Figure 2.
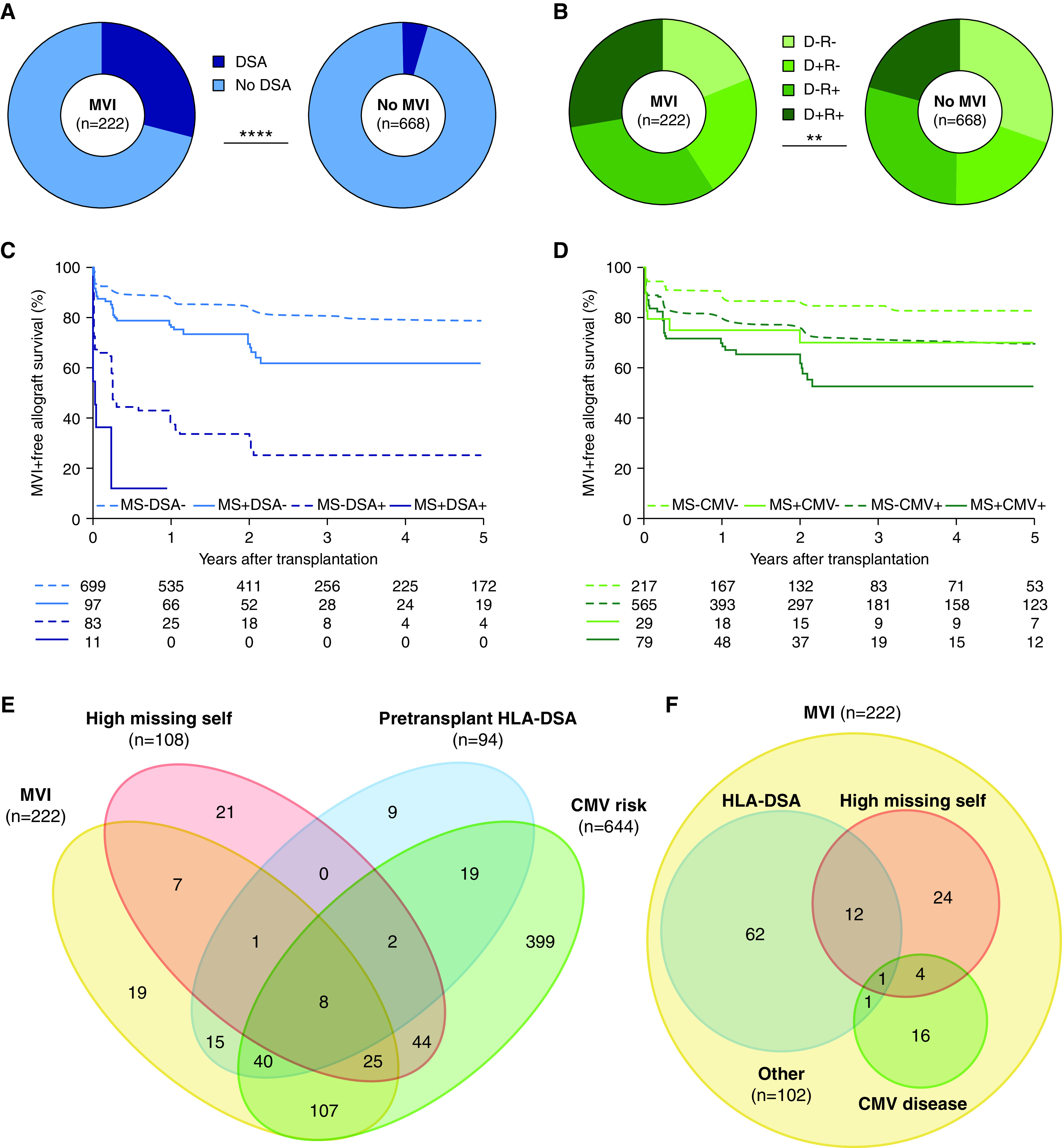
Missing self independently associates with risk of MVI (n=890 transplantations with 3476 post-transplant biopsies). (A) Prevalence of pretransplant HLA-DSA in transplantations with and without MVI during histologic follow-up, chi-squared test for comparison. (B) Pretransplant donor/recipient CMV IgG status in transplantations with and without MVI during follow-up, chi-squared test for comparison. (C) Kaplan–Meier survival curves for incidence of MVI, censored for recipient death and allograft failure, stratified according to high versus low missing self (2–3 versus 0–1 types) and pretransplant HLA-DSA. (D) Survival curves for incidence of MVI, stratified according to high missing self and post-transplant risk for CMV disease (high risk: donor and/or recipient CMV seropositive; low risk: donor and recipient CMV seronegative). (E) Venn diagram depicting the independence of high missing self, pretransplant HLA-DSA and CMV disease risk as pretransplant predictors for MVI (occurring in n=222 transplantations), and the proportion of MVI incidence associated with each predictor. (F) Venn diagram depicting the prevalence of high missing self, prior symptomatic CMV disease and HLA-DSA, either current or previous, at the first moment of diagnosis in the 222 transplantations with MVI. MS, high missing self; +/−, CMV IgG positive/negative. **P<0.01; ****P<0.0001.
