Abstract
This cross-sectional study characterizes prehospital large vessel occlusion transport algorithms across the US.
Prehospital triage is critically important in the care of patients with stroke caused by large vessel occlusion (LVO), both because of the time-sensitive nature of acute interventions and the need to appropriately use available resources.1 However, it is unclear if standardized LVO-specific triage protocols exist among emergency medical services (EMS) nationwide.
Methods
We performed a cross-sectional analysis of publicly available statewide EMS protocols in December 2020 using online searches cross-referenced to previous literature2 to characterize prehospital LVO transport algorithms across the US. We included states with mandated or recommended protocols as well as those with relevant state department of health–issued guidelines. Other states were excluded, even if they had protocols on a regional level.
After identifying 35 states with publicly available adult stroke EMS protocols, we determined the frequency of LVO-specific transport algorithms, use of LVO screening tools, criteria for determining transport to an alteplase-capable center (ACC) vs a thrombectomy-capable center (TCC), and specific time-based cutoffs considered in transport decision-making (ie, time from last known well and maximum acceptable delay to bypass an ACC for a TCC). All protocols were independently reviewed by C.C.C. and T.J.M., and there were no cases of disagreement.
Results
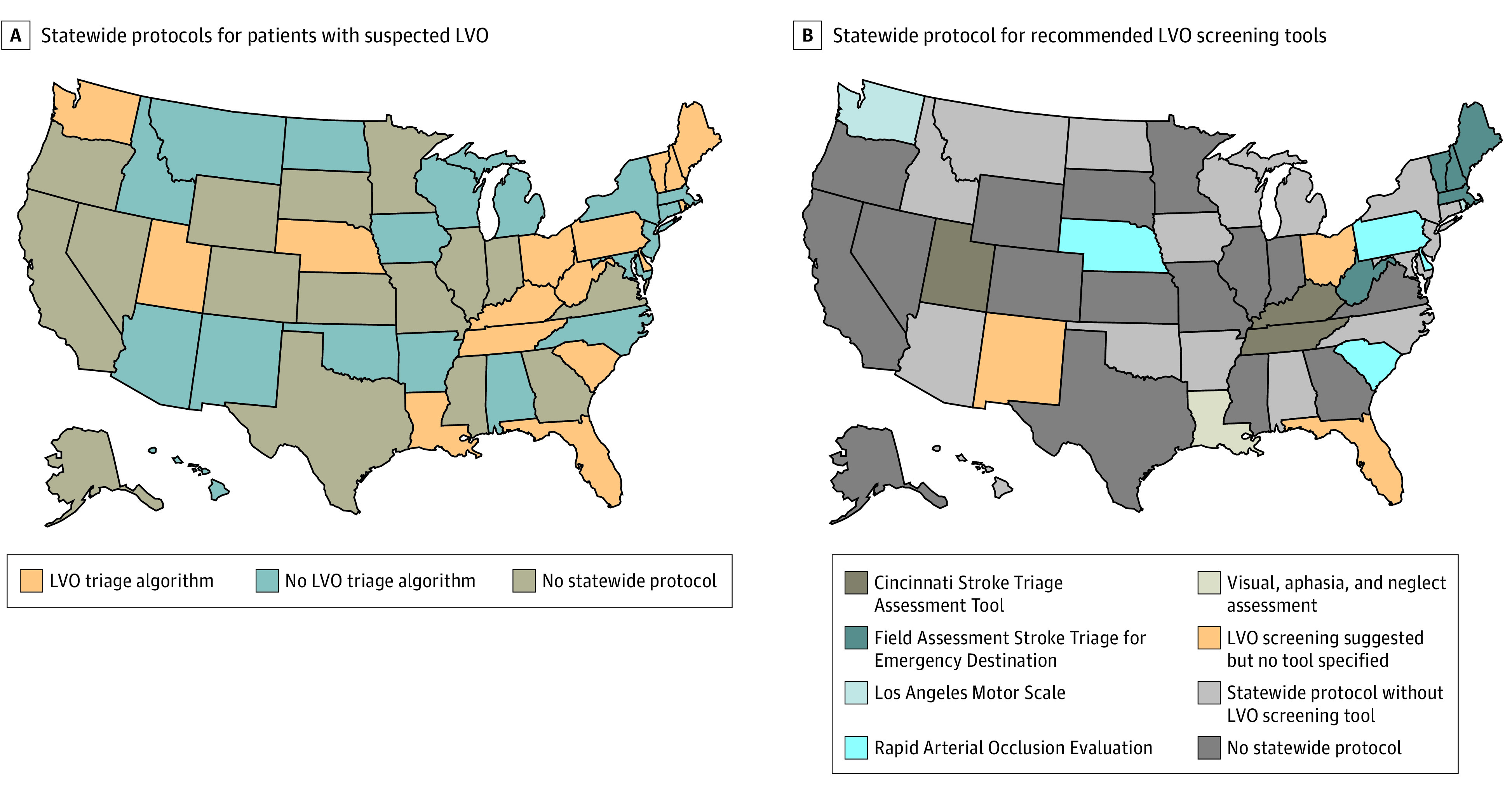
Only 16 states included specific transport considerations addressing suspected LVO cases, with 5 others suggesting following regional algorithms (Figure). Five different LVO screening tools were recommended: Rapid Arterial Occlusion Exam (RACE; 4 states), Field Assessment Stroke Triage for Emergency Destination (FAST-ED; 4 states), Cincinnati Stroke Triage Assessment Tool (C-STAT; 3 states), Los Angeles Motor Scale (LAMS; 2 states), and visual, aphasia, and neglect assessment (VAN; 1 state). Two states did not specify an LVO screening tool.
Figure. Map Depicting Available Statewide Protocols, Including Triage Algorithms for Patients With Suspected Large Vessel Occlusion (LVO) and Recommended LVO Screening Tools.
Among the 16 states with LVO transport algorithms, 9 recommended bypassing ACCs in favor of TCCs for potentially alteplase-eligible patients, while 6 recommended transport of alteplase-eligible patients to the nearest ACC and alteplase-ineligible patients to a TCC; 1 state defers transportation decisions of alteplase-eligible patients to potential receiving hospitals (Table). Among states that recommended bypassing ACCs for TCCs, 7 did not indicate a maximum acceptable transportation delay, while the others allowed maximum delays ranging from 15 to 60 minutes. Three states (Kentucky, Nevada, and West Virigina) explicitly prioritized comprehensive stroke centers over other TCCs, and 5 states (Iowa, Idaho, Nevada, Washington, and West Virginia) suggested air medical transport to expedite hospital arrival.
Table. Summary of Large Vessel Occlusion (LVO)–Specific Algorithms in Available Statewide Emergency Medical Services Protocols.
| State | Year updated | Type | LVO transport destination algorithm | Recommended LVO screening tool | Recommended transport destination by LKW | Maximum allowable added transport time to bypass for a TCC | No. | |||
|---|---|---|---|---|---|---|---|---|---|---|
| ASRHs | PSCs | Non-CSC TCCs | CSCs | |||||||
| Alabama | 2020 | Mandatory | No | NA | NA | NA | 42 | 21 | 0 | 3 |
| Arkansas | 2018 | Recommended | No | NA | NA | NA | 1 | 4 | 0 | 2 |
| Arizona | 2019 | Recommended | Defers to local protocol | NA | NA | NA | 0 | 16 | 1 | 2 |
| Connecticut | 2020 | Mandatory | Defers to local protocol | NA | NA | NA | 1 | 20 | 1 | 2 |
| Washington, DC | 2017 | Mandatory | No | NA | NA | NA | 0 | 2 | 0 | 3 |
| Delaware | 2020 | Mandatory | Yes | RACE | 0-4.5 h: Contact Medical Controla; 4.5-24 h: TCC | None | 0 | 1 | 0 | 1 |
| Florida | 2019 | Statewide stroke initiative | Yes | Not specified | 0-24 h: TCC | Based on total transport timeb | 2 | 102 | 0 | 50 |
| Hawaii | 2018 | Mandatory | No | NA | NA | NA | 0 | 7 | 0 | 1 |
| Iowa | 2018 | Recommended | No | NA | NA | NA | 85 | 18 | 0 | 1 |
| Idaho | 2020 | Recommended | No | NA | NA | NA | 7 | 4 | 0 | 2 |
| Kentucky | 2020 | Recommended | Yesc | C-STAT | 0-3 h: ACC; 3-24 h: TCCd | None | 13 | 19 | 0 | 4 |
| Louisiana | 2020 | Statewide stroke initiative | Yes | VAN | 0-6 h: TCC; 6-24 h: ACC | 15 min | 56 | 13 | 6 | 3 |
| Massachusetts | 2019 | Mandatory | Defers to local protocol | FAST-ED | NA | NA | 60e | 6e | ||
| Maryland | 2020 | Mandatory | No | NA | NA | NA | 0 | 36 | 0 | 3 |
| Maine | 2019 | Mandatory | Yes | FAST-ED | 0-3 h: ACC; 3-24 h: TCC | 30 min | 1 | 3 | 0 | 1 |
| Michigan | 2018 | Recommended | No | NA | NA | NA | 1 | 27 | 3 | 11 |
| Montana | 2019 | Recommended | No | NA | NA | NA | 5 | 25 | 2 | 6 |
| North Carolina | 2020 | Recommended | No | NA | NA | NA | 9 | 35 | 2 | 10 |
| North Dakota | 2016 | Recommended | Defers to local protocol | NA | NA | NA | 30 | 3 | 1 | 2 |
| Nevada | 2020 | Recommended | Yesc | RACE | 0-6 h: TCC; 6-24 h: ACC | 15 min | 2 | 12 | 1 | 1 |
| New Jersey | 2013 | Field guide | No | NA | NA | NA | 0 | 51 | 0 | 15 |
| New Mexico | 2018 | Recommended | No | Not specified | NA | NA | 1 | 6 | 0 | 0 |
| New Hampshire | 2018 | Mandatory | Yes | FAST-ED | 0-4.5 h: ACC; 4.5-24 h: TCC | None | 0 | 5 | 0 | 0 |
| New York | 2019 | Recommended | Defers to local protocol | NA | NA | NA | 0 | 106 | 1 | 16 |
| Ohio | 2018 | Recommended | Yesf | Defer to local protocol | 0-6 h: TCC; 6-24 h: ACC | 15 min | 7 | 60 | 0 | 11 |
| Oklahoma | 2018 | Recommended | No | NA | NA | NA | 1 | 5 | 0 | 2 |
| Pennsylvania | 2020 | Mandatory | Yes | mRACE | 0-3 h: ACC; 3-24 h: contact Medical Controld,g | None | 18 | 92 | 2 | 15 |
| Rhode Island | 2020 | Mandatory | Yesf | LAMS | 0-24 h: TCC | None | 1 | 7 | 0 | 1 |
| South Carolina | 2019 | Mandatory | Yes | RACE | 0-24 h: TCC | 60 min | 18 | 24 | 0 | 4 |
| Tennessee | 2018 | Recommended | Yes | C-STAT | 0-24 h: TCC | None | 4 | 19 | 0 | 7 |
| Utah | 2020 | Recommended | Yes | C-STAT | 0-4 h: ACC; 4-24 h: TCC | 30 min | 0 | 9 | 0 | 2 |
| Vermont | 2020 | Mandatory | Yes | FAST-ED | 0-4.5 h: ACC; 4.5-24 h: TCC | Based on total transport timeb | 0 | 1 | 0 | 0 |
| Washington | 2019 | Statewide stroke initiative | Yes | LAMS | 0-24 h: TCC | LKW<6 h: 15 min; LKW>6 h: 30 min | 45 | 28 | 4 | 8 |
| Wisconsin | 2019 | Recommended | No | NA | NA | NA | 4 | 41 | 0 | 4 |
| West Verginia | 2020 | Mandatory | Yesc | FAST-ED | 0-24 h: TCC | 45 min | 2 | 4 | 1 | 2 |
Abbreviations: ACC, alteplase-capable center; ASRH, acute stroke-ready hospital; CSC, comprehensive stroke center; C-STAT, Cincinnati Stroke Triage Assessment Tool; FAST-ED, Field Assessment Stroke Triage for Emergency Destination; LAMS, Los Angeles Motor Scale; LKW, last known well; mRACE, modified Rapid Arterial Occlusion Evaluation; NA, not applicable; PSC, primary stroke center; RACE, Rapid Arterial Occlusion Evaluation; TCC, thrombectomy-capable center; VAN, visual, aphasia, and neglect assessment.
Medical Control contacted in all cases of LKW within 0 to 4.5 hours.
Recommends transport to TCC if within 60 minutes of total transport time.
Prioritizes CSC within range above non-CSC TCC.
LKW specific to hospital arrival.
Designates 66 primary stroke service centers on their state department of health website, of which 6 are CSCs.
Prioritizes CSC; does not mention TCC.
Medical Control contacted only for consideration of bypass.
Discussion
According to a recent consensus statement, it is now recommended that patients with suspected LVO should be preferentially triaged to a TCC if within a certain range, depending on geographical setting.3,4 Specific prehospital procedures to identify such patients are also recommended. Nevertheless, our study found that most states do not have specific prehospital guidelines on the transport of patients with suspected LVO and that there is substantial variability in the states that do have such protocols.
Part of this variability may be because of the relatively unreliable nature of existing LVO screening tools,5 although they may still improve outcomes with appropriate training and implementation. Our study also found substantial variability in last known well cutoffs and acceptable destination delays for suspected LVO cases, some of which conflict with American Heart Association recommendations.3 Given the importance of EMS triage in the early care of patients with stroke,6 there is an urgent need for pragmatic trials to determine optimal prehospital LVO triage practices.
Because our study was limited to states with uniformly adopted guidelines, we may have undercounted protocols in the remaining states in which guidelines are adopted heterogeneously at the county or local level. Additionally, regional differences in health care infrastructure and resource availability may have impacted specific protocols and their implementation. Finally, we were unable to determine adherence to published protocols and real-world prehospital triage practices, which should be addressed in future studies using available EMS tracking databases.
References
- 1.Saver JL, Goyal M, van der Lugt A, et al. ; HERMES Collaborators . Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316(12):1279-1288. doi: 10.1001/jama.2016.13647 [DOI] [PubMed] [Google Scholar]
- 2.Kupas DF, Schenk E, Sholl JM, Kamin R. Characteristics of statewide protocols for emergency medical services in the United States. Prehosp Emerg Care. 2015;19(2):292-301. doi: 10.3109/10903127.2014.964891 [DOI] [PubMed] [Google Scholar]
- 3.American Heart Association. Mission: Lifeline Stroke. Accessed November 8, 2020. https://www.heart.org/en/professional/quality-improvement/mission-lifeline/mission-lifeline-stroke
- 4.Jauch EC, Schwamm LH, Panagos PD, et al. ; Prehospital Stroke System of Care Consensus Conference . Recommendations for regional stroke destination plans in rural, suburban, and urban communities from the Prehospital Stroke System of Care Consensus Conference: a consensus statement from the American Academy of Neurology, American Heart Association/American Stroke Association, American Society of Neuroradiology, National Association of EMS Physicians, National Association of State EMS Officials, Society of NeuroInterventional Surgery, and Society of Vascular and Interventional Neurology: endorsed by the Neurocritical Care Society. Stroke. 2021;52(5):e133-e152. doi: 10.1161/STROKEAHA.120.033228 [DOI] [PubMed] [Google Scholar]
- 5.Smith EE, Kent DM, Bulsara KR, et al. ; American Heart Association Stroke Council . Accuracy of prediction instruments for diagnosing large vessel occlusion in individuals with suspected stroke: a systematic review for the 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke. Stroke. 2018;49(3):e111-e122. doi: 10.1161/STR.0000000000000160 [DOI] [PubMed] [Google Scholar]
- 6.US Centers for Disease Control and Prevention . What is the evidence for existing state laws to enhance pre-hospital stroke care? Accessed May 6, 2021. https://www.cdc.gov/dhdsp/pubs/docs/Stroke-PEAR-508.pdf


