local newspapers) is associated with coverage about health disparities; this is a topic of interest because approximately one in five local newspapers in the United States shut down between 2004 and 2018.92 There would also be benefit to future research to shed light on the sources and processes through which mayoral officials receive evidence about health disparities (and health issues more broadly). In a Philadelphia case study, researchers found that city policymakers obtained evidence about sugar‐sweetened beverage taxes from multiple sources (e.g., university and government reports, local news media),25 but it is unclear how these findings might extend to different contexts. There could also be value to learning if and how elected officials’ opinions about health disparities change during their time in office.
Although the dynamics of city policymaking are likely different than those at the state and federal levels,84 there would be value in attempting to replicate our study at different levels of government. At the state level, methods similar to those used in the current study could be used to generate estimates of health disparity in state legislative districts, which could be linked to survey data from state legislators. At the federal level, estimates of population health status within US congressional districts have been generated using data from the Behavioral Health Risk Factor Surveillance System and could produce estimates of health disparity within congressional districts.93, 94 While it is challenging to obtain survey data from federal legislators, their legislative behaviors (e.g., bills introduced and public statements related to health disparity) can serve as indicators of the extent to which addressing health disparities is an issue on their policy agenda.95, 96
Limitations
Our study has five main limitations. First, although the mayoral official survey response rate (30.3%) is considered good for elected officials69 and was higher than recent surveys of this population,4, 5, 6, 7, 14, 17 small but statistically significant differences were observed between the cities whose mayoral officials completed the survey and cities whose mayoral officials did not participate. Also, when comparing participating and nonparticipating mayoral officials, we were only able to observe differences between the characteristics of their cities—not differences between the characteristics of the respondents and nonrespondents. Our analysis suggests that city constituent ideology may be a reasonable indicator of mayoral official ideology—consistent with prior research about the association between the city constituent ideology measure and city policies.70 But we cannot know whether mayoral officials who completed the survey had different ideological orientations and opinions about health disparities than those who did not complete the survey.
Second, the study only focused on one type of policymaker (mayoral officials), one level of government (local), and one health issue (health disparities). Our results are not necessarily generalizable to different types of policymakers, levels of government, or health issues. Furthermore, our survey questions were broadly focused on health disparities—defined as differences in health between socially advantaged and disadvantaged groups—and differences in life expectancy by income was our indicator of disparity magnitude. It is possible that our results would be different if racial/ethnic differences in either life expectancy or measures of morbidity were used as indicators of health disparity.65
Third, we aggregated ecological data from census tracts to generate place‐based estimates of income‐based life expectancy disparity. Because there is heterogeneity in both income and life expectancy within census tracts, our disparity estimates are not as precise as those that have been created using individual data.35 More precise estimates of health disparities in cities, however, would theoretically strengthen, not weaken, the associations observed if mayoral officials’ opinions about health disparities are indeed influenced by the epidemiological reality of health disparities among their constituents.
Fourth, the American Ideology Project measure of city constituent ideology70 was created using survey data from 2000 through 2011, and the mayoral official health disparity survey3 was fielded in 2016. Thus, the ideology measure might not precisely reflect the ideology of constituents at the time when mayoral officials completed the 2016 survey.
Fifth, the relevance of our findings may be limited because it is possible that mayoral officials’ opinions about health disparities have changed substantially since the 2016 survey. Recently, widespread media coverage about racial disparities in COVID‐19 infection and mortality rates may have increased mayoral officials’ awareness of the existence of health disparities in their cities and affected their beliefs about the fairness of such disparities.97 Relatedly, racial disparities in COVID‐19 mortality could impact the magnitude of income‐based life expectancy disparities in cities. There would be value in future research assessing associations between the magnitude of racial/ethnic COVID‐19 mortality disparities in cities and city policymakers’ opinions about health disparities related to COVID‐19.
Conclusion
Mayoral officials’ opinions about the existence and fairness of health disparities in their cities are generally aligned with empirical data about the magnitude of income‐based life expectancy disparities among their constituents. If exposure to information about health disparities is responsible for the associations observed, highly visible and well‐publicized information about such disparities—such as recent information related to racial/ethnic differences in COVID‐19 infection rates and morbidity and mortality—has the potential to influence elected officials’ opinions about the disparities and their political will to address them. Future research linking data on constituent heath with elected officials’ opinions and behaviors is needed. The current study offers of a model to stimulate research in this domain.
Funding/Support: Urban Health Collaborative Pilot Grant, Robert Wood Johnson Foundation (73960).
Conflict of Interest Disclosures: All authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest. No conflicts were reported.
Supporting information
Appendix Table A. Characteristics of Cities Governed by Survey Respondents and Nonrespondents
Appendix Table B. Correlations Between the Measure of City Health Disparity Used for the Analysis and Other Publicly Available Measures of Health Disparities in US Cities
Appendix Table C. Sensitivity Analysis: Odds of Mayoral Official Strongly Agreeing That Health Disparities Exist in Their City Given the Magnitude of Life Expectancy Disparitya per $10,000 of Income, z score standardized
Appendix Table D. Sensitivity Analysis: Odds of Mayoral Official Believing That Health Disparities in Their City Are Very Unfair (Compared to Fair) Given the Magnitude of Life Expectancy Disparitya per $10,000 income, z score standardized
Supporting Material
References
- 1.Kingdon JW. Congressmen's Voting Decisions. Ann Arbor: University of Michigan Press; 1989. [Google Scholar]
- 2.Burris S, Wagenaar AC, Swanson J, Ibrahim JK, Wood J, Mello MM. Making the case for laws that improve health: a framework for public health law research. Milbank Q. 2010;88(2):169‐210. 10.1111/j.1468-0009.2010.00595.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Purtle J, Henson RM, Carroll‐Scott A, Kolker J, Joshi R, Diez Roux AV. US mayors’ and health commissioners’ opinions about health disparities in their cities. Am J Public Health. 2018;108(5):634‐641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pagel C, Bates DW, Goldmann D, Koller CF. A way forward for bipartisan health reform? Democrat and Republican State legislator priorities for the goals of health policy. Am J Public Health. 2017;107(10):1601‐1603. 10.2105/AJPH.2017.304023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niederdeppe J, Roh S, Dreisbach C. How narrative focus and a statistical map shape health policy support among state legislators. Health Commun. 2016;31(2):242‐255. 10.1080/10410236.2014.998913 [DOI] [PubMed] [Google Scholar]
- 6.Zhu JM, Chhabra M, Grande D. Concise research report: the future of Medicaid: state legislator views on policy waivers. J Gen Intern Med. 2018;33(7):999‐1001. 10.1007/s11606-018-4432-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Purtle J, Lê‐Scherban F, Wang X, Shattuck PT, Proctor EK, Brownson RC. Audience segmentation to disseminate behavioral health evidence to legislators: an empirical clustering analysis. Implement Sci. 2018;13:121. 10.1186/s13012-018-0816-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffman BL, Tulikangas MC, James AE, et al. Pennsylvania policymakers’ knowledge, attitudes and likelihood for action regarding waterpipe tobacco smoking and electronic nicotine delivery systems. Tob Prev Cessat. 2018;4:14. doi: 10.18332/tpc/89624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welch PJ, Dake JA, Price JH, Thompson AJ, Ubokudom SE. State legislators’ support for evidence‐based obesity reduction policies. Prev Med. 2012;55(5):427‐429. 10.1016/j.ypmed.2012.09.008 [DOI] [PubMed] [Google Scholar]
- 10.Purtle J, Lê‐Scherban F, Wang X, Brown E, Chilton M. State legislators’ opinions about adverse childhood experiences as risk factors for adult behavioral health conditions. Psychiatr Serv. 2019;70(10):894‐900. 10.1176/appi.ps.201900175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brownson RC, Dodson EA, Kerner JF, Moreland‐Russell S. Framing research for state policymakers who place a priority on cancer. Cancer Causes Control. 2016;27(8):1035‐1041. 10.1007/s10552-016-0771-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Guia NA, Cohen JE, Ashley MJ, et al. Support for tobacco control policies: how congruent are the attitudes of legislators and the public? Can J Public Health. 2003;94(1):36‐40. 10.1007/BF03405050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brownson RC, Dodson EA, Stamatakis KA, et al. Communicating evidence‐based information on cancer prevention to state‐level policy makers. J Natl Cancer Inst. 2011;103(4):306‐316. 10.1093/jnci/djq529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rutkow L, McGinty MD, Wetter S, Vernick JS. Local public health policymakers' views on state preemption: results of a national survey, 2018. Am J Public Health. 2019;109(8):1107‐1110. 10.2105/AJPH.2019.305140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dodson EA, Stamatakis KA, Chalifour S, Haire‐Joshu D, McBride T, Brownson RC. State legislators’ work on public health‐related issues: what influences priorities? J Public Health Manag Pract. 2013;19(1):25‐29. 10.1097/PHH.0b013e318246475c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Purtle J, Le‐Scherban FÉ, Wang XI, Shattuck PT, Proctor EK, Brownson RC. State legislators’ support for behavioral health parity laws: the influence of mutable and fixed factors at multiple levels. Milbank Q. 2019;97(4):1200‐1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pike Lacy AM, Eason CM, Stearns RL, Tosakoon S, Casa DJ. Legislators’ perceptions and knowledge of the athletic training profession: specific considerations for secondary schools. J Athl Train. 2019;54(11):1140‐1148. 10.4085/1062-6050-29-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robbins R, Niederdeppe J, Lundell H, Meyerson J. Views of city, county, and state policy makers about childhood obesity in New York State, 2010–2011. Prev Chronic Dis. 2013;10:E195. 10.5888/pcd10.130164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dodson EA, Fleming C, Boehmer TK, Haire‐Joshu D, Luke DA, Brownson RC. Preventing childhood obesity through state policy: qualitative assessment of enablers and barriers. J Public Health Policy. 2009;30(Suppl1):S161‐S176. 10.1057/jphp.2008.57 [DOI] [PubMed] [Google Scholar]
- 20.Rutkow L, Jones‐Smith J, Walters HJ, O'Hara M, Bleich SN. Factors that encourage and discourage policy‐making to prevent childhood obesity: experience in the United States. J Public Health Policy. 2016;37(4):514‐527. 10.1057/s41271-016-0035-y [DOI] [PubMed] [Google Scholar]
- 21.Gollust SE, Seymour JW, Pany MJ, Goss A, Meisel ZF, Grande D. Mutual distrust: perspectives from researchers and policy makers on the research to policy gap in 2013 and recommendations for the future. Inquiry. 2017;54:46958017705465. 10.1177/0046958017705465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jewell CJ, Bero LA. “Developing good taste in evidence”: facilitators of and hindrances to evidence‐informed health policymaking in state government. Milbank Q. 2008;86(2):177‐208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morshed AB, Dodson EA, Tabak RG, Brownson RC. Comparison of research framing preferences and information use of state legislators and advocates involved in cancer control, United States, 2012–2013. Prev Chronic Dis. 2017;14:160292. 10.5888/pcd14.160292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moreland‐Russell S, Barbero C, Andersen S, Geary N, Dodson EA, Brownson RC. “Hearing from all sides”: how legislative testimony influences state level policy‐makers in the United States. Int J Health Policy Manag. 2015;4(2):91‐98.doi: 10.15171/ijhpm.2015.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Purtle J, Langellier B, Lê‐Scherban F. A case study of the Philadelphia sugar‐sweetened beverage tax policymaking process: implications for policy development and advocacy. J Public Health Manag Pract. 2018;24(1):4‐8. 10.1097/PHH.0000000000000563 [DOI] [PubMed] [Google Scholar]
- 26.Gollust SE, Kite HA, Benning SJ, Callanan RA, Weisman SR, Nanney MS. Use of research evidence in state policymaking for childhood obesity prevention in Minnesota. Am J Public Health. 2014;104(10):1894‐1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Purtle J, Goldstein ND, Edson E, Hand A. Who votes for public health? US senator characteristics associated with voting in concordance with public health policy recommendations (1998–2013). SSM Popul Health. 2016;3:136‐140. 10.1016/j.ssmph.2016.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tung GJ, Vernick JS, Reiney EV, Gielen AC. Legislator voting and behavioral science theory: a systematic review. Am J Health Behav. 2012;36(6):823‐833. [DOI] [PubMed] [Google Scholar]
- 29.Yanovitzky I, Weber M. Analysing use of evidence in public policymaking processes: a theory‐grounded content analysis methodology. Evidence Pol. 2020;16(1):65‐82. [Google Scholar]
- 30.Woolf SH, Purnell JQ, Simon SM, et al. Translating evidence into population health improvement: strategies and barriers. Annu Rev Public Health. 2015;36:463‐482. 10.1146/annurev-publhealth-082214-110901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014;129(Suppl 2):5‐8. 10.1177/00333549141291S203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DuBois WE. The health and physique of the Negro American 1906. Am J Public Health. 2003;93(2):272‐276. 10.2105/ajph.93.2.272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams DR. Miles to go before we sleep: racial inequities in health. J Health Soc Behav. 2012;53(3):279‐295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adler NE, Glymour MM, Fielding J. Addressing Social determinants of health and health inequalities. JAMA. 2016;316(16):1641‐1642. 10.1001/jama.2016.14058 [DOI] [PubMed] [Google Scholar]
- 35.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750‐1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beckfield J, Krieger N. Epi+ demos+ cracy: linking political systems and priorities to the magnitude of health inequities—evidence, gaps, and a research agenda. Epidemiol Rev. 2009;31:152‐177. 10.1093/epirev/mxp002 [DOI] [PubMed] [Google Scholar]
- 37.Reeve B, Ashe M, Farias R, Gostin L. State and municipal innovations in obesity policy: why localities remain a necessary laboratory for innovation. Am J Public Health. 2015;105(3):442‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stone D. Health equity in a Trump administration. J Health Polit Policy Law. 2017;42(5):995‐1002. 10.1215/03616878-3940517 [DOI] [PubMed] [Google Scholar]
- 39.Farrer L, Marinetti C, Cavaco YK, Costongs C. Advocacy for health equity: a synthesis review. Milbank Q. 2015;93(2):392‐437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Academies of Sciences, Engineering, and Medicine . Communities in Action: Pathways to Health Equity. Washington, DC: National Academies Press; 2017. doi: 10.17226/24624. [DOI] [PubMed] [Google Scholar]
- 41.Benz JK, Espinosa O, Welsh V, Fontes A. Awareness of racial and ethnic health disparities has improved only modestly over a decade. Health Affairs. 2011;30(10):1860‐1867. [DOI] [PubMed] [Google Scholar]
- 42.Lundell H, Niederdeppe J, Clarke C. Public views about health causation, attributions of responsibility, and inequality. J Health Commun. 2013;18(9):1116‐1130. [DOI] [PubMed] [Google Scholar]
- 43.Booske BC, Robert SA, Rohan AM. Awareness of racial and socioeconomic health disparities in the United States: the national opinion survey on health and health disparities, 2008–2009. Prev Chronic Dis. 2011;8(4):A73. [PMC free article] [PubMed] [Google Scholar]
- 44.Bye L, Ghirardelli A, Fontes A. Promoting health equity and population health: how Americans’ views differ. Health Affairs. 2016;35(11):1982‐1990. [DOI] [PubMed] [Google Scholar]
- 45.Robert SA, Booske BC, Rigby E, Rohan AM. Public views on determinants of health, interventions to improve health, and priorities for government. WMJ. 2008;107(3):124‐130. [PubMed] [Google Scholar]
- 46.Niederdeppe J, Bu Q, Borah P, Kindig DA, Robert SA. Message design strategies to raise public awareness of social determinants of health and population health disparities. Milbank Q. 2008;86(3):481‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gollust SE, Cappella JN. Understanding public resistance to messages about health disparities. J Health Commun. 2014;19(4):493‐510. [DOI] [PubMed] [Google Scholar]
- 48.Young R, Hinnant A, Leshner G. Individual and social determinants of obesity in strategic health messages: interaction with political ideology. Health Commun. 2016;31(7):903‐910. [DOI] [PubMed] [Google Scholar]
- 49.Jones BD, Baumgartner FR. Representation and agenda setting. Pol Stud J. 2004;32(1):1‐24. [Google Scholar]
- 50.Kingdon JW, Thurber JA. Agendas, Alternatives, and Public Policies. Boston: Little, Brown; 1984. [Google Scholar]
- 51.McCombs ME, Shaw DL. The agenda‐setting function of mass media. Public Opin Q. 1972;36(2):176‐187. [Google Scholar]
- 52.Bromley‐Trujillo R, Salience Karch A., Scientific uncertainty, and the agenda‐setting power of science. Pol Stud J. 2020. 10.1111/psj.12373 [DOI] [Google Scholar]
- 53.Winburn J, Winburn A, Niemeyer R. Media coverage and issue visibility: state legislative responses to school bullying. Soc Sci J. 2014;51(4):514‐522. [Google Scholar]
- 54.Goldstein ND, Purtle J, Suder JS. Association of vaccine‐preventable disease incidence with proposed state vaccine exemption legislation. JAMA Pediatr. 2019;174(1):88–9. 10.1001/jamapediatrics.2019.4365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Boehmer TK, Luke DA, Haire‐Joshu DL, Bates HS, Brownson RC. Preventing childhood obesity through state policy: predictors of bill enactment. Am J Prev Med. 2008;34(4):333‐340. [DOI] [PubMed] [Google Scholar]
- 56.Eyler AA, Nguyen L, Kong J, Yan Y, Brownson R. Patterns and predictors of enactment of state childhood obesity legislation in the United States: 2006–2009. Am J Public Health. 2012;102(12):2294‐2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Niggel SJ, Robinson SB, Hewer I, Noone J, Shah S, Laditka SB. Adult obesity prevalence and state policymaking in the United States: is problem severity associated with more policies? Soc Sci J. 2013;50(4):565‐574. [Google Scholar]
- 58.Pomeranz JL, Siddiqi A, Bolanos GJ, Shor JA, Hamad R. Consolidated state political party control and the enactment of obesity‐related policies in the United States. Prev Med. 2017;105:397‐403. 10.1016/j.ypmed.2017.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rodriguez JM. Health disparities, politics, and the maintenance of the status quo: a new theory of inequality. Soc Sci Med. 2018;200:36‐43. 10.1016/j.socscimed.2018.01.010 [DOI] [PubMed] [Google Scholar]
- 60.Rodriguez JM. The politics hypothesis and racial disparities in infants’ health in the United States. SSM Popul Health. 2019;8:100440. 10.1016/j.ssmph.2019.100440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rodriguez JM, Geronimus AT, Bound J, Dorling D. Black lives matter: differential mortality and the racial composition of the US electorate, 1970–2004. Soc Sci Med. 2015;136:193‐199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bor J. Diverging life expectancies and voting patterns in the 2016 US presidential election. Am J Public Health. 2017;107(10):1560‐1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gollust SE, Haselswerdt J. Introduction health and political participation: advancing the field. J Health Polit Policy Law. 2019;44(3):341‐348. 10.1215/03616878-7366976 [DOI] [Google Scholar]
- 64.Rigby E, Soss J, Booske BC, Rohan AM, Robert SA. Public responses to health disparities: how group cues influence support for government intervention. Soc Sci Q. 2009;90(5):1321‐1340. [Google Scholar]
- 65.Lynch J, Gollust SE. Playing fair: fairness beliefs and health policy preferences in the United States. J Health Polit Policy Law. 2010;35(6):849‐887. 10.1215/03616878-2010-032 [DOI] [PubMed] [Google Scholar]
- 66.de Benedictis‐Kessner J, Warshaw C. Mayoral partisanship and municipal fiscal policy. J Politics. 2016;78(4):1124‐1138. [Google Scholar]
- 67.Barber BR. If Mayors Ruled the World: Dysfunctional Nations, Rising Cities. New Haven, CT: Yale University Press; 2013. [Google Scholar]
- 68.Rutkow L, McGinty MD, Wetter S, Vernick JS. Local public health policymakers’ views on state preemption: results of a national survey, 2018. Am J Public Health. 2019;109(8):1107‐1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fisher SH, Herrick R. Old versus new: the comparative efficiency of mail and internet surveys of state legislators. State Polit Policy Q. 2013;13(2):147‐163. [Google Scholar]
- 70.Tausanovitch C, Warshaw C. Measuring constituent policy preferences in congress, state legislatures, and cities. J Politics. 2013;75(2):330‐42. [Google Scholar]
- 71.American National Election Studies . The ANES Guide to Public Opinion and Electoral Behavior. Accessed December 12, 2020. https://electionstudies.org/resources/anes-guide.
- 72.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167‐194. [DOI] [PubMed] [Google Scholar]
- 73.Braveman PA, Kumanyika S, Fielding J, et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(Suppl 1):S149‐S155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Henson RM, McGinty M, Juliano C, Purtle J. Big City health officials’ conceptualizations of health equity. J Public Health Manage Pract. 2019;25(4):332‐341. [DOI] [PubMed] [Google Scholar]
- 75.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322(20):1996‐2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Health Inequality Project . Data. https://healthinequality.org/data. Accessed December 12, 2020.
- 77.Gourevitch MN, Athens JK, Levine SE, Kleiman N, Thorpe LE. City‐Level measures of health, health determinants, and equity to foster population health improvement: The City Health Dashboard. Am J Public Health. 2019;109(4):585‐592. 10.2105/AJPH.2018.304903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Arias E, Escobedo LA, Kennedy J, Fu C, Cisewski JA. U Arias E, Escobedo LA, Kennedy J, Fu C, Cisewki J.U.S. Small‐area Life Expectancy Estimates Project: methodology and results summary. Vital Health Stat 2. 2018;(181):1‐40. [PubMed] [Google Scholar]
- 79.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165(8):858‐867. [DOI] [PubMed] [Google Scholar]
- 80.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods, 2nd ed.Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 81.Tausanovitch C, Warshaw C. Representation in municipal government. Am Polit Sci Rev. 2014;108(3):605‐641. [Google Scholar]
- 82.Einstein KL, Kogan V. Pushing the city limits: policy responsiveness in municipal government. Urban Affairs Rev. 2016;52(1):3‐32. [Google Scholar]
- 83.Cuevas AG, Levine S, Purtle J. What predicts a mayoral official's opinion about the role of stress in health disparities? J Racial Ethn Health Disparities. 2020;7(1):109‐116. 10.1007/s40615-019-00639-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gerber ER, Hopkins DJ. When mayors matter: estimating the impact of mayoral partisanship on city policy. Am J Polit Sci. 2011;55(2):326‐339. [Google Scholar]
- 85.Mendez MF. A neurology of the conservative‐liberal dimension of political ideology. J Neuropsych Clin Neurosci. 2017;29(2):86‐94. [DOI] [PubMed] [Google Scholar]
- 86.Maio GR, Olson JM, Bernard MM, Luke MA. Ideologies, values, attitudes, and behavior. In: Delamater J, ed. Handbook of Social Psychology. Boston, MA: Springer; 2006:283‐308. [Google Scholar]
- 87.Jost JT, Federico CM, Napier JL. Political ideology: its structure, functions, and elective affinities. Annu Rev Psychol. 2009;60:307‐337. [DOI] [PubMed] [Google Scholar]
- 88.Kreuter MW, Farrell DW, Olevitch LR, Brennan LK. Tailoring Health Messages: Customizing Communication with Computer Technology. New York: Routledge; 2013. [Google Scholar]
- 89.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta‐analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673‐693. 10.1037/0033-2909.133.4.673. PMID: 17592961 [DOI] [PubMed] [Google Scholar]
- 90.Kim AE, Kumanyika S, Shive D, Igweatu U, Kim S‐H. Coverage and framing of racial and ethnic health disparities in US newspapers, 1996–2005. Am J Public Health. 2010;100(Suppl 1):S224‐S231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Niederdeppe J, Bigman CA, Gonzales AL, Gollust SE. Communication about health disparities in the mass media. J Commun. 2013;63(1):8‐30. [Google Scholar]
- 92.Hendrickson, C. Local journalism in crisis. Brookings. 2019. https://www.brookings.edu/wp-content/uploads/2019/11/Local-Journalism-in-Crisis.pdf. Accessed December 12, 2020.
- 93.Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the behavioral risk factor surveillance system. Am J Epidemiol. 2015;182(2):127‐137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhang X, Holt JB, Lu H, et al. Multilevel regression and poststratification for small‐area estimation of population health outcomes: a case study of chronic obstructive pulmonary disease prevalence using the behavioral risk factor surveillance system. Am J Epidemiol. 2014;179(8):1025‐1033. [DOI] [PubMed] [Google Scholar]
- 95.Štelemėkas M, Galkus L, Liutkutė Gumarov V, Goštautaitė Midttun N, Miščikienė L. Holding policy makers to account: monitoring voting patterns on alcohol and tobacco policy in the Lithuanian Parliament. Drug Alcohol Rev. 2019;39(7):827‐834. [DOI] [PubMed] [Google Scholar]
- 96.Young JL, Pollack K, Rutkow L. Review of state legislative approaches to eliminating racial and ethnic health disparities, 2002–2011. Am J Public Health. 2015;105(Suppl 3):S388‐S394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gollust SE, Vogel RI, Rothman A, Yzer M, Fowler EF, Nagler RH. Americans' perceptions of disparities in COVID‐19 mortality: Results from a nationally‐representative survey. Preventive Medicine. 2020. Dec 1;141:106278. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Table A. Characteristics of Cities Governed by Survey Respondents and Nonrespondents
Appendix Table B. Correlations Between the Measure of City Health Disparity Used for the Analysis and Other Publicly Available Measures of Health Disparities in US Cities
Appendix Table C. Sensitivity Analysis: Odds of Mayoral Official Strongly Agreeing That Health Disparities Exist in Their City Given the Magnitude of Life Expectancy Disparitya per $10,000 of Income, z score standardized
Appendix Table D. Sensitivity Analysis: Odds of Mayoral Official Believing That Health Disparities in Their City Are Very Unfair (Compared to Fair) Given the Magnitude of Life Expectancy Disparitya per $10,000 income, z score standardized
Supporting Material


