FIG. 4.
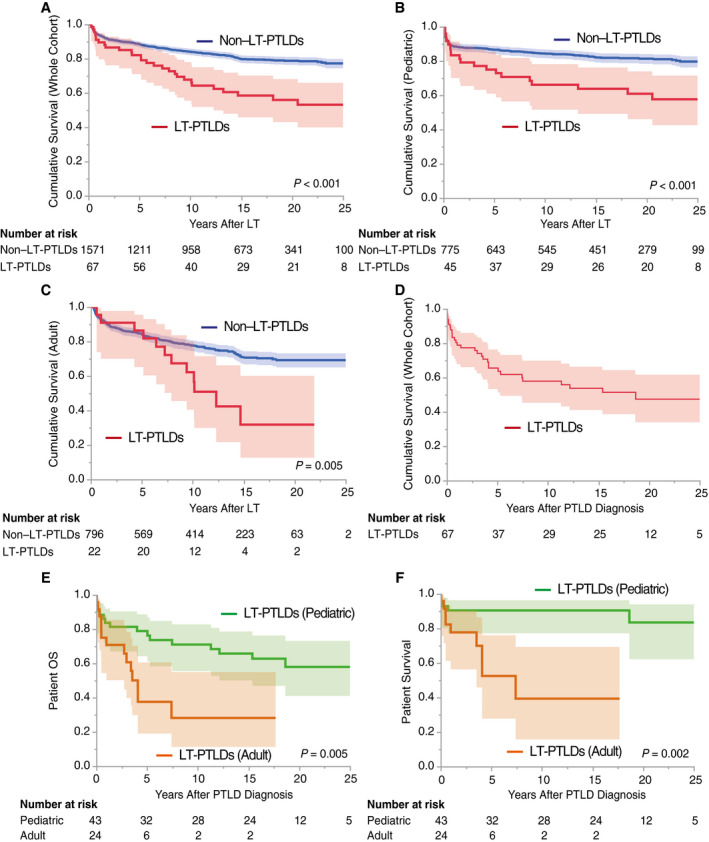
Patient survival after LT and PTLD diagnosis. The recipients who died within 3 months were excluded to eliminate the influence of early mortality from other causes, that is, the severe infections, refractory rejections, or intracranial bleeding in Fig. 2A‐C. The shaded areas show 95% CI. (A) Overall recipient survival: LT‐PTLDs versus non–LT‐PTLDs. Comorbid LT‐PTLDs significantly worsened recipient survival compared with those without (P < 0.001 by a log‐rank test). (B) Pediatric recipient survival: LT‐PTLDs versus non–LT‐PTLDs. Similarly, comorbid LT‐PTLDs in the pediatric cohort (<18 years of age) significantly worsened recipient survival compared with those without (P < 0.001). (C) Adult recipient survival: LT‐PTLDs versus non–LT‐PTLDs. In the adult cohort, comorbid PTLDs significantly worsened recipient survival compared with those without (P = 0.005). (D) Patient OS in LT‐PTLDs. The overall 3‐year, 5‐year, and 10‐year patient survival rates after LT‐PTLD diagnosis were 74%, 66%, and 58%, respectively. (E) Patient OS in LT‐PTLDs: pediatric versus adult cases. The 3‐year, 5‐year, and 10‐year pediatric patient survival rates after LT‐PTLD diagnosis were 81%, 79%, and 71%, respectively, whereas those of adults were 61%, 38%, and 28%, respectively. Pediatric LT‐PTLDs showed significantly better patient survival than adult PTLDs (P = 0.005). (F) Patient survival in LT‐PTLDs: pediatric versus adult cases. Patient deaths not related to PTLD were treated as "censored." LT‐PTLD–associated mortality was significantly lower in pediatric LT‐PTLDs than in adult LT‐PTLDs (P = 0.002).
