Abstract
Background and Aim
The Global Ulcerative Colitis (UC) Narrative Survey aimed to evaluate the impact of UC, perceptions of UC burden, and management approaches. Here, we present data from patients and physicians in Australia.
Methods
Surveys, fielded by The Harris Poll, were completed by 215 patients with UC and 90 physicians, between August 2017 and February 2018. Surveys included questions on disease characteristics, impact on life, communication with physicians, and patient knowledge of UC. Results are presented descriptively from all respondents (with no imputation for missing data).
Results
Based on medication history, 84% of patients had moderate to severe UC. Diagnostic delay was on average 1.9 (SD 5.0) years and 48% of patients had waited ≥1 year for diagnosis. Nearly two‐thirds (65%) of patients considered themselves to be in remission, with 97% also reporting a flare in the past year. The majority (92%) of patients were satisfied with their UC medication and, if their treatment made them feel “good enough,” many (75%) would not consider an alternative. Most (90%) patients were satisfied with communication with their physician; however, only 48% felt comfortable raising emotional concerns. Both patients and physicians desired more time during routine appointments. Patients had gaps in their knowledge of UC, which physicians mostly recognized.
Conclusions
The Australian survey results highlighted the diagnostic delay and burden of UC patients' experience, gaps in patients' knowledge of UC, and challenges in patient–physician communication. Compared with the overall Global UC Narrative Survey, patients in Australia reported a high burden of disease.
Keywords: communication, survey, ulcerative colitis
The Australia‐specific patient and physician results from the Global Ulcerative Colitis Narrative Survey are reported; they highlight a high disease burden, problems of diagnostic delay, and challenges in patient–physician communication. Pfizer Inc funded editorial support and the study.
Introduction
Ulcerative colitis (UC) is a chronic inflammatory bowel disease affecting the mucosal layer of the colon, characterized by relapsing and remitting symptoms, including diarrhea, rectal bleeding, abdominal pain, fecal urgency, weight loss, and fatigue.1 Although UC does not reduce life expectancy,2 it is a markedly disabling disease for many patients that adversely affects quality of life.3 Added to the physical burden of the symptoms are the effects on the patient's psyche, caused by the impact of the disease on social, work, and emotional relationships.4
Australia has one of the highest incidence rates of UC in the world.5 An observational, prospective, population‐based epidemiologic study conducted in Barwon, Victoria, reported a crude incidence rate of 7.5 per 100 000 for 2010/2011, which had not changed significantly over a 3‐year period.6
Patient–physician communication is a vital element in the care of patients with UC, where the construction of collaborative relationships is a key part of achieving optimal disease management.7, 8 Arming patients with an adequate knowledge of UC enables them to confront both their disease and the possibilities of self‐management.9
The burden of UC surpasses the clinical symptoms alone4; therefore, the Global UC Narrative Survey was designed to engage patients with UC and physicians to gain insight into their perceptions of how UC affects patients' lives. The survey explored several aspects of living with UC, including day‐to‐day disease impact, disease management, goal setting, and communication.
The Global UC Narrative Survey was conducted across 10 countries: Australia, Canada, Finland, France, Germany, Italy, Japan, Spain, the United Kingdom, and the United States. Results from the global total relating to epidemiology, and from patients and physicians in Finland, have previously been reported.10, 11 Here, we present a subset of the Global UC Narrative Survey and report responses from patients and physicians residing in Australia to assess disease burden, treatment satisfaction and attributes, and patient–physician relationships. To the best of our knowledge, this is the first, and therefore a unique, survey of both patients with UC and physicians conducted in Australia.
Methods
Study design and populations
Full details of the Global UC Narrative Survey methodology, including participant recruitment and eligibility criteria, have been previously reported.11 In Australia, patient and physician surveys were completed between August 2017 and February 2018, and were fielded by The Harris Poll (a research company; https://theharrispoll.com/). In brief, patients were adults aged ≥18 years with UC who self‐reported that they had received a diagnosis of UC (confirmed by endoscopy), had not had a colectomy, had visited a gastroenterologist's office for their UC in the past 12 months, and had, at any time, taken prescription medications for their UC (excluding those who had only ever taken 5‐aminosalicylates [5‐ASA]). Eligible physicians were gastroenterologists (hereafter referred to as physicians) who saw at least 10 patients with UC per month, with at least 10% of these patients currently taking a biologic for their UC. Patients were recruited online, and physicians were recruited online and by telephone.
The primary goal of the survey was to characterize the experiences of patients with moderate to severe UC or poorly controlled disease. Based on self‐reported medication history, patients were categorized as having moderate to severe UC (patients who had ever taken immunosuppressants, tumor necrosis factor inhibitors, other biologics, or corticosteroids for 4 or more of the past 12 months) or milder UC (patients who had never taken an immunosuppressant or biologic; and had taken corticosteroids for their UC for <4 of the past 12 months, 5‐ASA, or other UC medication). Patients who had only ever taken 5‐ASA were excluded. Patients with milder UC were capped at 20% of the total survey respondents. Where applicable, the physician questionnaire mirrored the patient questionnaire, and physicians were asked to provide general information about all patients with moderate to severe UC for whom they were responsible and not individual patients, hence no direct links could be shown between the responses collected in the patient and physician surveys.
Patient‐reported outcomes
In the patient survey, patients' self‐reported remission and flares (in the past 12 months) were based on definitions that were included in the survey. Remission was defined as UC being controlled with few to no symptoms, and a flare was defined as a period with a dramatic increase in symptoms compared with those typically experienced; however, there was no cutoff duration for defining flare.
Analyses of patient and physician surveys
Questions on both the patient and physician questionnaires required respondents to either: provide a numeric response; select a single option or multiple options from a list; or indicate their level of agreement with a statement (ranging from “strongly disagree” to “strongly agree”). Patient and physician responses were assessed using descriptive statistics. Responses from patients with UC were not weighted, with no imputation for missing data and were, therefore, representative of patients completing the survey. Patient responses were analyzed by subgroups: age, gender, length of time since diagnosis, remission status, and patient advocacy organization (PAO) involvement. Physician results were weighted by age and gender to ensure alignment with actual proportions in the population of gastroenterologists in Australia.12
Ethical considerations
The surveys were non‐interventional and were not conducted as a clinical trial; ethics approval was therefore not required. Patients and physicians provided informed consent to complete the surveys.
Results
Survey respondents
Patient respondents (n = 215) with UC had a mean age of 41.1 (SD 14.7) years, and 84% had moderate to severe UC. The median duration of UC was 3 (standard error [SE] 0.6) years, the mean time from first symptom to UC diagnosis was 1.9 (SD 5.0) years (Table 1), and 47% of patients had a delay between symptoms and diagnosis of ≥1 year.
Table 1.
Demographic characteristics of the patients (n = 215) completing the survey
| Demographic characteristic | |
|---|---|
| Age, mean (SD), years | 41.1 (14.7) |
| Male, % | 59 |
| Family history of IBD, % | 39 |
| Age when first experienced symptoms, mean (SD), years | 32.7 (15.6) |
| Age at diagnosis, mean (SD), years | 34.6 (14.6) |
| Time between first symptoms and UC diagnosis, mean (SD), years | 1.9 (5.0) |
| Length of time since UC diagnosis, mean (SD), years | 6.5 (8.2) |
| Patients who self‐report remission,† % | 65 |
| Marital status, % | |
| Never married | 20 |
| Married or civil union | 61 |
| Divorced | 4 |
| Separated | 3 |
| Widow/widower | 2 |
| Living with partner | 10 |
| Employment status, % | |
| Employed or self‐employed | 75 |
| Retired | 11 |
| Stay at home spouse/partner | 5 |
| Unable to work due to a disability or illness | 4 |
| Student | 3 |
| Unemployed, seeking work | 1 |
| Unemployed, not seeking work | 1 |
| Highest level of education completed, % | |
| Year 11 or below | 8 |
| Year 12 | 10 |
| Certificate I or II | 3 |
| Certificate III or IV | 8 |
| Certificate not further defined | 5 |
| Diploma/advanced diploma | 15 |
| Bachelor's degree or above | 51 |
| Region, % | |
| Sydney | 18 |
| Other New South Wales | 16 |
| Melbourne | 23 |
| Other Victoria | 6 |
| Brisbane | 9 |
| Other Queensland | 8 |
| Adelaide | 7 |
| Other South Australia | 1 |
| Perth | 7 |
| Other Western Australia | ‡ |
| Hobart | 2 |
| Other Tasmania | 1 |
| Australian Capital Territory | 1 |
| Northern Territory | 0 |
Remission was defined as disease being controlled with few to no symptoms.
Small base.
IBD, inflammatory bowel disease; UC, ulcerative colitis.
The mean age of physicians (n = 90) was 49 years (SD 9.9) and 92% were male. Physicians had been in their specialty practice for a mean of 15.9 (SD 9.0) years; 69% practiced in an inflammatory bowel disease center/clinic and saw a mean of 28.2 patients with UC per month.
Burden of disease
Only 30% of patients overall considered their health as “good” or “excellent” and most (97%) reported experiencing a flare in the past 12 months, with an overall mean of 6.5 separate flares. Patients reported their most recent flare to have lasted <1 week (34%), between 7 and 14 days (35%), or >15 days (31%). Of the 65% of patients who self‐reported remission, 95% had experienced a flare in the past 12 months with a mean of 4 separate flares.
Overall, 65% of patients had been hospitalized because of their UC in the past 12 months; 61% of patients who considered themselves in remission had been hospitalized compared with 72% of patients who did not. Most (75%) patients felt they spent more time in the bathroom (to pass stool, air, blood, or mucus) than elsewhere, with a mean of 4.4 (SD 2.5) visits to the bathroom on a good day and 9.1 (SD 5.0) visits on a bad day. Of patients who self‐reported remission, 70% felt they spent more time in the bathroom than elsewhere, with a mean of 4.2 (SD 2.6) visits on a good day and 8.7 (SD 4.9) visits on a bad day. Similarly, of patients who did not view their UC to be in remission, 85% felt they spent more time in the bathroom than elsewhere, with a mean of 4.6 (SD 2.6) visits on a good day and 10.0 (SD 5.2) visits on a bad day.
Current prescription medication and medication satisfaction
Patients' self‐reported current prescription medication for their UC, and their medication satisfaction, are shown in Table 2.
Table 2.
Patient‐reported current prescription medication for their ulcerative colitis (UC) and satisfaction with medication
| Patients in remission† | Current overall health | ||||||
|---|---|---|---|---|---|---|---|
| Overall | Male | Female | Yes | No | Excellent/good | Fair/poor | |
| Current prescription medication, n (%)‡ | |||||||
| Biologic | 21 (37) | 15 (71) | 6 (29) | 15 (71) | 6 (29) | 8 (38) | 13 (62) |
| Immunosuppressant | 19 (33) | 12 (63) | 7 (37) | 10 (53) | 8 (42) | 5 (26) | 14 (74) |
| 5‐aminosalicylates | 12 (22) | 6 (50) | 6 (50) | 8 (67) | 4 (33) | 4 (33) | 8 (67) |
| Corticosteroid | 17 (29) | 9 (53) | 8 (47) | 9 (53) | 7 (41) | 3 (19) | 13 (81) |
| Satisfaction with current prescription medication, n (%) | |||||||
| Very satisfied | 15 (28) | 10 (67) | 5 (33) | 11 (73) | 4 (27) | 6 (40) | 9 (60) |
| Somewhat satisfied | 34 (64) | 21 (62) | 13 (38) | 21 (64) | 12 (36) | 9 (27) | 24 (73) |
| Somewhat dissatisfied | 3 (6) | 1 (33) | 2 (67) | 1 (33) | 2 (67) | 0 (0) | 3 (100) |
| Very dissatisfied | 1 (2) | 1 (100) | 0 (0) | 1 (100) | 0 (0) | 0 (0) | 1 (100) |
| Top reasons for satisfaction, n (%)‡ | |||||||
| Less frequent flares | 26 (54) | 15 (58) | 11 (42) | 17 (65) | 9 (35) | 8 (31) | 18 (69) |
| Less abdominal pain | 23 (47) | 13 (57) | 10 (43) | 15 (65) | 8 (35) | 7 (30) | 16 (70) |
| Less urgency to visit the bathroom | 22 (45) | 13 (59) | 9 (41) | 15 (68) | 7 (32) | 8 (36) | 14 (64) |
Remission was self‐reported by patients and was defined as disease being controlled with few to no symptoms.
Patients could select more than one answer.
Overall current prescription medication: other (n = 3; 6%) and none (n = 4; 7%), data not shown.
Of patients currently taking biologics as their UC medication, 95% were very/somewhat satisfied and 81% wished they had moved to biologics sooner. However, 66% of patients said they were not happy with their biologic medication.
Physicians were more likely to determine patient satisfaction with their current treatment via specific treatment‐related questions (Table 3). Most (92%) physicians agreed that patients with UC who are involved in treatment decisions tend to be more satisfied with their treatment experience than those who are less involved. Most (87%) patients felt they made joint treatment plan decisions with their physician.
Table 3.
How physicians typically determine if their patients are satisfied with their prescription medication regimen
| Question | Proportion of physicians (%) |
|---|---|
| I ask the patient if they are satisfied with the frequency of administration | 88 |
| I ask the patient if they are experiencing any side effects | 86 |
| I ask the patient if they are taking medications as prescribed | 74 |
| I determine based on the symptoms patients describe | 72 |
| I ask the patient directly if they are satisfied or not | 69 |
| I ask the patient if they are satisfied with the mode of administration | 64 |
| I ask the patient how their medication regimen impacts various aspects of their personal life | 63 |
| I ask the patient how they feel before and after initiating the medication | 40 |
| I wait for the patient to tell me if they are satisfied or not | 14 |
Questions: other (1%) and nothing (0%), data not shown. Physicians could select all applicable answers.
Most (76%) patients wished they had more treatment choices, although 75% of patients agreed that if their treatment made them feel “good enough,” they did not see a need to consider other treatment options, even if it might make them feel better.
Both patients and physicians agreed that continued flares and symptoms were the top indicators for considering a change in medication. Assuming equal effectiveness, patients would prefer a daily oral medication (54%) compared with other modes of administration (injection in a medical facility [20%], self‐injection [16%], or infusion [7%]; 2% of patients had no preference).
Knowledge of UC
At diagnosis, 78% of patients wished they had known where to find more information and support. The survey identified gaps in patient knowledge of UC, and for most aspects, physicians recognized the knowledge gaps (Fig. 1).
Figure 1.
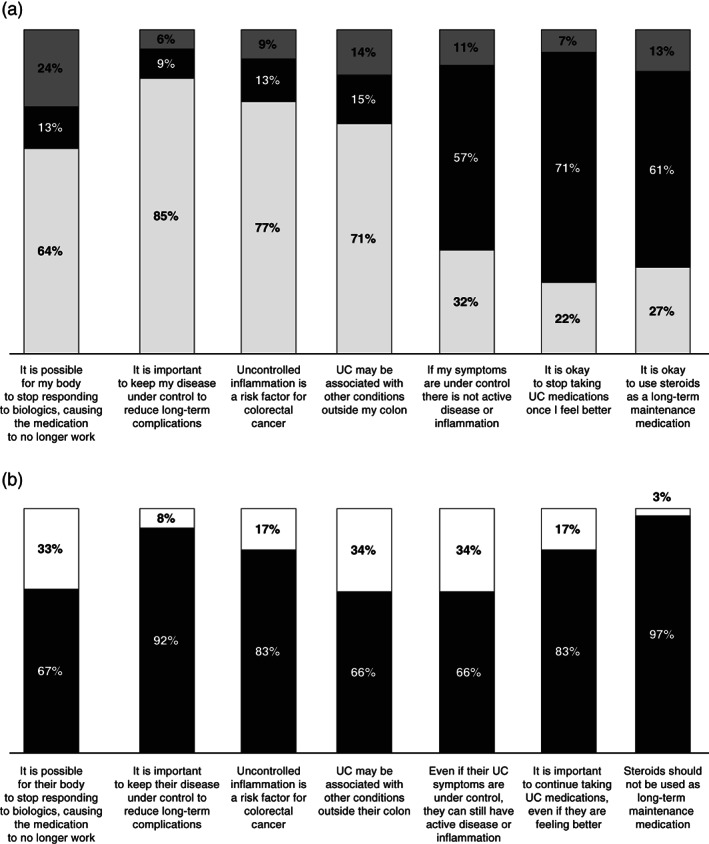
(a) Patient knowledge of ulcerative colitis (UC).  , true;
, true;  , false;
, false;  , not sure. (b) Physicians' perception of patients' knowledge.
, not sure. (b) Physicians' perception of patients' knowledge.  , understand well;
, understand well;  , do not understand well. Due to rounding, the sum of each category may not equal 100%.
, do not understand well. Due to rounding, the sum of each category may not equal 100%.
More patients who did not self‐report remission answered all seven knowledge questions correctly compared with those who did self‐report remission (35% vs 17%).
Communication between patients and physicians
The majority (90%) of patients were satisfied with communication with their physician and, on average, physicians believed 85.5% of their patients were satisfied with communication. Specific aspects of UC management that patients were satisfied with included: discussion of symptoms experienced (88%); prescription medication options (85%); and how current medication may help reach long‐term treatment goals (85%). Despite reporting high satisfaction with communication, patients identified a lack of time as a communication barrier, with 67% wanting more appointment time and 53% feeling that their physician did not have time to address all their concerns. Most (71%) physicians also expressed a desire for more appointment time with their patients. The majority (93%) of physicians believed their patients felt comfortable discussing emotional concerns; however, only 47% of patients said the same. During physician visits, 60% of patients often regretted not telling their physician more, but 60% worried that asking too many questions would result in being seen as difficult and affect quality of care. More male patients than female patients regretted not telling their physician more (66% vs 51%).
A similar proportion of patients (62%) and physicians (65%) wanted more discussions on UC treatment goals; however, a greater proportion of male patients than female patients desired this (73% vs 47%).
The top aspects patients wished their physician better understood about their experiences of living with UC are shown in Figure 2.
Figure 2.
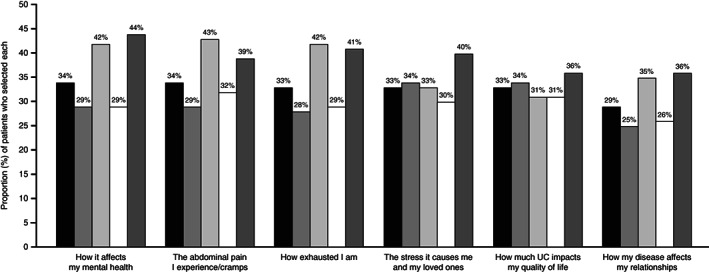
Top aspects of ulcerative colitis (UC) that patients wished their physician better understood about their experiences of living with UC. Patients could select all applicable answers; select responses shown. Remission was self‐reported by patients and defined as disease being controlled with few to no symptoms.  , total;
, total;  , male;
, male;  , female;
, female;  , remission—yes;
, remission—yes;  , remission—no.
, remission—no.
A high proportion (79%) of physicians have taken steps to improve their communication skills (e.g. attended seminars or taken training courses). Items selected by physicians for improving their patient relationships included: providing advice for accessing reliable information (71%); an online tool or smartphone application to monitor and track disease (70%); more information about UC treatment options to provide to patients (62%); having informed resources to provide to patients (59%); and a list for patients of other healthcare professionals who could aid in UC treatment (59%).
Appointment priorities
The top priorities for patients and physicians during routine appointments are shown in Figure 3a. Compared with patients, physicians tended to deprioritize the discussion of cancer risk and new medications available.
Figure 3.
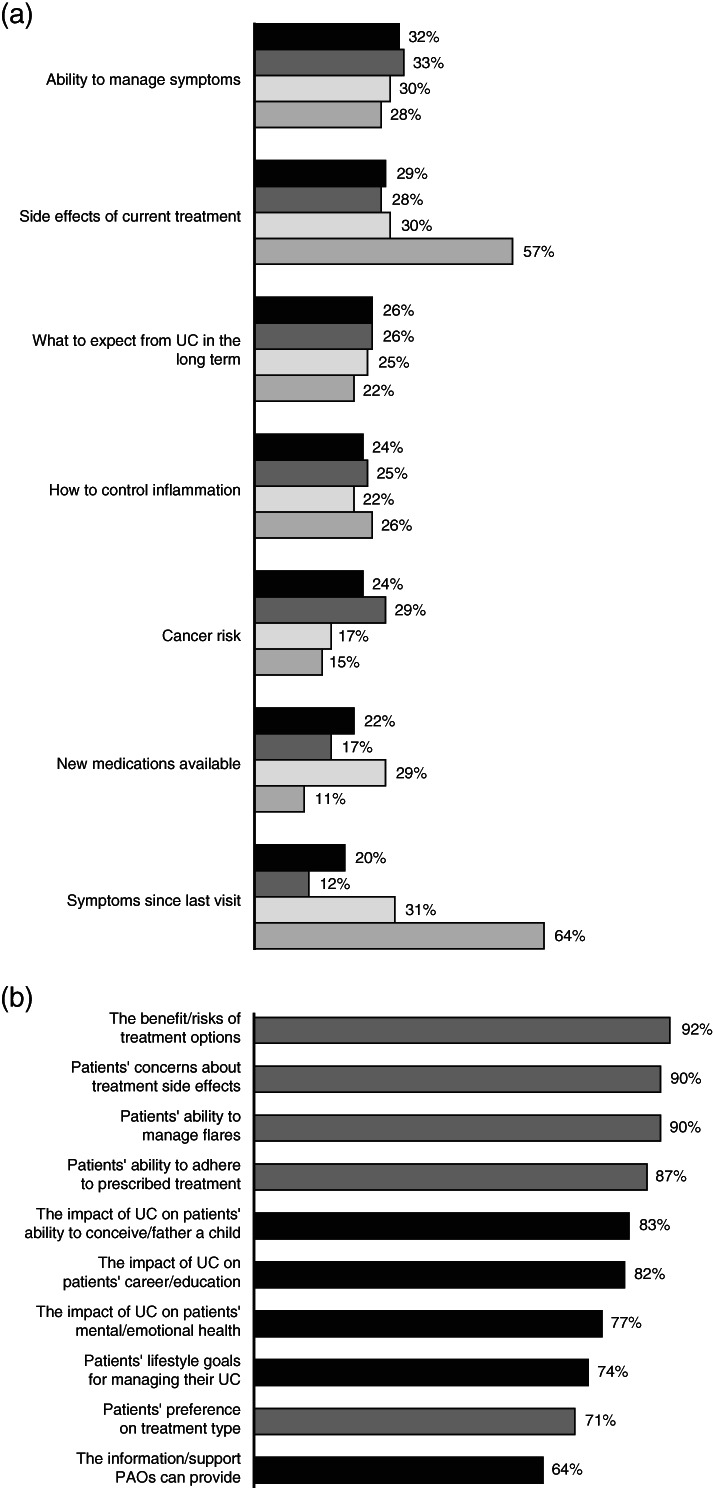
(a) Patient and physician top‐priority topics for discussion during routine appointments, and (b) aspects of ulcerative colitis (UC) management that physicians discuss with patients. (a) Patients and physicians could select up to three answers; select responses shown.  , total patients;
, total patients;  , male patients;
, male patients;  , female patients;
, female patients;  , gastroenterologists. (b) Physicians could select all applicable answers; select responses shown. PAO, patient advocacy organization; QoL, quality of life.
, gastroenterologists. (b) Physicians could select all applicable answers; select responses shown. PAO, patient advocacy organization; QoL, quality of life.  , treatment related;
, treatment related;  , QoL related.
, QoL related.
Aspects of UC management where patients wanted better explanation from their physicians included: how to access information and support from PAOs (28%); what would happen if their treatment failed (25%); benefits/risks of biologics (22%); and the hereditary nature of UC (22%). Physicians were more likely to discuss treatment‐related topics with their patients than quality‐of‐life topics (Fig. 3b).
Information and support
More than half (57%) of the physicians wished there were resources they could refer their patients to for more information and support. Patients (69%) and physicians (84%) agreed on the importance of PAOs in the management of UC. On average, physicians recommended PAOs to 61% of their patients with moderate to severe UC. Only 54% of patients had interacted with a PAO; of these, 30% of patients had been referred to a PAO by their physician, 13% reached out to a PAO for information, and 27% relied on a PAO for information. A high proportion (82%) of patients who had interacted with a PAO wished they had known about them sooner. The same proportion of male and female patients had interacted with a PAO, but more male patients wished they had known about PAOs earlier compared with female patients (88% vs 73%). Approximately one‐third (36%) of physicians never discussed PAOs with their patients, and among those who did, only 75% discussed at diagnosis or initial consultation. A minority (28%) of patients thought their physician could have explained better how to access information and support from PAOs. Information patients said they would be interested in receiving from a PAO is shown in Figure 4.
Figure 4.
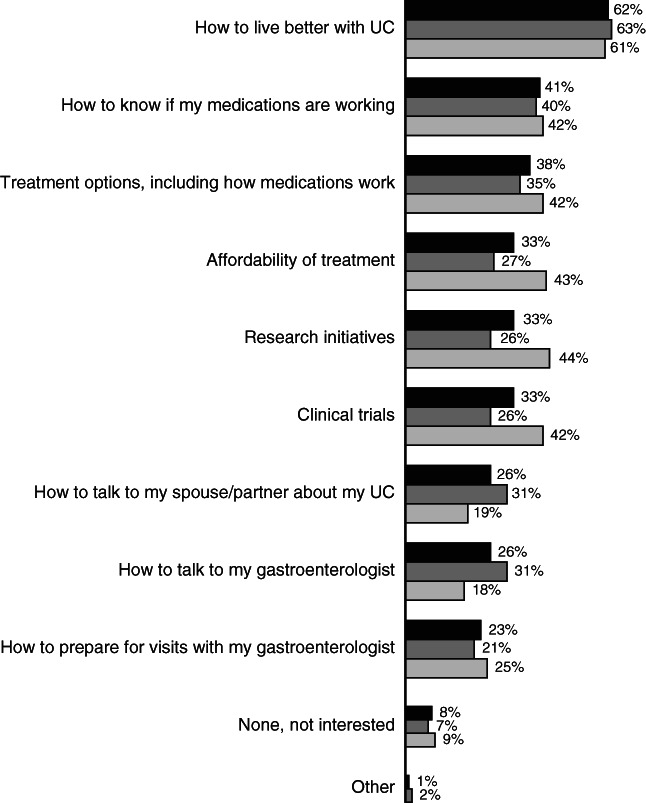
Information patients would be interested in receiving from a patient advocacy organization. Patients could select all applicable responses. UC, ulcerative colitis.  , total;
, total;  , male;
, male;  , female.
, female.
Discussion
Our survey (which was part of the Global UC Narrative Survey) collected information from patients with UC and physicians treating patients with UC in Australia, providing insights into their perceptions of disease burden, treatment, and communication. The principal finding of the survey was the significant burden of UC on patients' lives. Despite many patients considering their UC to be in remission, nearly all (97%) reported they had experienced a flare in the past 12 months. Compared with the overall Global UC Narrative Survey, patients in Australia reported a high burden of disease and this included patients who self‐reported being in remission. Nearly all (97%) patients in Australia reported to have experienced a flare in the past 12 months, with a mean of 6.5 flares during that time. Globally, 87% of patients experienced a flare in the past 12 months and, compared with the other nine countries included in the survey, the mean number of flares experienced was higher in Australia.11 Furthermore, a considerable number of patients in Australia required hospital visits due to their UC.
Patients in Australia reported a mean delay of approximately 2 years between first symptoms and UC diagnosis, consistent with the Global UC Narrative Survey findings11 and data from Finland.10 Diagnostic delay in UC has been associated with poor outcomes such as increased intestinal surgery risk.13
Consistent with other surveys of patients with UC, patients tend to normalize their condition and adapt their lifestyle to accommodate the limitations imposed by their continuing symptoms.14 The proportion of patients who reported satisfaction with their current prescription medication for UC was high, consistent with previously reported data3, 15, 16 and the overall Global UC Narrative Survey results.11 Patients who did not perceive their UC as being in remission reported satisfaction with their current UC prescription medication, further emphasizing the normalization of symptoms and possibly indicating patients' low expectations of medication.
Patients were satisfied with patient–physician communication, although patients and physicians both expressed a desire for greater appointment time. In this survey, physician responses showed that during routine appointments, the emphasis of discussion was on symptom‐related topics rather than quality‐of‐life topics. Similar results were reported from a survey conducted in the United States and Europe, in which the emphasis during patient–physician visits was placed on the quantification of symptoms.17 In this survey, almost all physicians believed their patients felt comfortable to discuss emotional difficulties; however, less than half of patients said they felt comfortable discussing their emotional concerns. Inclusion of discussions surrounding the psychologic and emotional impacts of UC into the management of UC have previously been shown to benefit patients.18, 19
Physicians who completed this survey were a representative sample of Australian gastroenterologists, who are predominantly male with an average age of 49 years.20 Physicians wished they had more reliable information sources that they could refer their patients to. A high proportion (69%) of patients considered PAOs to be an important source of information; this was far greater than in a similar survey of patients with UC in Spain, in which only 16% of patients held this view.21 Globally, only 45% of patients had interacted with a PAO,22 whereas in Australia this figure was numerically higher (54%) but lower than reported from Finland (69.9%).10 Previous studies have reported that those who are members of PAOs are associated with better knowledge23; here, however, patient knowledge did not differ between those who had or had not interacted with a PAO. Various studies have shown that educating patients to be more self‐directed in the management of their disease can have a positive impact on the number of visits to their physician.24, 25 Interestingly, more patients who were not in remission correctly answered all knowledge questions, a finding which agreed with a previous report in which patients with clinically active disease had better disease‐related knowledge.23 A considerable proportion of patients had erroneous beliefs about some aspects of UC, such as the use of steroids for long‐term maintenance treatment.
This study had several limitations; firstly, as this was a patient‐based survey, it was limited by the patients' understanding of the questions and their diagnosis of UC. In this survey, remission and flares were patient‐reported outcomes with less stringent definitions than those used in clinical trials26 and patient severity was based on medication history as opposed to current clinical condition. Additionally, patients completed the survey online; patient participation was, therefore, limited to those with internet access and membership of online panels. Physicians completed the survey online or by telephone, and hence there was potential for interviewer technique/recording to impact upon the results for those surveys completed by telephone. Furthermore, both patient and physician responses relied upon accurate recall and honest reporting.
The results of this survey highlight the burden of UC within Australia, and the normalization of symptoms by patients. There was a generally high level of concordance between Australian patients and physicians in their responses. The findings highlight the importance of patient–physician communication and that, overall, Australian patients have positive relationships with their physicians. Opportunities remain regarding understanding concerns, goal setting, and provision of more information about support at diagnosis, where PAOs could be an important source of additional physician‐recommended information.
Acknowledgments
The authors would like to thank the patients and physicians who were involved in the UC Narrative Survey in Australia. The Global UC Narrative Survey was sponsored by Pfizer Inc. Medical writing support, under the guidance of the authors, was provided by Helen Findlow, PhD, CMC Connect, McCann Health Medical Communications and was funded by Pfizer Inc, New York, NY, USA in accordance with Good Publication Practice (GPP3) guidelines (Ann Intern Med 2015; 163: 461–464).
Declaration of conflict of interest: Susan J. Connor has received honoraria for advisory board participation, speaker fees, educational support, and/or research support from AbbVie, Aspen, Bristol‐Myers Squibb, Celgene, Celltrion, Chiesi, Dr Falk, Ferring, Fresenius Kabi, Gilead, Janssen, MSD, Novartis, Pfizer Inc, Takeda, and Vifor. Alexandra Sechi has been a consultant for Pfizer Inc. Mauricio Andrade, J. Jasper Deuring, and David Witcombe are employees and stockholders of Pfizer Inc.
Author contribution: Study design: The Harris Poll, Global UC Narrative Survey Panel. Statistical analysis: The Harris Poll. Manuscript drafting, critical revision, and final approval: all authors.
References
- 1.Ungaro R, Mehandru S, Allen PB, Peyrin‐Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017; 389: 1756–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jess T, Gamborg M, Munkholm P, Sørensen TIA. Overall and cause‐specific mortality in ulcerative colitis: meta‐analysis of population‐based inception cohort studies. Am. J. Gastroenterol. 2007; 102: 609–17. [DOI] [PubMed] [Google Scholar]
- 3.Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn's and Ulcerative Colitis Associations (EFCCA) patient survey. J. Crohns Colitis. 2007; 1: 10–20. [DOI] [PubMed] [Google Scholar]
- 4.Jones JL, Nguyen GC, Benchimol EIet al. The impact of inflammatory bowel disease in Canada 2018: quality of life. J. Can. Assoc. Gastroenterol. 2019; 2: S42–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng SC, Shi HY, Hamidi Net al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population‐based studies. Lancet. 2017; 390: 2769–78. [DOI] [PubMed] [Google Scholar]
- 6.Studd C, Cameron G, Beswick Let al. Never underestimate inflammatory bowel disease: high prevalence rates and confirmation of high incidence rates in Australia. J. Gastroenterol. Hepatol. 2016; 31: 81–6. [DOI] [PubMed] [Google Scholar]
- 7.Rubin DT, Cleveland NK. Using a treat‐to‐target management strategy to improve the doctor‐patient relationship in inflammatory bowel disease. Am. J. Gastroenterol. 2015; 110: 1252–6. [DOI] [PubMed] [Google Scholar]
- 8.Glass KE, Wills CE, Holloman Cet al. Shared decision making and other variables as correlates of satisfaction with health care decisions in a United States national survey. Patient Educ. Couns. 2012; 88: 100–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lesnovska KP, Börjeson S, Hjortswang H, Frisman GH. What do patients need to know? Living with inflammatory bowel disease. J. Clin. Nurs. 2014; 23: 1718–25. [DOI] [PubMed] [Google Scholar]
- 10.Molander P, Ylänne K. Impact of ulcerative colitis on patients' lives: results of the Finnish extension of a global ulcerative colitis narrative survey. Scand. J. Gastroenterol. 2019; 54: 869–75. [DOI] [PubMed] [Google Scholar]
- 11.Dubinsky MC, Watanabe K, Molander Pet al. Ulcerative Colitis Narrative Global Survey findings: the impact of living with ulcerative colitis – a patients' and physicians' view. Inflamm. Bowel Dis. 2021. Epub ahead of print. https://pubmed.ncbi.nlm.nih.gov/33529314/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kish L. Survey Sampling. New York, NY: John Wiley & Sons, 1965. [Google Scholar]
- 13.Lee DW, Koo JS, Choe JWet al. Diagnostic delay in inflammatory bowel disease increases the risk of intestinal surgery. World J. Gastroenterol. 2017; 23: 6474–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loftus EV Jr. A practical perspective on ulcerative colitis: patients' needs from aminosalicylate therapies. Inflamm. Bowel Dis. 2006; 12: 1107–13. [DOI] [PubMed] [Google Scholar]
- 15.Gray JR, Leung E, Scales J. Treatment of ulcerative colitis from the patient's perspective: a survey of preferences and satisfaction with therapy. Aliment. Pharmacol. Ther. 2009; 29: 1114–20. [DOI] [PubMed] [Google Scholar]
- 16.Carpio D, López‐Sanromán A, Calvet Xet al. Perception of disease burden and treatment satisfaction in patients with ulcerative colitis from outpatient clinics in Spain: UC‐LIFE survey. Eur. J. Gastroenterol. Hepatol. 2016; 28: 1056–64. [DOI] [PubMed] [Google Scholar]
- 17.Rubin DT, Dubinsky MC, Martino S, Hewett KA, Panés J. Communication between physicians and patients with ulcerative colitis: reflections and insights from a qualitative study of in‐office patient‐physician visits. Inflamm. Bowel Dis. 2017; 23: 494–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taft TH, Ballou S, Bedell A, Lincenberg D. Psychological considerations and interventions in inflammatory bowel disease patient care. Gastroenterol. Clin. North Am. 2017; 46: 847–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leone D, Menichetti J, Fiorino G, Vegni E. State of the art: psychotherapeutic interventions targeting the psychological factors involved in IBD. Curr. Drug Targets. 2014; 15: 1020–9. [DOI] [PubMed] [Google Scholar]
- 20.Australian Government Department of Health . Gastroenterology & Hepatology 2016 Factsheet. Australian Government Department of Health. 2016.. Available from URL: https://hwd.health.gov.au/webapi/customer/documents/factsheets/2016/Gastroenterology%20&%20hepatology.pdf. [Google Scholar]
- 21.Argüelles‐Arias F, Carpio D, Calvet Xet al. Knowledge of disease and access to a specialist reported by Spanish patients with ulcerative colitis. UC‐LIFE survey. Rev. Esp. Enferm. Dig. 2017; 109: 421–9. [DOI] [PubMed] [Google Scholar]
- 22.Rubin DT, Hart A, Panaccione Ret al. Ulcerative Colitis Narrative Global Survey findings: communication gaps and agreements between patients and physicians. Inflamm. Bowel Dis. 2021; 27: 1096–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Selinger CP, Carbery I, Warren Vet al. The relationship between different information sources and disease‐related patient knowledge and anxiety in patients with inflammatory bowel disease. Aliment. Pharmacol. Ther. 2017; 45: 63–74. [DOI] [PubMed] [Google Scholar]
- 24.Robinson A, Thompson DG, Wilkin D, Roberts C. Guided self‐management and patient‐directed follow‐up of ulcerative colitis: a randomised trial. Lancet. 2001; 358: 976–81. [DOI] [PubMed] [Google Scholar]
- 25.Kennedy AP, Nelson E, Reeves Det al. A randomised controlled trial to assess the effectiveness and cost of a patient orientated self management approach to chronic inflammatory bowel disease. Gut. 2004; 53: 1639–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sands BE, Cheifetz AS, Nduaka CIet al. The impact of raising the bar for clinical trials in ulcerative colitis. J. Crohns Colitis. 2019; 13: 1217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]


