Abstract
Introduction and importance
Gossypiboma or textiloma is a mass comprising of cotton matrix within the body left accidentally during a surgical procedure. The body may react to this foreign body through an exudative inflammatory reaction or an aseptic fibrotic reaction in order to encapsulate the cotton material and result into a mass.
Case presentation
We report a case of 65-year-old female. She was referred to our department due to 2 episodes of nausea and vomiting. She had history of open cholecystetomy 29 years ago, then cure for eventration one year after. On exploratory laparotomy there was a mass measuring 6 cm axis at the expense of segment 3 of the liver coming into intimate contact with the duodenum. Atypical segmental hepatectomy of segment 3 of liver was performed, and the histological report confirmed necrotic textiloma.
Clinical discussion
Textiloma represents a complication of all forms of surgery. It is a real, serious but preventable surgical complication, and could present with various complaints. Prevention of this condition can be achieved by meticulous count of surgical materials.
Conclusion
The embarrassment faced by the surgeon and the medico legal implications of this iatrogenic complication are tremendous and all preventive measures should be taken to avoid this as no excuse is justifiable.
Keywords: Gossypiboma, Textiloma, Laparotomy, Medicolegal, Case report
Highlights
-
•
Gossypiboma is a mass comprising of cotton matrix within the body left accidentally during a surgical procedure.
-
•
Gossypiboma is a serious but avoidable complication.
-
•
It has serious medicolegal implications and negative impact on medical fraternity.
-
•
Surgical and nursing team should be careful and ensure counts of surgical items during and at the end of surgery.
1. Introduction and importance
This work has been reported in line with the SCARE 2020 criteria [1]. Gossypiboma or textiloma is a mass comprising of a cotton matrix within the body left accidentally during a surgical procedure. The body may react to this foreign body through an exudative inflammatory reaction or an aseptic fibrotic reaction in order to encapsulate the cotton material and result into a mass [2].
This iatrogenic, unintentional but avoidable misfortune, often under-reported, has damaging effects upon the health of patients, and entails embarrassment as well as medico-legal consequences [3,4].
It is estimated that retained surgical foreign bodies occur one in every 5500–18,760 in patient operations but the incidence may be as high as one out of every 1000–1500 abdominal cavity operations, and even more common during emergency surgeries [5].
2. Case presentation
Patient was 65-year-old female, was referred to our department due to 2 episodes of nausea and vomiting for no clear reason, loss of appetite and weight loss estimated at 8 kg during 1 year.
In the past, the patient had open cholecystetomy 29 years ago, then cure for eventration one year after, but no documentation was available. The patient had no history of alcohol or drug abuse, and she didn't have any adverse reaction of medication.
We didn't have enough information in order to know family history including any relevant genetic issue.
On examination, she was afebrile, with normal respiratory rate and normal resting heart rate. Per abdomen examination revealed a midline vertical scar indicative of previous surgery, without palpable masses. Digital rectal exam and digital examination of the vagina were normal.
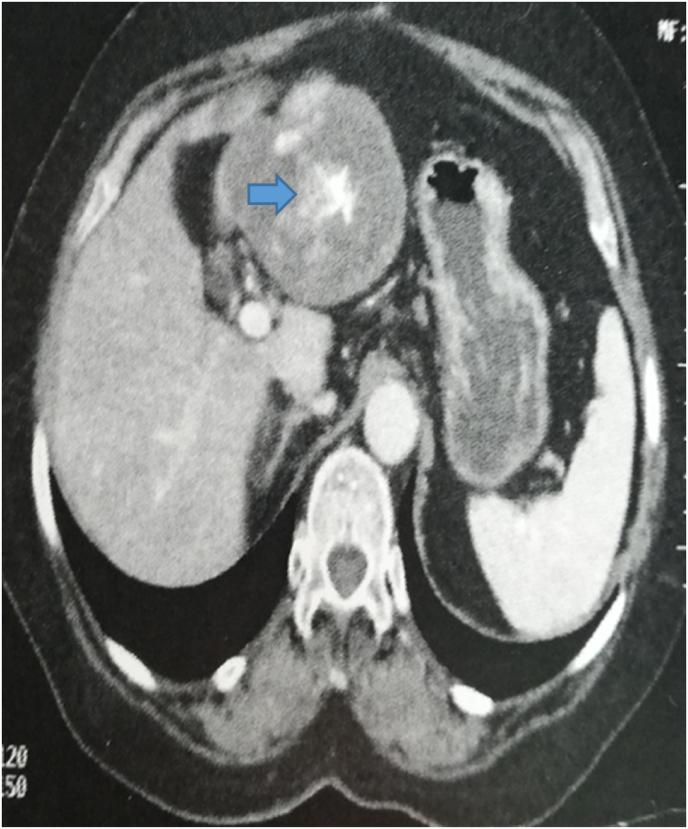
Eso-gastro-duodenal fibroscopy revealed: extrinsic compression of the lesser curvature on an erythematous mucosa (Fig. 1). The Biopsy showed a mixed dense lymphoid infiltrate (T and B) which is difficult to label in this sampling. Abdominal CT scann: evidence of heterogeneous formation connecting with the duodenum, this mass comes into intimate contact at the top with the left liver, with disappearance of the separation border, it is the site of multiple parietal and central calcifications, its site appears duodenal, this aspect is suggestive of a GIST (Fig. 2). Thoracic CT scann didn't show any secondary lesions. CA 19-9 slightly raised to 48,50 U/ml, and ACE was normal at 1,70 ng/ml.
Fig. 1.
Fibroscopy shows extrinsic compression of the lesser curvature.
Fig. 2.
Heterogenous formation which suggest a GIST (blue arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Preanesthesic assessment was done by an anesthesia provider.
Patient was performed by two Professors with superior 20 years of experience in the field of general surgery and was assissted by three junior residents, in the university hospital center.
The patient gave her approval to do surgery, especially for tumor ablation.
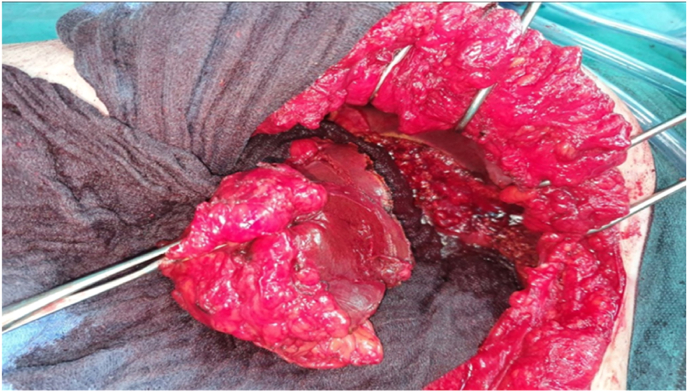
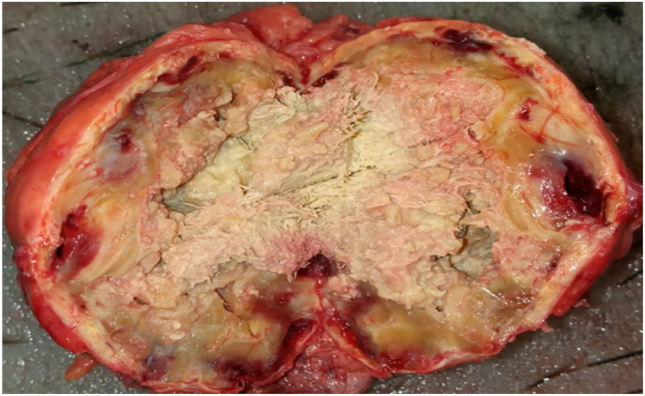
During laparotomy under general anesthesia, the exploration showed the presence of an irregular contour mass measuring 6 cm axis at the expense of segment 3 of the liver coming into intimate contact with the duodenum (genu superius). We proceed to release of the mass from the duodenum with biopsies of the duodenal edges and atypical segmental hepatectomy of segment 3 of liver after kellyclasia (Fig. 3). The abdomen was closed with all precautions and counts of surgical items. The materiel was recognized after incision of the mass as a surgical sponge (Fig. 4). Histological report confirmed necrotic textiloma.
Fig. 3.
Atypical segmental hepatectomy of segment 3 of liver.
Fig. 4.
The materiel after incision of the mass.
After 6 hours of surgery, the patient was extubated. However, on postoperative day 3 the patient presented respiratory distress for which we realised thoraco-abdominal CT showing lesion related to infection lung (treated by ATB). She was transferred to an intensive care unit where she was intubated, ventilated with hypotension at 8/4 tachycardia at 124. The patient died on postoperative day 10 following an unrecovered cardio-respiratory arrest despite the resuscitation measures.
3. Clinical disscusion
A surgical sponge that is inadvertently left in a surgical wound eventually develops into a textiloma [6]. Strictly speaking, the term ‘‘textiloma’’ should be reserved only for a surgical sponge consisting of organic material. Indeed, ‘‘gossypiboma’’ is the term used to describe a mass within the body that comprises a cotton matrix surrounded by a foreign-body reaction like our CASE [6]. However, these days, synthetic material has replaced cotton, so the definition of a textiloma and gossypiboma need to be adapted. The incidence of retained foreign bodies following surgery varies from 0.01% to 0.001% [1,6,7]. Of these cases, 80% are gossypibomas [6].
Textiloma represents a complication of all forms of surgery: abdominal (52%); gynecological (22%); urological and vascular (10%); orthopedic and spinal (6%) [5]. Olnick et al. [7] has further classified textilomas into acute necrotic forms and chronic forms. The acute form, in which an exudative reaction dominates the clinical picture, along with abscess formation and skin fistulas, is symptomatic in the early postoperative period. The differential diagnosis in such cases includes postoperative collection, hematoma and non foreign-body abscess. In the chronic form, as seen in our patient, adhesions and encapsulation eventually lead to the development of a foreign-body granuloma. Asymptomatic forms are sometimes discovered fortuitously. A delayed presentation may be seen months or even years after the initial surgery. Our patient was referred to us with episode of nausea and vomiting for no clear reason and loss of appetite and weight loss, 29 years after the primary operation. Adhesions and encapsulation are common features of gossypiboma, and the lesion may present as a mass. In such cases, the differential diagnosis typically includes tumors [6]. The exudative type of gossypiboma causes symptoms earlier than does the fibrinous type [6].
Such foreign bodies are often discovered long after surgery and may present with non-specific clinical symptoms. The imaging appearance of textilomas is not widely known and they can often be mistaken for a soft-tissue tumor [8].
The radiological diagnosis of textiloma is easily made by plain abdominal radiography, when a radio-opaque marker is seen. However, these markers could disintegrate or fragment over years after the surgery [9].
This diagnostic doubt led to an abdominal ultrasound and a CT scan. Ultrasound is useful in the diagnosis of abdominal retained gauze. Ultrasound features are usually a well delineated mass containing an wavy internal echo with a hypoechoic ring and strong posterior acoustic shadowing. CT is the technique of choice for detecting gossypibomas and possible complications. Many authors consider a gossypiboma to be specifically indicated by a CT finding of a low-density heterogeneous mass with an external highdensity wall that is further highlighted on contrast-enhanced imaging and that has a spongiform pattern containing air bubbles [10].
But in our scenario the surgical swab retained in our patient as a heterogeneous formation specially like gastro intestinal stromal tumor, and this was attributed to the nature of the surgical gauze, the different foreign-body reaction, and the quantity of fluid and protein associated with the lesion.
Though the diagnosis of left out foreign body can be made by taking careful history, clinical examinations and by doing some necessary investigations. Yet some patients are diagnosed on the operating table during re-laparotomy. Surgical exploration is the answer to the problem [11]. In 2003, Gawande and colleagues [4] described the most common risk factors associated with “retained foreign bodies” are-emergency operations, unplanned changes in operating procedures. The prevention of this condition can be achieved by meticulous count of surgical materials in addition to thorough exploration of surgical site at the conclusion of operations and also by routine use of surgical textile materials impregnated with a radio opaque marker that are easily detected by intraoperative radiological screening when the countis suspicious.
4. Conclusion
Gossypiboma is serous but avoidable, postoperative complication. It must be prevented at all costs. The embarrassment faced by the surgeon and the medico legal implications of this iatrogenic complication are tremendous and all preventive measures should be taken to avoid this as no excuse is justifiable.
Sources of funding
The authors declared that this study has received no financial support.
Author contribution
Amal Hajri: written the paper.
Kenza Benjelloun Touimi: corresponding author writing the paper.
Yassine El Berni: written the paper.
Driss Erguibi: study concept.
Rachid Boufettal: study concept.
Saad Rifki Jai: correction of the paper.
Farid Chehab: correction of the paper.
Guarantor
KENZA BENJELLOUN TOUIMI.
Consent
Consent to publish the CASE report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Ethical approval
I declare on my honor that the ethical approval has been exempted by my establishment.
Patient Consent
Consent to publish the CASE report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The authors declare having no conflicts of interest for this article.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the Scare Group The SCARE 2020 guideline: updating consensus surgical CASE REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Gibbs V.C., Coakley F.D., Reines H.D. Preventable errors in the operating room: retained foreign bodies after surgery—Part I. Curr. Probl. Surg. 2007;44(5):281–337. doi: 10.1067/j.cpsurg.2007.03.002. mai. [DOI] [PubMed] [Google Scholar]
- 3.Stawicki S.P., Evans D.C., Cipolla J., Seamon M.J., Lukaszczyk J.J., Prosciak M.P. Retained surgical foreign bodies: a comprehensive review of risks and preventive strategies. Scand J. Surg. 2009;98(1):8–17. doi: 10.1177/145749690909800103. mars. [DOI] [PubMed] [Google Scholar]
- 4.Gawande A.A., Studdert D.M., Orav E.J., Brennan T.A., Zinner M.J. Risk factors for retained instruments and sponges after surgery. N Engl. J. Med. 2003;348(3):229–235. doi: 10.1056/NEJMsa021721. 16 janv. [DOI] [PubMed] [Google Scholar]
- 5.Sonarkar R., Wilkinson R., Nazar Z., Gajendra G., Sonawane S. Textiloma presenting as a lump in abdomen: a CASE report. Int. J. Surg. Case Rep. 2020;77:206–209. doi: 10.1016/j.ijscr.2020.10.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim H.S., Chung T.-S., Suh S.H., Kim S.Y. MR imaging findings of paravertebral gossypiboma. AJNR Am. J. Neuroradiol. 2007;28(4):709–713. avr. [PMC free article] [PubMed] [Google Scholar]
- 7.Olnick H.M. Radiological diagnosis OF retained surgical sponges. J. Am. Med. Assoc. 1955;159(16):1525. doi: 10.1001/jama.1955.02960330025008. 17 déc. [DOI] [PubMed] [Google Scholar]
- 8.Rasoaherinomenjanahary F., Ranoharison D.H., Samison L.H. Abdominal foreign body textiloma: imaging and operative appearance. J. Visc. Surg. 2017;154(6):463–465. doi: 10.1016/j.jviscsurg.2017.08.002. déc. [DOI] [PubMed] [Google Scholar]
- 9.Hammadieh A.R., Alsabek M.B., Rustom S. Textiloma mimicking Crohn's disease in its features: a CASE report. Ann Med Surg. févr. 2021;62:283–287. doi: 10.1016/j.amsu.2021.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdominal Textiloma Mimicking as Left Colic Tumour: A Postoperative Complication Still Common in Low-Income Countries. EMJ Radiol [Internet]. 1 sept 2020 [cite 3 juill 2021]; Disponible sur: https://www.emjreviews.com/radiology/abdominal-textiloma-mimicking-as-left-colic-tumour-a-postoperative-complication-still-common-in-low-income-countries.
- 11.Robinson K.B., Levin E.J. Erosion OF retained surgical sponges into the intestine. Am. J. Roentgenol. 1966;96(2):339–343. doi: 10.2214/ajr.96.2.339. févr. [DOI] [PubMed] [Google Scholar]