Abstract
Objectives
The purpose of this randomized clinical trial was to compare the required time of potential clinical adjustments of posterior screw‐retained monolithic zirconia implant retained crowns based on intraoral optical scanning (IOS) or conventional impressions.
Materials and methods
Patients with posterior tissue level implants (Straumann RN) replacing solitary teeth were recruited. Of all patients, impressions were taken with both an IOS (3M™ TDS) and a conventional (polyether) pick‐up impression. Randomization was performed after impression taking and patients were to receive either a crown based on the digital or the conventional impression. The time required for adjustments at placement was recorded. Additionally, restoration survival and mechanical complications with a follow‐up of one year were documented.
Results
Thirty two patients with 45 implants were included: 23 restorations in the test (IOS) and 22 in the control (conventional) group. The average adjustment time was 3.35 min (SD ± 3.38, range: 0–11 min) for the digital versus 6.09 min (SD ± 4.63, range: 0–18 min) for the conventional impressions (p = .039). A proper fit (no adjustments required) was achieved 39,1% in the digital and 18,2% conventional group respectively. All 45 restorations could be placed within the two planned appointments and only two minor mechanical complications occurred during the first year of function.
Conclusions
The use of IOS resulted in shorter adjustment times at try‐in than conventional impressions for solitary CAD/CAM implant restorations. Screw‐retained solitary monolithic zirconia restorations on ti‐base abutments show low complication‐ and survival rates in the short term.
Keywords: CAD/CAM, digital impression, digital workflow, implant, intraoral optical scanning, monolithic, ti‐base, zirconia
1. INTRODUCTION
The use of CAD/CAM technology to produce dental restorations is widely applied and considered daily routine in many dental laboratories (Alves de Carvalho et al., 2018; Wittneben et al., 2009). The introduction of intraoral optical scanning (IOS) has made these workflows even more efficient since the data—necessary to create a digital design (CAD)—is directly available (Zimmermann et al., 2015). For restorations on dental implants the application of CAD/CAM technologies is even more beneficial since—in contrary to the preparations on a natural tooth—the shape of an implant or selected abutment is standardized for various implant types and can be considered known. This means that only the relative position of an implant and not the exact shape needs to be obtained in order to design a corresponding restoration. For implant restorations, CAD/CAM was initially mainly used for the production of abutments, (metal) bars or (oxide) copings used to be veneered with porcelain or acrylic. With the introduction of monolithic ceramic CAD/CAM materials, it became possible to design full‐contour ceramic implant restorations (Joda & Bragger, 2014). It is known that ceramic veneering materials exhibit high complication rates, especially when used on dental implants (Pjetursson et al., 2014). Therefore, in addition to the improved production efficacy, a possible advantage of these monolithic restorations is that due to improved strength, chipping or fracture is less likely to occur (Joda, Ferrari., 2017). With respect to flexural strength, monolithic zirconia is currently the strongest ceramic material available in dentistry (Kwon et al., 2018). Although the hardness of the material has its benefits in relation to chipping or fractures, there are concerns about the wear of the opposing dentition. Nonetheless, polished monolithic zirconia is the least abrasive restorative material available (Burgess et al., 2014; Preis et al., 2011, 2012; Rosentritt et al., 2012).
These monolithic CAD/CAM implant restorations are completely designed and produced with computerized processes dedicated to specific abutments available in the libraries of dental technician software. These so‐called ti‐base abutments are nowadays available for most implants and a cost‐effective and efficient option for the application in the digital workflow (Joda & Bragger, 2014).
To date, most studies related to these digital workflows have focused on the theoretical accuracy of certain aspects of the procedure, such as the comparison of digital versus conventional impressions in vitro (Alikhasi et al., 2018, Flugge et al., 2016; Vandeweghe et al., 2016). Many authors have concluded that especially longer inter‐implant distances may lead to larger deviations (Gimenez‐Gonzalez et al., 2016; van der Meer et al., 2012). Nevertheless, for solitary implant restorations some authors suggest that the use of IOS is suitable (Lee & Gallucci, 2012). Clinical data to support this—nowadays widely applied—fully digital workflow for solitary implant restorations is limited (De Angelis et al., 2020; Joda, Zarone, et al., 2017). Especially the benefit of applying IOS in comparison to conventional impressions to create these CAD/CAM monolithic restorations has not been documented in clinical trials yet.
Therefore, the objective of this randomized controlled clinical trial is to compare the required time of potential clinical adjustments at placement of posterior CAD/CAM monolithic zirconia screw‐retained solitary implant crowns luted on ti‐base abutments made based on either intraoral scanning or conventional impression techniques.
2. MATERIALS AND METHODS
2.1. Patient selection
The study was designed as a randomized controlled clinical trial. The test group comprises of restorations based on IOS, the control group restorations are based on conventional impressions. All patients were recruited at the department of Oral Implantology and Prosthetic Dentistry at ACTA, Academic Center for Dentistry Amsterdam. The study protocol was approved by the regional ethical committee of VU‐Medical Center, Amsterdam, the Netherlands (No. 2013‐152NL43489.029.13). Patients provided written informed consents with permission to use their data for scientific purposes. All patient treatments were performed by the same clinician (WD). The study followed the CONSORT 2010 guidelines.
Patients were included based on the following inclusion criteria: (1) Partially edentulous adults. (2) Having at least one osseointegrated Straumann tissue level implant with an RN prosthetic connection to replace a solitary missing tooth in the posterior area. (3) The missing tooth location (future restoration) had at least one antagonist (4) Stable medical condition to undergo implant therapy (ASA 1 or 2), smokers were not excluded. Exclusion criteria were: (1) Signs of inflammation or peri‐implant diseases at the time of implant impressions. (2) Implants that would not allow straight occlusal screw access within the contours of the future implant crown. (3) Patients with known allergies to any of the used prosthetic components.
2.2. Impression phase
All patients underwent the same initial procedure since randomization was performed after the final impressions (Figure 1). First, an alginate impression (Impressional NS, Cavex Holland BV) of the implanted jaw was obtained to create an individual impression tray (Lightplast base plate, Dreve Dentamid GmbH) for a pick‐up impression. After one week the definitive impressions were made. All patients underwent a digital and a conventional impression procedure. First, the digital impression was obtained: the healing cap was removed, a brand‐specific scan abutment (Straumann CARES RN Mono Scanbody) was screwed on the implant with 10 Ncm (Figure 2). Subsequently, a thin layer of scan powder (3 M High‐Resolution Scanning Spray) was applied and a full‐arch IOS was obtained using the True Definition Scanner (3 M). Also a scan of the opposing arch, and left and right bite scan in maximum intercuspation (MIP) were obtained. After a thorough rinse, the scanbody was removed and replaced by an open tray impression coping (Straumann RN synOcta impression cap) and a conventional pick‐up impression was taken using the earlier made individual tray and a polyether impression material (3 M Impregum Penta) (Figure 3). In case of an instable MIP or an implant placed in the most distal tooth position, a bite registration was obtained with 8 mm RN bite registration aids (Straumann) using a vinyl polysiloxane bite registration material (Futar D Fast, Kettenbach GmbH & Co, Eschenburg, Germany). The impression of the opposing arch was obtained using alginate (Cavex Impressional NS). Both the STL‐file of the digital impression and the conventional impressions were sent to a dental laboratory and further processed within 24 h. The implant analogues were placed on the copings captured in the conventional impressions in the laboratory to minimize the risk of deformation during transportation.
FIGURE 1.

Clinical situation at inclusion: posterior osseointegrated tissue level implant
FIGURE 2.

Scan body for IOS
FIGURE 3.

Conventional pick‐up impression
2.3. Laboratory phase
After processing of the conventional‐ (pouring) and digital impressions (downloading) in the laboratory the dental technician opened the attached sealed randomization envelop stating to which study group the restoration would belong. With that, only one restoration per implant was produced either based on the conventional impression or on the IOS. For the restorations in the conventional group, Straumann Mono Scanbodies were placed on the created stone cast (Primus goldbraun, Klasse 4 Dental GmbH) and these were digitized with a desktop laboratory scanner (3Series, Dental Wings Inc.). For the restorations in the digital group, the open‐source STL‐files were imported in the laboratory CAD software (DWOS, Dental Wings) and the workflow was started with a model builder to design a 3D‐printed model (Dreve Dentamid GmbH, Unna, Germany) in which special repositionable implant analogs (Straumann) could be placed. Following this protocol both groups were digitized, and thus the following entire CAD/CAM procedure for both research groups would be completely identical. Therefore, the only difference between the test and control group was the method of impression taking and the subsequent model forming.
For both the test and control group monolithic zirconia (3 M Lava Plus) screw‐retained implant crowns to be luted on ti‐base abutments (Straumann Variobase for crown RN AH 4 mm) were designed in the CARES X‐stream workflow of the DWOS software. All crowns were fabricated in the same centralized milling facility (Straumann CAD/CAM‐Center). The dental laboratory finalized and individualized the crowns by applying a thin layer of glaze and staining (IPS e.max Ceram, Ivoclar Vivadent). Depending on the study group, conformation on the seating of the crowns and luting was performed on either the conventional cast‐ or the 3D‐printed models. Luting of the crowns onto the ti‐base abutments was performed with luting composite (Multilink Hybrid Abutment, Ivoclar Vivadent).
2.4. Restorative phase
3 weeks after impressions the patients were recalled for placement of the final restorations. To ensure a blinded study design the clinician received the crowns from the dental laboratory without any information on the production process or a model to verify the fit (Figure 4). One experienced clinician (WD) performed all fit examinations. The only available information given was the patient's name and tooth number. After removal of the healing abutments the crowns were tried in. First the interproximal contacts were controlled with dental floss and complete seating of the crown was assessed (Figure 5). Primarily Waxed Floss (Reach, Johnson & Johnson) was used. If this floss would not give enough tug‐back a thicker Waxed Dentotape (Reach, Johnson & Johnson) was used while the abutment screw was torqued 15 Ncm. If this dentotape would give sufficient tug‐back, the contact was quantified as being slightly weak but clinically acceptable. If not, the contact was too weak and deemed unacceptable. After this, final torque (35 Ncm) was applied to the abutment screws and the above‐mentioned steps were repeated. This was followed by checking the occlusion with 12 μ occlusion foil and 8 μ shimstock (Hanel, Coltène Whaledent) to confirm occlusal contact. If there was imprint with the occlusion foil but no tug‐back with the shimstock the occlusal contact was considered weak but clinically acceptable. If there was no colored imprint of the occlusion foil the occlusion was deemed unacceptable. If any corrections (occlusal or contact points) were deemed necessary a stopwatch was started and the time (in min) needed to perform these corrections was recorded. Corrections were performed with fine diamond burr with a maximum grit size of 50μ (red ring) and copious water‐cooling. This was followed by polishing the corrected surfaces for at least 2 min per touched surface with a specific zirconia polishing kit (eZr, Garrison). The correction and polishing was, where possible, performed extra‐orally. Sealing the screw access channel was the last step in the restorative protocol: first the screw channel was cleaned with a specific agent which removes phospholipids due to saliva contamination (Ivoclean, Ivoclar Vivadent), subsequently teflon tape was applied to protect the occlsal screw, followed by the application of an MDP‐containing bonding agent (Scotchbond Universal, 3 M), and a dentin‐shade occlusal composite restoration (Filtek Supreme XTE, 3 M). To prevent discoloration of the occlusal composite restoration a second light cure was performed after applying a layer of glycerine gel.
FIGURE 4.

Delivery of solitary monolithic zirconia crown luted on ti‐base abutment to clinician (without any further information or model)
FIGURE 5.
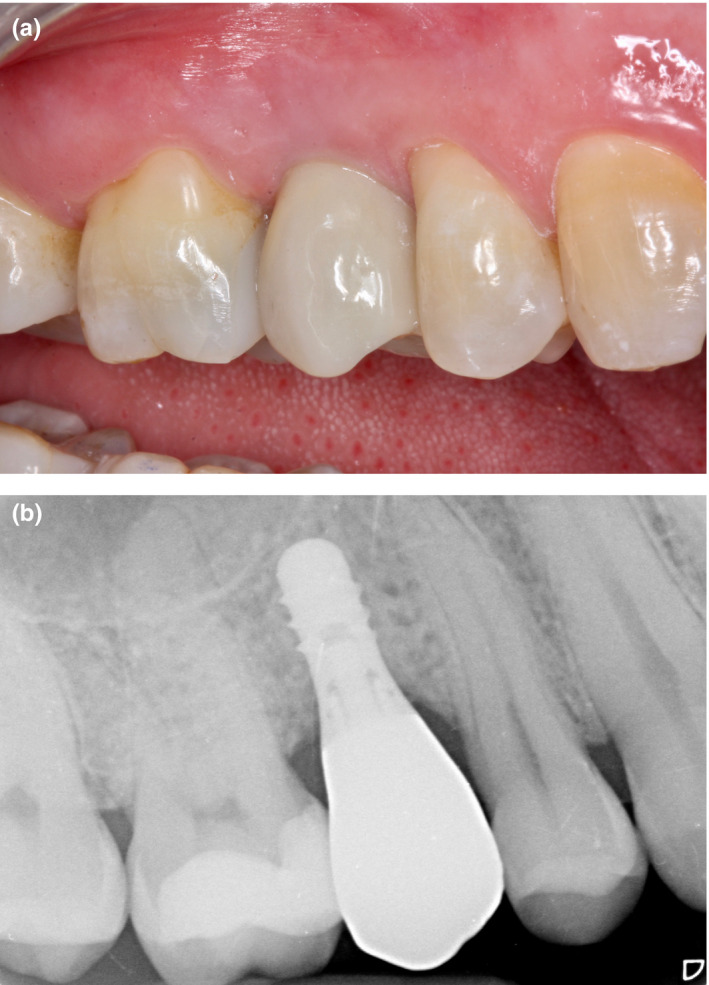
A + B. Clinical and radiological situation directly after placement
Directly after placement of the restoration the clinician filled in a questionnaire stating if it was either a (1) Proper fit (no adjustments required), (2) Adjustment‐requiring fit, or (3) Unacceptable fit (laboratory intervention required). Also, the location(s) of the corrections and the extra time necessary to perform these adjustments and polishing were noted per crown. A restoration was considered unacceptable in case of either a lack of occlusion and/or interproximal contacts or such extreme over‐contouring that corrections in the laboratory were deemed necessary. In case of an unacceptable restoration, a new set of impressions and bite registrations was taken immediately. If such an event would occur, the documented correction time required for statistical purposes was determined at 40 min (the time lost by the extra appointment) plus the time of adjustment during the (extra) third session.
2.5. Follow‐up
All patients were recalled 1 year after placement of the restorations. In addition to overall survival of the restoration the following potential complications were documented: (1) Screw loosening, (2) Ceramic fracture, (3) Ceramic chipping, (4) De‐cementation from ti‐base abutment, (5) Loss of the occlusal composite restoration.
2.6. Outcomes
A distinction was made between proper fit, adjustment‐requiring fit and unacceptable fit at placement. The primary outcome variable was the time required (in minutes) for potential adjustments at the time of placement of the crowns. Additionally the locations of these adjustments were recorded (occlusal, interproximal mesial and distal). As secondary outcome variable mechanical complications and survival of these implant restorations during the first year of function were reported.
2.7. Sample size
Performing a proper sample size calculation was challenging since at baseline very limited comparable data was available. One study performed clinical fit comparison of conventional versus digital impressions for crowns on natural teeth (Syrek et al., 2010). A difference of 20µm in marginal gap fit of single crowns in favor of digital impressions (SD: 15 µm) versus conventional impressions (SD: 25 µm) was reported. The question remains if these differences are representative for the clinical evaluation of fit in our study. One of the parameters checked in our study is the occlusion. The thinnest occlusion foil used to judge if a restoration is too high is 12 µm thick. This would mean that the reported difference of 20 µm could be clinically significant. Based on these figures and assumptions, a desired statistical power level of 0.90 and a probability level of 0.05 a minimum total sample size (two‐tailed hypothesis) of 48 was calculated.
2.8. Randomization
In advance, 2 × 25 sealed envelopes—containing information to which study group a case was divided—were created. All envelopes were prepared by an independent researcher and marked with a randomly generated code. This code was used for all further registrations by the clinician. The list of codes and their associated research group was only accessible by the statistician. Per implant restoration one of these sealed envelopes was sent together with the impressions to the dental laboratory. The clinician was therefore blinded to which impression the dental technician would use to produce the subsequent restoration. If a patient would have more than one implant, the second implant would be restored using the alternative impression technique. Any third implant would be randomized again and a fourth implant would routinely be the different from the third again. Therefore, any patient included in the study with more than one implant is inevitably included in both study groups. This was done to minimize potential patient factors.
2.9. Statistics
All data analyses were carried out according to a pre‐established analysis plan. During data collection, there was no knowledge about which research group the patient's restoration was assigned to. The data were analyzed using SPSS version 24 (SPSS). Data were analyzed at restoration level. For the primary outcome variable–the correction time in minutes per restoration—a Shapiro–Wilk test of normality was first performed. Nonetheless, since proper fit would result a value of zero normality is unlikely. Further comparison between test and control groups—in case of the expected non‐normally‐distributed data—was performed using Wilcoxon rank sum tests (Mann–Whitney U). The level of significance was set at α = .05. The secondary outcome variables will be reported with descriptive statistics only.
3. RESULTS
Initially 34 patients requiring 48 solitary implant restorations were recruited in the study. The distribution of the implant crowns is shown in table 1. One patient (with one implant) dropped out because of financial reasons before placement of the final crown and one patient (with two implants) passed away between impression and placement of the final restoration. With that, 32 patients with 45 solitary implant crowns were included and completed the study protocol. All 32 patients were recalled after one year. The randomly assigned test group consisted of 23 and the control of 22 crowns respectively. Twenty‐one patients received one crown, nine patients received two crowns and two patients received three crowns included in the study. The inclusion‐ and randomization process of all implant‐supported solitary crowns (ISCs) was schematically illustrated in a flowchart (Figure 6).
TABLE 1.
Distribution of crowns
| Upper jaw: | FDI: | 14 | 15 | 16 | 17 | 24 | 25 | 26 |
| 21 × | 1 × | 5 × | 2 × | 1 × | 1 × | 4 × | 7 × | |
| Lower jaw: | FDI: | 35 | 36 | 45 | 46 | 47 | ||
| 24 × | 2 × | 7 × | 3 × | 8 × | 4 × |
FIGURE 6.
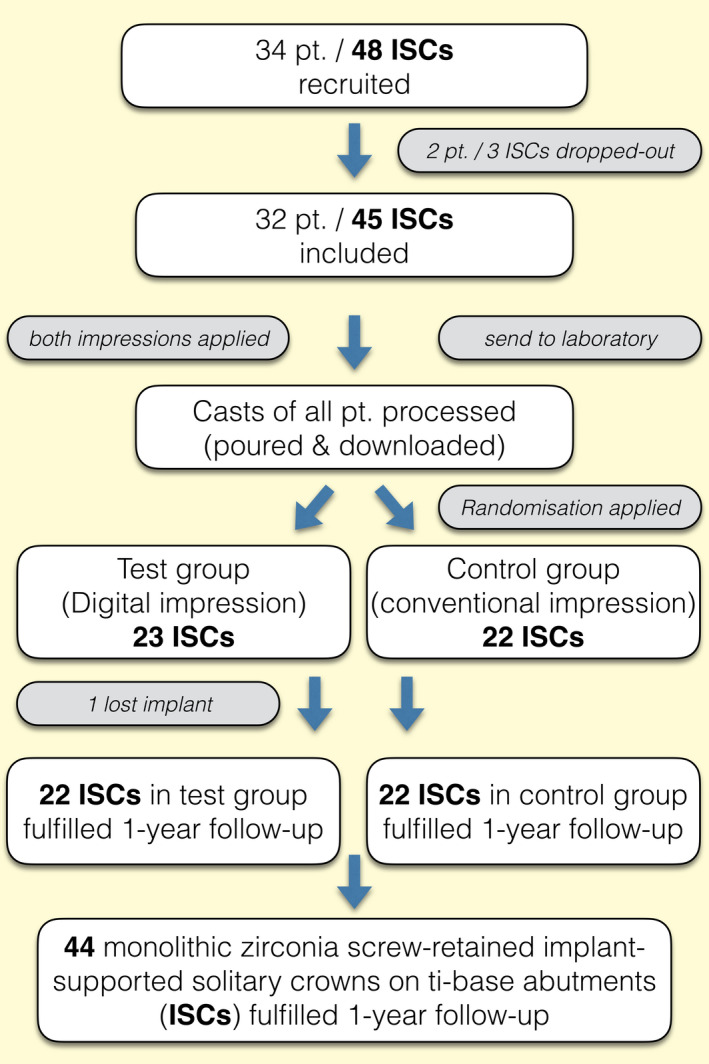
Flowchart of inclusion‐ and randomization process
A “proper fit’—without any adjustments—occurred in nine of the 23 (39,1%) crowns in the test and four of the 22 (18,2%) crowns in the control group respectively. Fourteen crowns in the test group (60,9%) required adjustment prior to placement and were therefore classified as “adjustment‐requiring fit” versus. eighteen crowns in the control group (81,8%). The time required for these adjustments in the test group ranged from 3 to 11 min. Four of the crowns in the test group needed occlusal adjustment (17,4%), twelve had a too tight mesial contact (52,2%), and seven (of the eighteen crowns that had distal neighboring tooth) needed distal contact correction (38,9%). For these crowns in the control group, the correction times required ranged from 2 to 18 min. Ten crowns exhibited a too tight occlusal contact (45,5%), and of one crown the occlusal contact was considered slightly too weak (4,5%). Twelve crowns had a too tight mesial contact (54,5%) and of the of the eighteen crowns that had distal neighboring tooth in this group, nine (50%) had a too tight and one crown demonstrated a slightly too loose distal contact (5,6%). Of all crowns included in the study no “unacceptable fit” was reported and therefore all implants were restored as planned.
Of all crowns included, significantly less average adjustment time was required in the IOS (test) group with 3.35 min (SD ± 3.38, range: 0–11 min) versus. 6.09 min (SD ± 4.63, range: 0–18 min) in the conventional impression (control) group (p = .039). The results are summarized in table 2.
TABLE 2.
Fit and possible adjustments of solitary implant crowns based on IOS (test) versus. conventional (control) impressions
| Solitary implant crowns based on | ||
|---|---|---|
| Digital impression | Conventional impression | |
| n = 23 | n = 22 | |
| Proper fit | 9 (39,1%) | 4 (18,2%) |
| Adjustment‐requiring fit | 14 (60,9%) | 18 (81,8%) |
| Location of adjustments/inaccuracies | ||
| Occlusal—too high | 4 (17,4%) | 10 (45,5%) |
| Occlusal—too weak | – | 1 (4,5%) |
| Mesial contact—too tight | 12 (52,2%) | 12 (54,5%) |
| Mesial contact—too loose | – | – |
| Distal contact, if present—too tight | 7/18 (38,9%) | 9/18 (50%) |
| Distal contact, if present—too loose | – | 1/18 (5,6%) |
| Unacceptable fit | – | – |
| Average time required for corrections |
3.35 min (SD ± 3.38)* range: 0–11 min |
6.09 min (SD ± 4.63)* range: 0–18 min |
Statistical analysis (Wilcoxon rank sum tests) *(p = .039).
During the first year of function two mechanical complications occurred in conventional group on the same implant (FDI: 26): its crown—with a gold restoration on a natural tooth as antagonist–demonstrated mobility due to screw loosening 5 months after placement. After reattachment, the same crown de‐cemented from its ti‐base abutment within a month. This crown turned out to have an occlusal interference in lateral excursion and was adjusted. In the digital group one implant demonstrated mobility without any signs of inflammation three months after placement of the restoration. It was a 4.1x8mm implant replacing a missing 26 FDI. There were no mechanical issues to the abutment or crown when the implant was removed together with its crown. If this lost implant was quantified as a drop‐out the overall the restoration survival was 100% after one year. If lost implants—failed for other than mechanical issues—are also included in the survival rates of the restorations the overall restoration survival rate was 97,8%. The survival and complication rates of the crowns recalled after one year are reported in table 3.
TABLE 3.
Clinical performance of monolithic zirconia screw‐retained crowns on ti‐base abutments during the first year of function
| Solitary implant crowns based on | |||
|---|---|---|---|
| Digital impression | Conventional impression | Total | |
| Baseline | n = 23 | n = 22 | n = 45 |
| Implants lost (without prosthetic reason) | 1 | ‐ | 1 |
| One‐year follow‐up | n = 22 | n = 22 | n = 44 |
| Mechanical complications: | |||
| Screw loosening: | – | 1 | 1 (2,3%) |
| Ceramic fracture: | – | – | ‐ (0,0%) |
| Ceramic chipping: | – | – | ‐ (0,0%) |
| De‐cementation from ti‐base abutment | – | 1 | 1 (2,3%) |
| Loss of occlusal composite restoration | – | – | ‐ (0,0%) |
| Restoration survival (1 year) | 100% | 100% | 100% |
| Restoration survival—lost implants included (1 year) | 95,7% | 100% | 97,8% |
4. DISCUSSION
The aim of this randomized clinical trial was to compare the use of digital versus. conventional impression techniques for application in the digital workflow in the laboratory phase to produce monolithic zirconia screw‐retained implant solitary implant restorations. Monolithic restorations are increasingly popular due to promising mechanical characteristics and cost‐effectiveness (Joda & Bragger, 2016). Since the production workflow of these monolithic restorations is predominantly digital, it seems logical to immediately digitize the required information in the patient's mouth utilizing IOS. In contrary to studies in which digital and completely conventional workflows were compared (Delize et al., 2019; Joda et al., 2016)—resulting in multiple possible effects influencing the fit of the restorations–it was attempted to solely test the effect of the impression technique in our study. For that reason, the same restorative material, implant abutment type, and CAD/CAM software and parameters were applied for the test and the control restorations in our study.
In order to minimize patient factors and to strive for a double‐blind setup (patients and clinician), patients underwent both digital and conventional impressions in our study. In the above‐mentioned clinical study by Joda et al. patients also underwent both impression techniques but instead of receiving only one restoration based on randomization, both a (zirconia) digital and a (PFM) conventional restoration were tested per patient. This consequently meant that the clinician preforming the fit test is not blinded for the production and impressions process. In our study the clinicians were blinded, however—as a consequence of the followed the production workflow of the restorations—the technicians could also not be blinded in our study. After the clinical fit test only the test restorations were placed in the Joda et al. study in contrast to our study in which also the follow‐up study remains designed as a RCT. Nevertheless, the value of this randomization for the follow‐up period is disputable since both test and control restorations in our study are supposed to be identical. Consequently, from the moment of placement these restorations should behave similar and little difference in future follow‐up can be expected between the crowns in the test and the control groups. For this reason, the total amount of restorations is also reported in the results table.
Although focusing on the entire digital workflow, still some conventional laboratory steps are applied in both protocols and could have influenced the results. First of all, the monolithic zirconia restorations were stained and glazed—as commonly applied in daily clinical practice—with a thin layer of nano‐fluorapatite glass ceramic. Although this layer is usually less then 50μm, it does change the outer shape of restorations and will therefore have an effect on occlusion and contact points. Although it is possible to anticipate on this thickness in the design software, the thickness is never completely uniform and therefore technicians usually prevent applying these layers on interproximal and occlusal contact areas, or manually remove it with polishers while verifying the fit on a cast model. This means however that the accuracy of a 3D‐printed cast has an influence on the fit of the final restoration. Since differences in accuracy of the 3D‐printed casts are reported and inconsistent results are presented (Alshawaf et al., 2018; Buda et al., 2018), caution should to taken when utilizing these 3D‐printed casts. Although less esthetic, a 100% monolithic restoration–without any glaze layer and produced without the use of any cast—would therefore theoretically have been superior for evaluating the clinical accuracy of this digital workflow. Second of all, the production and processing of dental casts is prone to an accumulation of errors. The impression material used, the time required for processing and the decision whether or not the analogs were placed on the copings directly all could play a role in the accuracy of the working cast. The study has tried to mimic clinical reality as much as possible and therefore decisions such as using alginate as antagonist impression material were made. Last but not least, the luting step required to extra‐orally connect a crown to a ti‐base abutment could introduce issues (e.g., occlusal changes) to an otherwise perfectly designed and produced (well‐fitting) crown. Since these factors and its introduced inaccuracies could happen in both groups—and in daily clinical practice—we had to accept that these factors were part of the protocol.
The time required for clinical fitting and adjustments of restorations is not the only possible time‐related factor when comparing digital versus conventional workflows. Other authors have also reported shorter laboratory times (Joda & Bragger, 2016; Sailer et al., 2017), and reduced time required for obtaining the impressions in the digital workflow (Gjelvold et al., 2016). In general, it can also be stated that time‐related results are arbitrary. No clinician or dental technician works exactly with the same efficacy and even some scanners, materials or software packages allow more time than others. Therefore, it is the author's opinion that time‐related outcomes should always be interpreted with care.
Also, the decision to choose between full‐arch IOS or partial scan can be of influence on the time‐efficacy. Obviously, a partial scan requires less time than a full arch scan. In this particular study it was decided to obtain full‐arch impressions. Since this study only deals with solitary posterior restorations, a partial scan would also have been a possibility. Retrospectively, this might have been more accurate since recent data supports the improved accuracy for partial scans (Ender, Attin, et al.,2016; Ender, Zimmermann, et al., 2016). Therefore, not only the scan‐time but also the adjustment times might have been shorter if partial scans were used. This is, however, hypothetical and should be confirmed by further clinical studies.
In the current study, it was decided to always scan first and then take the conventional impression. This decision was mainly due to practical reasons: No impression materials would be stuck between teeth which could influence the IOS and patients were less likely to come into a “gagging reflex modus” already at the start of the appointment. Retrospectively, this order of impressions could potentially have led to some bias if—for example—patients became tired, and with that, less cooperative during their conventional impression.
Although promising on short term, there is still very little clinical evidence on using monolithic zirconia, especially on implants. This study shows promisingly low‐mechanical complications whereas other studies report chipping as a major issue for implant supported—non monolithic—restorations (Larsson & Vult von Steyern, 2010). The hardness and possible abrasiveness of adjusted and re‐polished monolithic zirconia, however, remains a topic that needs further investigation. It is the author's opinion to not only perform in vitro studies on this topic but also perform long‐term clinical studies that focus both on the clinical performance of the restoration and the evolution of wear in the opposing dentition.
Based on the results of this study, the application of solitary screw‐retained monolithic zirconia restorations on ti‐base abutments seems to be a suitable treatment option in the posterior area. Nevertheless, this study did not focus on biological factors and bone stability around the restored implants. The latter also seems to be depending on configuration and location of the prosthetic connection (Lago et al., 2018). Moreover, different implant platforms also have different abutment designs and mechanical complications can thus also be different. Hence, possible conclusions from this tissue level implant study cannot not be extrapolated one‐to‐one to other implant types and prosthetic connections.
5. CONCLUSIONS
Within the limitation of clinical study, the following conclusions can be summarized:
The use of intraoral optical scanning (IOS) results shorter clinical adjustment times at try‐in of CAD/CAM solitary screw‐retained monolithic zirconia implant restorations when compared to using conventional impressions for the same restoration type.
Screw‐retained solitary monolithic zirconia restorations on implants exhibit low complication rates and promising survival on the short term (one‐year follow‐up).
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
WD and AT conceived the ideas, WD collected the DATA, WD, and DW analyzed the data, and WD and DW led the writing.
ETHICAL APPROVAL
The study protocol was approved by the regional ethical committee of VU‐Medical Center, Amsterdam, the Netherlands (No. 2013‐152NL43489.029.13) and was performed in accordance with the Declaration of Helsinki guidelines on medical human research ethics.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
This RCT was supported by a research grant from the International Team for Implantology, Basel, Switzerland (ITI_909_2013). Implants and abutments were supplied by Straumann AG, Basel Switserland. The sponsors had no influence upon the study design, analysis or interpretation of the data, on the writing of the manuscript or on submission for publication. In addition, the authors express their gratitude to Tandtechnisch Laboratorium Zutphen for their laboratory work and endless support.
Derksen, W., Tahmaseb, A., & Wismeijer, D. Randomized Clinical Trial comparing clinical adjustment times of CAD/CAM screw‐retained posterior crowns on ti‐base abutments created with digital or conventional impressions. One‐year follow‐up. Clinical Oral Implants Research. (2021);32:962–970. 10.1111/clr.13790
Funding information
This study was supported by an ITI clinical research grant (ITI_909_2013). Implant materials were supplied by Straumann AG.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Alikhasi, M., Siadat, H., Nasirpour, A., & Hasanzade, M. (2018). Three‐dimensional accuracy of digital impression versus conventional method: Effect of implant angulation and connection type. International Journal of Dentistry. 2018:3761750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshawaf, B., Weber, H. P., Finkelman, M., El Rafie, K., Kudara, Y., & Papaspyridakos, P. (2018). Accuracy of printed casts generated from digital implant impressions versus stone casts from conventional implant impressions: A comparative in vitro study. Clinical Oral Implants Research, 29(8), 835–842. 10.1111/clr.13297 [DOI] [PubMed] [Google Scholar]
- Alves de Carvalho, I., Santos Marques, T., Araujo, F., Azevedo, L., Donato, H., & Correia, A. (2018). Clinical performance of cad/cam tooth‐supported ceramic restorations: A systematic review. The International Journal of Periodontics & Restorative Dentistry, 38, e68–e78. 10.11607/prd.3519 [DOI] [PubMed] [Google Scholar]
- Buda, M., Bratos, M., & Sorensen, J. A. (2018). Accuracy of 3‐dimensional computer‐aided manufactured single‐tooth implant definitive casts. Journal of Prosthetic Dentistry, 120, 913–918. 10.1016/j.prosdent.2018.02.011 [DOI] [PubMed] [Google Scholar]
- Burgess, J. O., Janyavula, S., Lawson, N. C., Lucas, T. J., & Cakir, D. (2014). Enamel wear opposing polished and aged zirconia. Operative Dentistry, 39, 189–194. 10.2341/12-345-L [DOI] [PubMed] [Google Scholar]
- De Angelis, P., Passarelli, P. C., Gasparini, G., Boniello, R., D'Amato, G., & De Angelis, S. (2020). Monolithic cad‐cam lithium disilicate versus monolithic cad‐cam zirconia for single implant‐supported posterior crowns using a digital workflow: A 3‐year cross‐sectional retrospective study. Journal of Prosthetic Dentistry, 123, 252–256. 10.1016/j.prosdent.2018.11.016 [DOI] [PubMed] [Google Scholar]
- Delize, V., Bouhy, A., Lambert, F., & Lamy, M. (2019). Intrasubject comparison of digital vs. Conventional workflow for screw‐retained single‐implant crowns: Prosthodontic and patient‐centered outcomes. Clinical Oral Implants Research, 30, 892–902. 10.1111/clr.13494 [DOI] [PubMed] [Google Scholar]
- Ender, A., Attin, T., & Mehl, A. (2016). In vivo precision of conventional and digital methods of obtaining complete‐arch dental impressions. Journal of Prosthetic Dentistry, 115, 313–320. [DOI] [PubMed] [Google Scholar]
- Ender, A., Zimmermann, M., Attin, T., & Mehl, A. (2016). In vivo precision of conventional and digital methods for obtaining quadrant dental impressions. Clinical Oral Investigations, 20, 1495–1504. 10.1007/s00784-015-1641-y [DOI] [PubMed] [Google Scholar]
- Flugge, T. V., Att, W., Metzger, M. C., & Nelson, K. (2016). Precision of dental implant digitization using intraoral scanners. The International Journal of Prosthodontics, 29, 277–283. 10.11607/ijp.4417 [DOI] [PubMed] [Google Scholar]
- Gimenez‐Gonzalez, B., Hassan, B., Ozcan, M., & Pradies, G. (2016). An in vitro study of factors influencing the performance of digital intraoral impressions operating on active wavefront sampling technology with multiple implants in the edentulous maxilla. Journal of Prosthodontics, 26, 650–655. 10.1111/jopr.12457 [DOI] [PubMed] [Google Scholar]
- Gjelvold, B., Chrcanovic, B. R., Korduner, E. K., Collin‐Bagewitz, I., & Kisch, J. (2016). Intraoral digital impression technique compared to conventional impression technique. A Randomized Clinical Trial. Journal of Prosthodontics, 25, 282–287. 10.1111/jopr.12410 [DOI] [PubMed] [Google Scholar]
- Joda, T., & Bragger, U. (2014). Complete digital workflow for the production of implant‐supported single‐unit monolithic crowns. Clinical Oral Implants Research, 25, 1304–1306. 10.1111/clr.12270 [DOI] [PubMed] [Google Scholar]
- Joda, T., & Bragger, U. (2016). Time‐efficiency analysis of the treatment with monolithic implant crowns in a digital workflow: A randomized controlled trial. Clinical Oral Implants Research, 27, 1401–1406. 10.1111/clr.12753 [DOI] [PubMed] [Google Scholar]
- Joda, T., Ferrari, M., & Bragger, U. (2017). Monolithic implant‐supported lithium disilicate (ls2) crowns in a complete digital workflow: A prospective clinical trial with a 2‐year follow‐up. Clinical Implant Dentistry and Related Research, 19, 505–511. 10.1111/cid.12472 [DOI] [PubMed] [Google Scholar]
- Joda, T., Katsoulis, J., & Bragger, U. (2016). Clinical fitting and adjustment time for implant‐supported crowns comparing digital and conventional workflows. Clinical Implant Dentistry and Related Research, 18, 946–954. 10.1111/cid.12377 [DOI] [PubMed] [Google Scholar]
- Joda, T., Zarone, F., & Ferrari, M. (2017). The complete digital workflow in fixed prosthodontics: A systematic review. BMC Oral Health, 17(1), 124. 10.1186/s12903-017-0415-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon, S. J., Lawson, N. C., McLaren, E. E., Nejat, A. H., & Burgess, J. O. (2018). Comparison of the mechanical properties of translucent zirconia and lithium disilicate. Journal of Prosthetic Dentistry, 120, 132–137. 10.1016/j.prosdent.2017.08.004 [DOI] [PubMed] [Google Scholar]
- Lago, L., da Silva, L. , Martinez‐Silva, I., & Rilo, B. (2018). Crestal bone level around tissue‐level implants restored with platform matching and bone‐level implants restored with platform switching: A 5‐year randomized controlled trial. International Journal of Oral and Maxillofacial Implants, 33(2), 448–456. 10.11607/jomi.6149 [DOI] [PubMed] [Google Scholar]
- Larsson, C., & Vult von Steyern, P. (2010). Five‐year follow‐up of implant‐supported y‐tzp and zta fixed dental prostheses. A randomized, prospective clinical trial comparing two different material systems. The International Journal of Prosthodontics, 23, 555–561. [PubMed] [Google Scholar]
- Lee, S. J., & Gallucci, G. O. (2012). Digital vs. Conventional implant impressions: Efficiency outcomes. Clin Oral Implants Res, 24, 111–115. 10.1111/j.1600-0501.2012.02430.x [DOI] [PubMed] [Google Scholar]
- Pjetursson, B. E., Asgeirsson, A. G., Zwahlen, M., & Sailer, I. (2014). Improvements in implant dentistry over the last decade: Comparison of survival and complication rates in older and newer publications. International Journal of Oral and Maxillofacial Implants, 29(Suppl), 308–324. 10.11607/jomi.2014suppl.g5.2 [DOI] [PubMed] [Google Scholar]
- Preis, V., Behr, M., Handel, G., Schneider‐Feyrer, S., Hahnel, S., & Rosentritt, M. (2012). Wear performance of dental ceramics after grinding and polishing treatments. Journal of the Mechanical Behavior of Biomedical Materials, 10, 13–22. 10.1016/j.jmbbm.2012.03.002 [DOI] [PubMed] [Google Scholar]
- Preis, V., Behr, M., Kolbeck, C., Hahnel, S., Handel, G., & Rosentritt, M. (2011). Wear performance of substructure ceramics and veneering porcelains. Dental Materials, 27, 796–804. 10.1016/j.dental.2011.04.001 [DOI] [PubMed] [Google Scholar]
- Rosentritt, M., Preis, V., Behr, M., Hahnel, S., Handel, G., & Kolbeck, C. (2012). Two‐body wear of dental porcelain and substructure oxide ceramics. Clinical Oral Investigations, 16(3), 935–943. 10.1007/s00784-011-0589-9 [DOI] [PubMed] [Google Scholar]
- Sailer, I., Benic, G. I., Fehmer, V., Hammerle, C. H. F., & Muhlemann, S. (2017). Randomized controlled within‐subject evaluation of digital and conventional workflows for the fabrication of lithium disilicate single crowns. Part ii: Cad‐cam versus conventional laboratory procedures. Journal of Prosthetic Dentistry, 118, 43–48. [DOI] [PubMed] [Google Scholar]
- Syrek, A., Reich, G., Ranftl, D., Klein, C., Cerny, B., & Brodesser, J. (2010). Clinical evaluation of all‐ceramic crowns fabricated from intraoral digital impressions based on the principle of active wavefront sampling. Journal of Dentistry, 38, 553–559. 10.1016/j.jdent.2010.03.015 [DOI] [PubMed] [Google Scholar]
- van der Meer, W. J. , Andriessen, F. S., Wismeijer, D., & Ren, Y. (2012). Application of intra‐oral dental scanners in the digital workflow of implantology. PLoS ONE, 7, e43312. 10.1371/journal.pone.0043312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandeweghe, S., Vervack, V., Dierens, M., & De Bruyn, H. (2016). Accuracy of digital impressions of multiple dental implants: An in vitro study. Clinical Oral Implants Research, 28, 648–653. [DOI] [PubMed] [Google Scholar]
- Wittneben, J. G., Wright, R. F., Weber, H. P., & Gallucci, G. O. (2009). A systematic review of the clinical performance of cad/cam single‐tooth restorations. The International Journal of Prosthodontics, 22, 466–471. [PubMed] [Google Scholar]
- Zimmermann, M., Mehl, A., Mormann, W. H., & Reich, S. Intraoral scanning systems ‐ A current overview. International Journal of Computerized Dentistry. 2021;00:1–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


