Figure 3. Potential Mechanisms of Inflammatory Syndromes Associated With SARS-CoV-2.
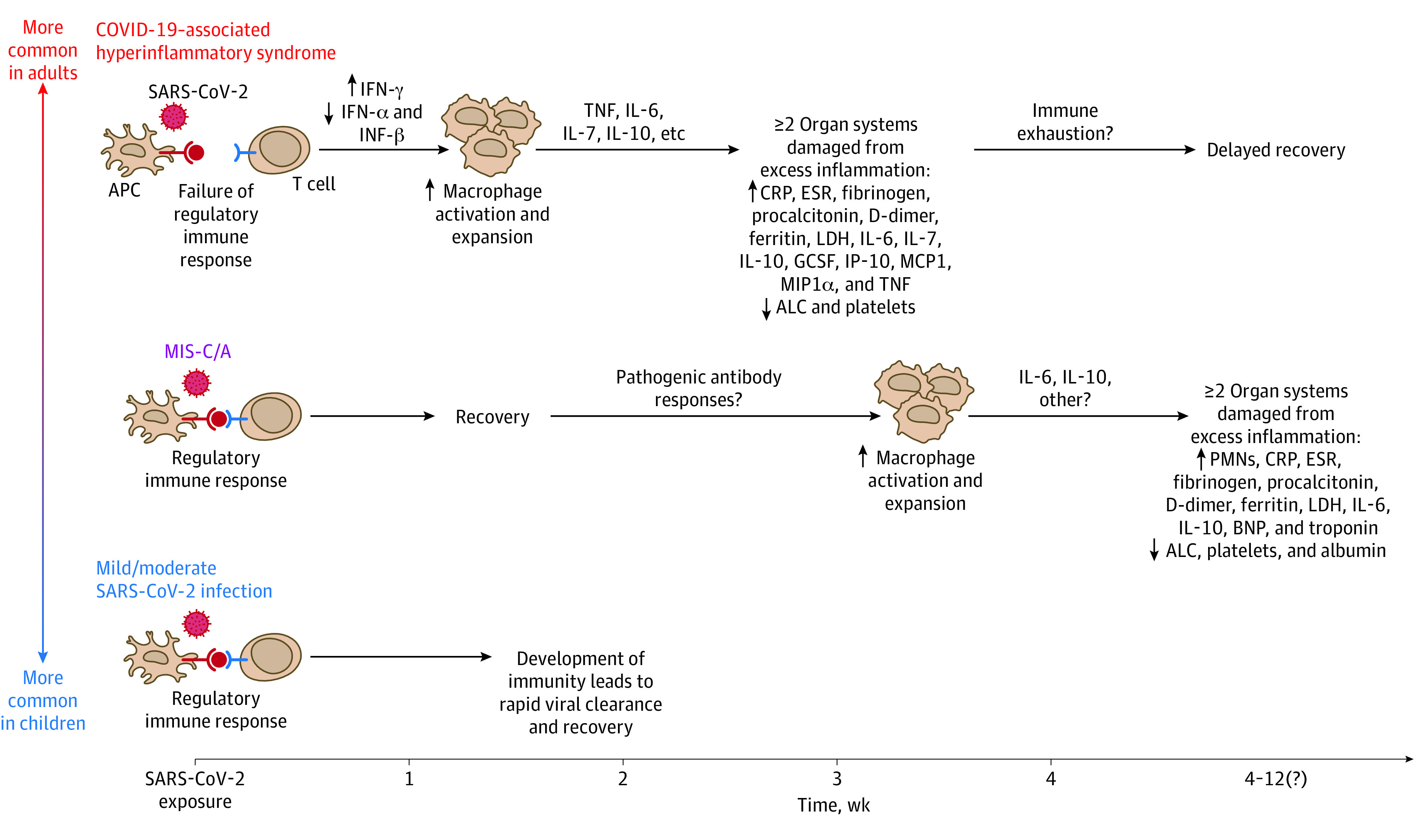
SARS-CoV-2 can trigger a range of inflammatory syndromes across the age spectrum. Compared with children, adults—particularly those with certain preexisting proinflammatory comorbidities—are more likely to develop acute COVID-19–associated hyperinflammatory syndrome within 1 to 2 weeks of exposure to SARS-CoV-2. COVID-19–associated hyperinflammatory syndrome begins with failure of the regulatory immune response to SARS-CoV-2, including abnormal interferon (INF) production that drives macrophage hyperactivation. This results in inflammatory cytokine cascades and causes significant damage to multiple organ systems. In contrast, children are more likely to have asymptomatic or mild acute SARS-CoV-2 infection without sequelae. The reason(s) why children do not commonly develop acute COVID-19–associated hyperinflammatory syndrome remains unknown. However, both children and adults can develop a multisystem inflammatory syndrome (MIS-C/A) of unclear etiology weeks after initial asymptomatic or mild SARS-CoV-2 infection. The precise cause of MIS-C/A remains unclear but may be due to development of abnormal antibody responses that drive systemic hyperinflammation.81 ALC indicates absolute lymphocyte count; APC, antigen-presenting cell; BNP, B-type natriuretic peptide; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; GCSF, granulocyte colony-stimulating factor; IL, interleukin; IP-10, human interferon-inducible protein 10; LDH, lactate dehydrogenase; MCP, monocyte chemotactic protein; MIP, macrophage inflammatory protein; PMN, polymorphonuclear leukocyte; and TNF, tumor necrosis factor. Reproduced with permission from Prathit Arun Kulkarni (Weatherhead et al83) on December 20, 2020.
