From the authors,
We appreciate Dr. El-Khatib et al.’s comments regarding our article on the “P/FP ratio” [1]. As we all agree [1–3], the ratio of the partial pressure of arterial oxygen (PaO2) to the fraction of inspired oxygen (FiO2), or P/F ratio, can be significantly improved for better reflection of acute respiratory distress syndrome (ARDS) severity by incorporating a wide range of either applied or measured pressures available in an intubated patient.
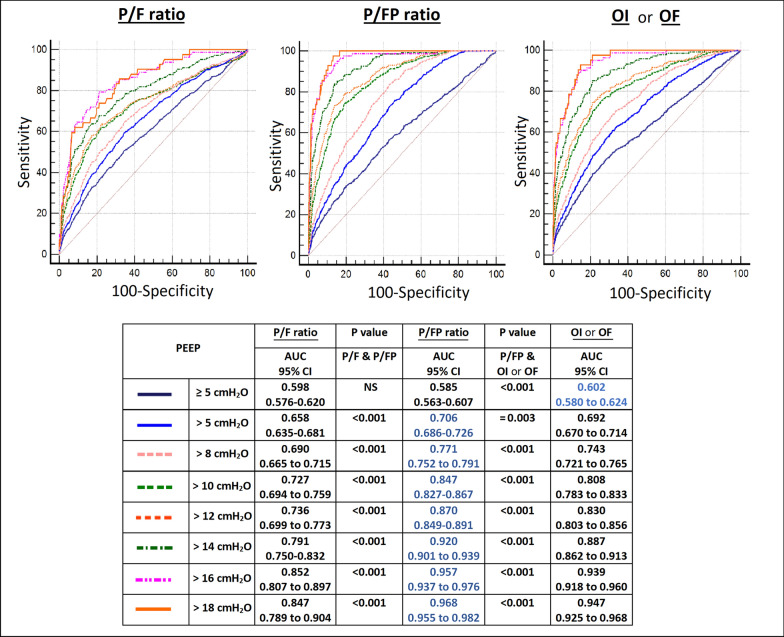
The oxygenation factor (OF) (PaO2/[FiO2*MAP]) proposed and studied by EL Khatib et al. is a reciprocal of the oxygenation index (OI) ([FiO2*MAP]/PaO2) which is often used in paediatric patients. Both indices incorporate mean airway pressure (MAP) into the P/F ratio. While we agree that for the same P/F ratio, a patient with higher MAP may have more severe ARDS than a patient with lower MAP, the use of MAP has several limitations. First, it is a very non-specific variable which is dependent on multiple factors, including tidal volume, inspiratory time, flow, respiratory rate, peak inspiratory pressure, and positive end-expiratory pressure (PEEP). Second, the impact of PEEP on PaO2 is much higher than any of these other variables. Third, when PEEP requirements go up, clinicians usually use various lung-protective strategies to limit alveolar pressure and its surrogate, plateau pressure (to less than 28 to 30 cmH2O)—this in turn limits the rise of MAP. Furthermore, in our dataset of 7 randomized controlled trials using receiver operating characteristics (ROC) curves, we found significantly better predictive validity for hospital mortality with the P/FP ratio compared to the OF or OI and the P/F ratio for different thresholds of PEEP > than 5 cmH2O, as measured by areas under the curves (AUC) (Fig. 1).
Fig. 1.
Receiver operating curves for hospital mortality at different PEEP thresholds for 3191 patients from our study [1], after excluding those with missing mean airway pressure values. Abbreviations: P/F, ratio of the partial pressure of arterial oxygen (PaO2) to the fraction of inspired oxygen (FiO2); P/FP = (PaO2*10)/(FiO2*PEEP); OI, oxygenation index = (FiO2*MAP)/PaO2; OF, oxygenation factor = (PaO2/(FiO2*MAP); PEEP, positive end-expiratory pressure; AUC, area under the curve; CI confidence interval; NS, not significant
We had provided several justifications in our paper for choosing the correction factor of 10 with our P/FP ratio. These include previous suggestions to use an applied PEEP of ≥ 10 cmH2O as an initial standardized ventilator setting for ARDS, and our own analysis of a regression line of PEEP versus P/F ratio in our dataset which found a clear intersection of a PEEP of 10 cmH2O and a P/F ratio of 150 mmHg, a value midway between 0 and 300 mmHg. The correction factor of 10 brings the values of the P/FP ratio to a range similar to that of the P/F ratio, which clinicians are already familiar with. For example, for a patient with a P/F ratio of 150 mmHg and a PEEP of 10 cmH2O, a correction factor of 10 would result in a P/FP ratio of (150/10)*10 = 150 mmHg/cmH2O. A correction factor of 5 would result in a P/FP ratio of (150/10)*5 = 75 mmHg/cmH2O, thus potentially giving clinicians a false impression of greater severity than is actually the case. A correction factor of 15 would result in a P/FP ratio of (150/10)*15 = 225 mmHg/cmH2O, thus potentially giving clinicians a false impression of milder severity than is actually the case. On the other hand, for a patient with a P/F ratio that is spuriously low at 150 mmHg as a result of an insufficient PEEP of 5 cmH2O, a correction factor of 10 would result in a P/FP ratio of (150/5)*10 = 300 mmHg/cmH2O, thus giving a better picture of the actual severity (or rather, lack thereof). In sum, the correction factor of 10 can be applied to any level of PEEP.
There is a wide variation in the practice of choosing PEEP globally. Although the concept of personalized PEEP settings continues to generate much interest, our study shows that the simple multifactorial P/FP ratio is significantly better able to predict mortality for ARDS than other related indices and ratios. As our study and El-Khatib et al.'s demonstrate, the P/F ratio needs to be revisited for better classification and prognostication of ARDS.
Acknowledgements
None.
Authors' contributions
SP wrote the first draft of the manuscript. JP, AM and CH edited and approved. All authors have read and approved the final manuscript.
Funding
None.
Availability of data and materials
ARDS network trials mentioned in our article [1].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Palanidurai S, Phua J, Chan YH, Mukhopadhyay A. P/FP ratio: incorporation of PEEP into the PaO2/FiO2 ratio for prognostication and classification of acute respiratory distress syndrome. Ann Intensive Care. 2021;11:124–132. doi: 10.1186/s13613-021-00908-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Khatib MF, Jamaleddine GW. A new oxygenation index for reflecting intrapulmonary shunting in patients undergoing open heart surgery. Chest. 2004;125(2):592–596. doi: 10.1378/chest.125.2.592. [DOI] [PubMed] [Google Scholar]
- 3.El-Khatib MF, BouAkl IJ, Ayoub CM, Chatburn RL, Farhat H, Msheik M, Fakih MH, Hallal AH. Comparison of the oxygenation factor and the oxygenation ratio in subjects with ARDS. Respir Care. 2020;65(12):1874. doi: 10.4187/respcare.07669. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
ARDS network trials mentioned in our article [1].