Abstract
Purpose
The COVID-19 pandemic and efforts to slow the spread of disease have particularly affected the lives of adolescents. Many studies have recently identified the risks to adolescent mental health posed by the COVID-19 pandemic, yet few have identified the markers of resilience to the events and concerns associated with the pandemic's lived experience. This study examined the moderating role of psychosocial resources in the association between the tangible and emotional experiences of the COVID-19 pandemic and symptoms of common psychiatric problems during adolescence (depression, anxiety, proactive and reactive aggression, and sleep problems).
Methods
Participants were adolescents in the United States who were oversampled for early life adversity before the COVID-19 pandemic. The psychosocial resources assessed were humor styles, emotion regulation, social support, optimism, and purpose in life, which have previously been identified as protective in the acute aftermath of stressful events.
Results
Greater COVID-19 impact was associated with more anxiety, depressive symptoms, sleep disturbance, and proactive aggression. COVID-19 impact and psychiatric symptoms were unrelated among youth reporting high self-enhancing humor and cognitive reappraisal.
Conclusions
Adolescents high in humor and cognitive reappraisal may be protected against the mental health correlates of the COVID-19 pandemic and other prolonged stressors. Importantly, these factors are known to be modifiable through behavioral interventions. Attention to their effectiveness in prevention and intervention studies is needed as the pandemic continues to exert its impact on individuals and society.
Keywords: COVID-19, Community-level stressors, Resilience, Cognitive reappraisal, Humor, Sleep, Proactive aggression, Developmental psychopathology
Implications and Contribution.
The COVID-19 pandemic has impacted most adolescents, although what explains which adolescents will experience psychiatric symptoms in its wake remains unknown. Humor and cognitive reappraisal may be sources of psychological resilience for youth impacted by COVID-19 and other prolonged stressors.
Modern pandemics, such as those caused by COVID-19, H1N1, AIDS, and Ebola, have been followed by prolonged psychiatric symptoms in youth, such as posttraumatic stress, anxiety, and depression [1]. The stressors specific to a pandemic (i.e., concern for your own health and that of your loved ones) are also associated with elevated need for psychiatric care [2]. Furthermore, the social distancing precautions enacted to slow the spread of the coronavirus may be particularly challenging for adolescents [3,4], including school closures, stay-at-home orders that impede peer relationships, and postponement/cancelation of life events. The purpose of the present study was to determine the extent to which COVID-19 impact was associated with psychiatric symptoms among adolescents and to identify modifiable sources of resilience that may be leveraged as this pandemic continues to impact individuals and society.
While the psychiatric consequences of pandemics are well-documented, few studies have documented psychosocial resources that can be modified through psychosocial interventions and may help reduce the mental health impact of the COVID-19 pandemic for adolescents. Modifiable psychosocial resources, such as optimism [5], purpose in life [6,7], cognitive reappraisal skills [8,9], social support [10,11], and humor [12], have been identified as protective in the acute aftermath of stressful experiences among adults. Specifically, higher social support [13] and cognitive reappraisal [14] have been identified as protective during COVID-19. Whether these resources have similar protective potential among vulnerable adolescents, such as those at risk for psychopathology, is unknown. Indeed, there is overwhelming evidence that many adolescents are experiencing elevated psychiatric distress in the wake of the COVID-19 pandemic [15,16], with adolescents exposed to early life adversity (ELA) among the most vulnerable [[17], [18], [19]]. In order to address these gaps in the literature, we assessed the impact of the COVID-19 pandemic (both events and concerns), psychiatric symptoms, and modifiable psychosocial resources among adolescents (aged 11–18 years) oversampled for risk for psychopathology by virtue of elevated ELA. See Figure 1 for a conceptual model.
Figure 1.
Conceptual model for psychological resources as potential modifiers of the association between COVID-19 impact and psychiatric symptoms.
Method
Participants
Participants in this study were 88 youth aged 11–18 years (M = 14.99 ± 1.84; 48.9% female) recruited from within our internal laboratory database. Families in our database were initially recruited for a prospective, longitudinal study of adolescent-onset depression via mass mailing using household contact information. Household contact information came from the 2015 Census conducted by the United States government to systematically enumerate the population. The mass mailing targeted families in Los Angeles and Orange Counties, California, who were likely to have a child between the ages of 12–15 years and oversampled from zip codes with poverty rates at or exceeding the national median given the robust association between ELA and risk for psychopathology. This sample was diverse, reflecting the Southern California region, such that 50.5% identified as non-Hispanic white, 33% Hispanic/Latino, 12% Asian, and 7% Black/African American (Groups are not mutually exclusive [e.g., participants identifying as both Hispanic/Latino and black].); 66% of families owned their home; 19.5% of youth had parents both with a graduate degree; and 47% of youth had parents both without a college degree. After receiving an invitation letter, interested parents contacted the laboratory to complete a brief phone interview assessing their child's demographic, ELA, and health information. ELA was measured via parent report on a modified version of the Adverse Childhood Experiences questionnaire which evaluated their child's exposure to extreme poverty, physical neglect, emotional abuse, parental mental illness or substance abuse, parent divorce or separation, death of a close person, parent incarceration, and serious personal injury using aggregate-item screening [20,21]. For protection of human subjects, only a total score on the Adverse Childhood Experiences was recorded, and no reliability can be computed. At the end of the interview, parents were asked whether they wished to be included in a database to be contacted for future studies.
Procedures
Parents in our database were contacted via email for the present study. The email explained the goals of the present study and included a link to a consent form in Qualtrics. After reviewing the consent form, parents provided the name, email, and phone number of the child for whom they were providing consent. Youth whose parents provided consent were contacted via email or text message with an invitation to participate via a link to the assent form and survey. The 88 youth in the final analytic sample represent 71.5% of the 123 youths invited to participate. Eighteen children in the sample were siblings of other participants. Data collection for this study occurred between June 22nd and August 11th, 2020, although the vast majority of our analytic sample (73%) completed the survey within the first 2 weeks of data collection. Youth had the option of completing the survey across multiple sittings: Eighty percent of respondents completed the survey within 1 hour, and 92% completed the survey on the same day they started. Youth were compensated with a $10 gift card to Target. All study procedures were approved by the Institutional Review Board at the University of California Irvine.
Measures
COVID-19 impact
Pandemic impact was measured by combining scores from two different subscales from the COVID-19 Adolescent Symptom and Psychological Experience questionnaire [22]: COVID-19 events and COVID-19-related concern. In the 13-item COVID-19 events scale, youth reported whether any of the following had happened in their household during the past two weeks: parent or personal job loss, parent or personal change in work hours, difficulty paying bills or buying necessities, parent unemployment, family applied for public assistance, or food insecurity. Participants also reported whether they or anyone in their immediate social network had been infected or died. “Yes” responses were summed. Internal consistency across COVID-19 events was low, α = .34, suggesting that COVID-19 has impacted youth in our sample in widely variable ways. COVID-19-related concern was assessed using 18 items. For each item, youth were asked, “How concerned are you about the impact of COVID-19 on the following …” during the past two weeks. The response scale was a 6-point scale from 1 “Not at all” to 6 “Extremely.” Examples of these 18 items included getting infected, missing important events, conflict between parents, and not getting into college. COVID-19 concern exhibited good internal reliability, α = .80. These concern items were included as a part of COVID-19 impact because the tangible events related to the pandemic (job loss, death of a loved one) may be meaningful but of low frequency in many populations, and limiting our measure of COVID-19 impact to these events would be a gross underestimation of the adolescent experience over the past year. While a high average score on distress may reflect a risk factor, such as the tendency toward negative affect, a teen reporting that they have been “Extremely” concerned about “Family might get sick” or “Missing events that were important to me (e.g., graduation)” is not a psychiatric problem. The psychiatric concern lies in which teens will experience prolonged and generalized distress as was assessed via clinically validated outcome measures. Both COVID-19-related events and COVID-19-related concern were converted to z-scores and averaged to create a single index of COVID-19 impact.
Primary outcomes
Psychiatric symptoms were measured using four validated self-report questionnaires. Table 1 includes possible and observed ranges for all measures. Depressive symptoms were measured via the Reynolds Adolescent Depression Scale second edition. This is a 30-item measure, and scores > 77 indicate a likely depressive episode. The Reynolds Adolescent Depression Scale second edition demonstrated excellent internal reliability in this sample, α = .93. Anxiety symptoms were measured using the Screen for Childhood Anxiety and Related Emotional Disorders. This is a 41-item measure, and scores > 25 indicate a likely anxiety disorder. The Screen for Childhood Anxiety and Related Emotional Disorders demonstrated excellent internal reliability in this sample, α = .95. Proactive and reactive aggression were measured via the 23-item Reactive and Proactive Aggression Questionnaire. The Reactive and Proactive Aggression Questionnaire demonstrated acceptable internal reliability for reactive aggression in this sample, α = .76, and good internal reliability for proactive aggression, α = .86. Sleep disturbance was measured via the Pittsburgh Sleep Quality Index (PSQI). The PSQI is an 18-item self-report questionnaire assessing subjective sleep quality, sleep efficiency, sleep latency, sleep duration, types of sleep disturbances (e.g., urination, environmental noise, bed partner restlessness), use of medications, and daytime functioning over the past month. The PSQI global score is a sum of the impaired sleep domains. Scores > 5 indicate clinically meaningful sleep disturbances. Internal reliability of the PSQI global score was fairly low in this sample, α = .60, but comparable to that of other adolescent samples [23]. Importantly, several impaired sleep domains are uncommon among adolescents, thus undermining internal reliability.
Table 1.
COVID-19 impact, psychiatric symptoms, and potential moderators among adolescents
| Measure | Possible range | Observed range | M (SD) | % Above clinical threshold |
|---|---|---|---|---|
| Age | — | 11–18 | 14.99 (1.84) | |
| Early life adversity (ACEs) | 0–10 | 0–9 | 2.18 (1.81) | 21.3 |
| Independent variables | ||||
| COVID-19 events | 0–12 | 0–4 | .97 (.75) | |
| COVID-19 concern | 1–6 | 1.24–5.11 | 2.67 (.72) | |
| Overall COVID-19 impact (z-score) | – | −1.64–2.86 | −.01 (.78) | |
| Primary outcomes | ||||
| Depressive symptoms | 30–120 | 32–88 | 55.48 (15.25) | 12.4 |
| Anxiety symptoms | 0–82 | 1–55 | 20.39 (14.46) | 34.8 |
| Reactive aggression | 0–22 | 0–15 | 6.34 (3.38) | |
| Proactive aggression | 0–24 | 0–12 | 1.29 (2.45) | |
| Sleep disturbance | 0–21 | 0–13 | 4.28 (2.82) | 27.3 |
| Moderators | ||||
| Affiliative humor | 8–56 | 24–56 | 44.55 (7.71) | |
| Self-enhancing humor | 8–56 | 13–52 | 36.00 (8.22) | |
| Cognitive reappraisal | 1–7 | 1.33–7.00 | 4.58 (1.15) | |
| Optimism | 0–24 | 0–24 | 10.34 (4.58) | |
| Purpose in life | 6–30 | 9–30 | 22.67 (4.64) | |
| Giving social support | 1–6 | 1.6–6 | 4.64 (1.05) | |
| Receiving social support | 1–6 | 1.6–6 | 4.73 (1.24) |
ACE = Adverse Childhood Experiences; M = mean; SD = standard deviation.
Moderators
Modifiable psychosocial resources were measured using five validated self-report questionnaires.
Cognitive reappraisal
Youth completed the Emotion Regulation Questionnaire [24], which included a 6-item subscale assessing cognitive reappraisal. Cognitive reappraisal is a strategy for altering emotional experience by reframing or changing the way a person thinks about a stimuli or situation. For each item, respondents indicated their agreement with statements describing ways they regulate their emotions according to a 7-item Likert-type scale from 1 “Strongly disagree” to 7 “Strongly agree.” Scores in each domain were averaged, and higher scores indicated more cognitive reappraisal. Cognitive reappraisal showed good internal reliability in this sample, α = .85.
Humor
Youth completed two subscales from the Humor Styles Questionnaire that measured adaptive uses of humor [25]: self-enhancing and affiliative humor. Self-enhancing humor is the tendency to try to find humor in everyday situations and make oneself the target of the humor in a good-natured way. Affiliative humor is the tendency to use humor to bring people together and create inclusiveness. Both subscales included eight items describing a way they use humor to which respondents indicated their agreement according to a 7-item Likert-type scale from 1 “Totally disagree” to 7 “Totally agree.” Higher scores indicated more frequent use of each humor style. Both self-enhancing and affiliative humor showed good internal reliability in this sample, α = .81 and α = .83, respectively.
Optimism
Youth self-reported optimism via the Life Orientation Test [26]. This is a 10-item questionnaire of which responses to six items are summed to compute an index of optimism. For each item, respondents indicated their agreement with each statement according to a 5-point scale from 0 “I disagree a lot” to 4 “I agree a lot.” Higher values indicated higher optimism. Optimism demonstrated acceptable internal reliability in this sample, α = .78.
Purpose in life
Youth self-reported purpose in life via the 6-item Life Engagement Test, which assesses the extent to which a person engages in activities that are personally valued [27]. Respondents were asked to indicate the extent of their agreement with each statement according to a 5-point scale from 1 “Strongly disagree” to 5 “Strongly agree”. Higher scores indicated greater life engagement or purpose in life. Purpose in life demonstrated good internal reliability in this sample, α = .84.
Social support
Youth reported social support via responses to the Giving and Receiving Emotional Support subscales of the Two-way Social Support Scale [28]. Each subscale included six items. For each item, respondents indicated how true each statement is for them using a 6-point scale from 0 “Not at all true” to 5 “Always true.” Scores for all items within each subscale were averaged. Higher scores indicated higher support given or received in each domain. Both subscales demonstrated excellent internal reliability in this sample, receiving α = .95 and giving α = .91.
Data analysis
All data analysis was conducted in SPSS version 25. All continuous variables were assessed for normality and found to meet the assumptions required for parametric statistics. We used regression to test whether our eight modifiable psychological resources moderated the association between COVID-19 impact and psychiatric symptoms using the PROCESS Macro [29]. To determine the reliability of associations between COVID-19 impact and each outcome at varying levels of each moderator, we used bootstrap resampling to compute the conditional association between COVID-19 and each outcome at low (-1SD), average, and high (+1SD) scores for each moderator. Given the nonindependence issue raised by having siblings in our data set, we also applied all our significant models with one randomly selected participant from each family (n = 70), which did not change the pattern or interpretation of any results. All analyses accounted for age, sex, and ELA. In order to facilitate comparison with other studies, all statistical tests in which p < .05 are reported, but a p < .001 corrects for multiple comparisons and should be considered significant and reliable.
Results
In addition to state-mandated school closures, adolescents reported experiencing a wide range of events and concern associated with the COVID-19 pandemic, as well as a range of psychiatric symptoms. At the time of assessment (Summer 2020), almost a third (29.2%) of the sample reported knowing a person who had been infected with the virus, 9.1% reported knowing someone who died of COVID-19, and a quarter (24.8%) reported that their parents were either working longer or shorter hours as a result of the pandemic. Across the psychiatric domains measured, nearly half (48.4%) of the sample reported symptoms in a clinical range (Table 1). After accounting for age, sex, and ELA, higher COVID-19 impact was associated with more depressive symptoms, b = 5.82 (standard error [SE] = 2.03), p = .005; more anxiety, b = 5.23 (SE = 1.98), p = .010; more proactive aggression, b = .87 (SE = .36), p = .019; and more severe sleep disturbance, b = .92 (SE = .42), p = .031. Greater COVID-19 impact was not associated with reactive aggression, b = .35 (SE = .52), p = .50.
Humor
Table 2 provides the estimated associations between COVID-19 impact and each clinical outcome at low (-1SD), average, and high (+1SD) values of each moderator. Affiliative humor moderated the association between COVID-19 impact and both proactive aggression, b = -.12 (SE = .04), p = .002, and sleep, b = -.13 (SE = .05), p = .006. Specifically, higher COVID-19 impact was only associated with more proactive aggression among adolescents with low, p = .0008, but not average or high affiliative humor, p ≥ .19. Higher COVID-19 impact was only associated with more sleep problems among adolescents with low, p = .001, but not average or high affiliative humor, p ≥ .16. Affiliative humor did not moderate the association between COVID-19 impact and depressive or anxiety symptoms, p ≥ .19.
Table 2.
Coefficient estimates of the association between COVID-19 impact and psychiatric symptoms by psychological resource
| Moderator |
Depressive symptoms (RADS-2) |
Anxiety symptoms (SCARED) |
Reactive aggression (RPQ-R) |
Proactive aggression (RPQ-p) |
Sleep disturbances (PSQI) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| b (SE) | 95% CI | b (SE) | 95% CI | b (SE) | 95% CI | b (SE) | 95% CI | b (SE) | 95% CI | |
| Cognitive reappraisal | ||||||||||
| High | 1.00 (2.65) | −4.27–6.27 | −.0004 (2.69) | −5.35–5.35 | −.40 (.76) | −1.90–1.10 | −.47 (.49) | −1.44–.51 | −.60 (.55) | −1.70–.50 |
| Average | 6.34 (1.78)∗ | 2.79–9.89 | 5.64 (1.81) + | 2.04–9.25 | .42 (.51) | −.59–1.43 | .03 (.93) + | .27–1.59 | 1.01 (.37) + | .26–1.75 |
| Low | 11.69 (2.69)∗ | 6.32–17.05 | 11.29 (2.73)∗ | 5.84–16.73 | 1.24 (.77) | −.29–2.77 | 2.32 (.50)∗ | 1.33–3.32 | 2.62 (.56)∗ | 1.50–3.73 |
| Self-enhancing humor | ||||||||||
| High | 2.05 (2.76) | −3.44–7.54 | 3.39 (2.83) | −2.26–9.03 | .31 (.75) | −1.17–1.80 | −.28 (.48) | −1.23–.67 | −.13 (.58) | −1.29–1.04 |
| Average | 7.08 (1.95)∗ | 3.20–10.96 | 5.89 (2.00) + | 1.90–9.88 | .46 (.53) | −.59–1.51 | 1.15 (.34)∗ | .47–1.82 | 1.13 (.41) + | .31–1.96 |
| Low | 12.11 (3.24)∗ | 5.66–18.57 | 8.39 (3.33) + | 1.76–15.02 | .61 (.88) | −1.14–2.35 | 2.57 (.56)∗ | 1.45–3.69 | 2.40 (.69)∗ | 1.03–3.76 |
| Affiliative humor | ||||||||||
| High | 3.00 (3.02) | −3.01–9.01 | 1.96 (3.00) | −4.02–7.94 | −.13 (.79) | −1.70–1.45 | −.46 (.49) | −1.43–.51 | −.42 (.61) | −1.64–.81 |
| Average | 4.67 (2.06)+ | .57–8.78 | 4.27 (2.05) + | .18–8.35 | .18 (.54) | −.90–1.25 | .44 (.33) | −.22–1.10 | .59 (.42) | −.25–1.43 |
| Low | 6.35 (2.37) + | 1.63–11.07 | 6.57 (2.36) + | 1.88–11.27 | .48 (.62) | −.76–1.71 | 1.33 (.38)∗ | .57–2.09 | 1.60 (.48) ∗ | .64–2.56 |
| Optimism | ||||||||||
| High | 6.40 (2.34) + | 1.74–11.06 | 5.58 (2.42) + | .77–10.39 | −.10 (.71) | −1.32–1.51 | 1.08 (.50) + | .08–2.08 | .88 (.56) | −.23–1.99 |
| Average | 4.23 (1.75) + | .75–7.70 | 3.89 (1.80) + | .30–7.49 | .30 (.53) | −.76–1.36 | .82 (.37) + | .07–1.57 | .75 (.42) | −.08–1.58 |
| Low | 2.05 (2.57) | −3.08–7.18 | 2.20 (2.66) | −3.09–7.50 | .50 (.78) | −1.06–2.06 | .56 (.55) | −.54–1.66 | .62 (.61) | −.60–1.85 |
| Purpose in life | ||||||||||
| High | 2.51 (2.64) | −2.74–7.77 | 2.92 (3.10) | −3.26–9.10 | 1.02 (.85) | −.67–2.71 | .04 (.59) | −1.15–1.22 | .22 (.65) | −1.07–1.51 |
| Average | 3.41 (1.71) + | −.003–6.82 | 3.73 (2.01) | −.29–7.74 | .41 (.55) | −.69–1.51 | .57 (.39) | −.20–1.34 | .54 (.42) | −.30–1.38 |
| Low | 4.30 (1.91) + | .49–8.12 | 4.53 (2.25) + | .04–9.01 | −.20 (.62) | −1.43–1.03 | 1.11 (.43) + | .25–1.97 | .86 (.47) | −.07–1.80 |
| Social support (giving) | ||||||||||
| High | 5.43 (2.61) + | .24–10.63 | 4.45 (2.60) | −.73–9.64 | .07 (.68) | −1.29–1.43 | .39 (.47) | −.55–1.33 | .69 (.53) | −.36–1.74 |
| Average | 5.92 (2.00) + | 1.95–9.90 | 5.36 (1.99) + | 1.39–9.33 | .40 (.52) | −.65–1.44 | .94 (.36) + | .22–1.65 | .96 (.40) | .16–1.77 |
| Low | 6.41 (2.90) + | .64–12.19 | 6.26 (2.90) + | .49–12.03 | .72 (.76) | −.79–2.24 | 1.48 (.52) + | .44–2.52 | 1.24 (.59) + | .07–2.40 |
| Social support (receiving) | ||||||||||
| High | −.10 (2.59) | −5.27–5.06 | 2.86 (2.98) | −3.08–8.80 | .68 (.80) | −.91–2.28 | −.01 (.53) | −1.07–1.05 | −.08 (.60) | −1.29–1.12 |
| Average | 2.72 (1.77) | −.79–6.24 | 3.80 (2.03) | −.24–7.83 | .28 (.54) | −.80–1.37 | .49 (.36) | −.23–1.21 | .45 (.41) | −.37–1.27 |
| Low | 5.55 (1.99) + | 1.58–9.52 | 4.73 (2.29) + | .17–9.29 | −.12 (.61) | −1.34–1.11 | .99 (.41) + | .17–1.80 | .98 (.46) + | .05–1.90 |
Bold values indicate statistical significant effect correcting for multiple comparison. ∗p < .001, +p < .05.
CI = confidence interval; PSQI = Pittsburgh Sleep Quality Index; RADS-2 = Reynolds Adolescent Depression Scale second edition; RPQ = Reactive and Proactive Aggression Questionnaire; SCARED = Screen for Childhood Anxiety and Related Emotional Disorders; SE = standard error.
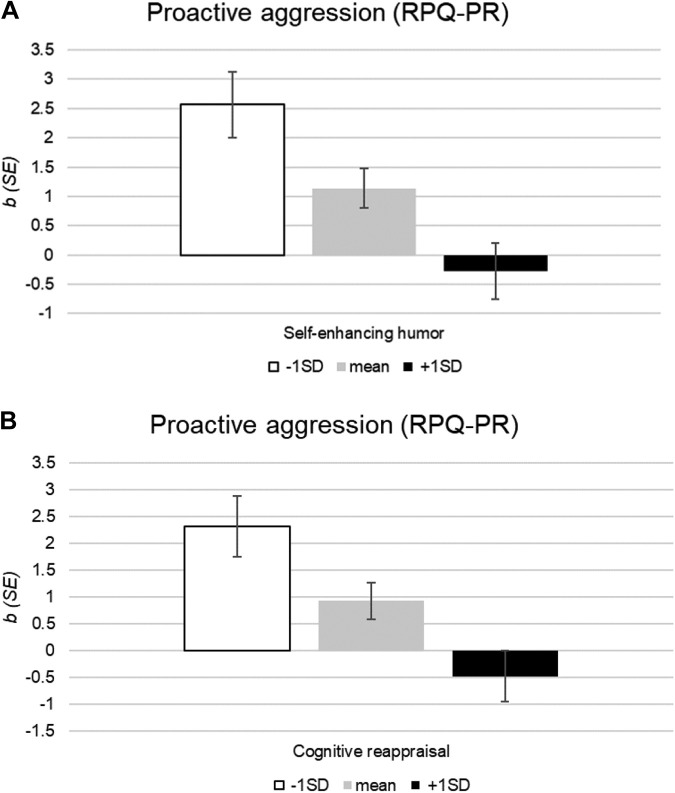
Self-enhancing humor moderated the association between COVID-19 impact and depressive symptoms, b = -.61 (SE = .28), p = .03; proactive aggression, b = -.17 (SE = .05), p = .0006; and sleep problems, b = -.15 (SE = .06), p = .01. Specifically, higher COVID-19 impact was associated with more depressive symptoms among youth with low, p = .0004, and average, p = .0005, but not high self-enhancing humor, p = .46. COVID-19 impact was also associated with more proactive aggression among youth with low, p < .0001, and average, p = .001, but not high self-enhancing humor, p = .56. Figure 2 A illustrates the magnitude of the association between COVID-19 impact and proactive aggression at varying levels of self-enhancing humor. Finally, higher COVID-19 impact was associated with more sleep problems among youth with low, p = .0008, and average, p = .008, but not high self-enhancing humor, p = .83. Self-enhancing humor did not moderate the association between COVID-19 impact and anxiety, p = .29.
Figure 2.
Estimated effects of COVID-19 impact on proactive aggression by (A) self-enhancing humor and (B) cognitive reappraisal.
Cognitive reappraisal
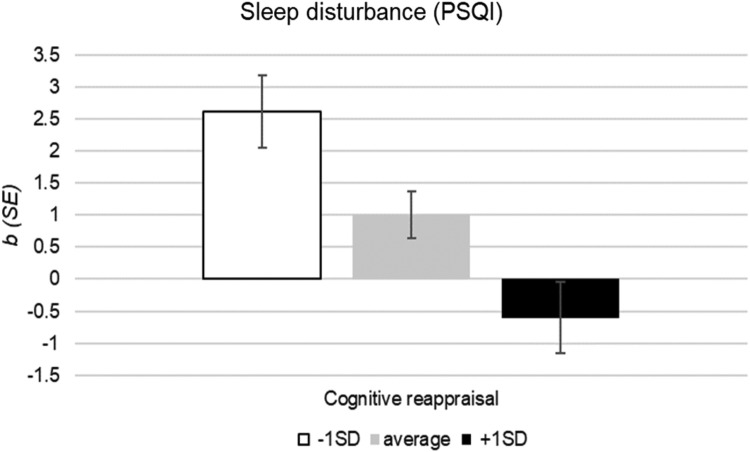
Cognitive reappraisal moderated the association between COVID-19 impact and depressive symptoms, b = -4.57 (SE = 1.70), p = .009; anxiety, b = -4.83 (SE = 1.73), p = .007; proactive aggression, b = -1.19 (SE = .32), p = .0003; and sleep disturbances, b = −1.38 (SE = .35), p = .0002. Specifically, higher COVID-19 impact was associated with more depressive symptoms for adolescents with low, p < .0001, and average, p = .0006, but not high cognitive reappraisal, p = .71. Furthermore, COVID-19 impact was associated with more anxiety for adolescents with low, p = .0001, and average, p = .003, but not high cognitive reappraisal, p = .99. Moreover, COVID-19 impact was associated with more proactive aggression for adolescents with low, p < .0001, and average, p = .006, but not high cognitive reappraisal, p = .35. Figure 2B illustrates the magnitude of the association between COVID-19 impact and proactive aggression at varying levels of cognitive reappraisal. Finally, COVID-19 impact was associated with more sleep problems for adolescents with low, p < .0001, and average, p = .008, but not high cognitive reappraisal, p = .28. Figure 3 illustrates the magnitude of the association between COVID-19 impact and sleep problems at varying levels of cognitive reappraisal.
Figure 3.
Estimated effects of COVID-19 impact on sleep by cognitive reappraisal.
Optimism, purpose in life, and social support
Optimism, purpose in life, and giving social support did not moderate the association between COVID-19 impact and any outcomes, p ≥ .12. There was a nonsignificant trend suggesting that receiving social support moderated the association between COVID-19 impact and depressive symptoms, p = .06, such that greater COVID-19 impact was associated with more depressive symptoms among adolescents reporting receiving low social support, p = .007, but not adolescents reporting average or high social support, p ≥ .13. Receiving social support did not moderate the association between COVID-19 impact and anxiety, proactive aggression, or sleep disturbances, p ≥ .11.
Discussion
For these youth oversampled for ELA, the association between COVID-19 impact and psychiatric symptoms, particularly proactive aggression and sleep disturbances, varied by humor and cognitive reappraisal. Specifically, we observed that greater COVID-19 impact was associated with more psychiatric symptoms among youth with lower cognitive reappraisal and less use of adaptive humor. Cognitive reappraisal and humor are both modifiable skills and may be protective against psychiatric symptoms during prolonged stressors such as a global pandemic. Greater attention to their utility for prevention and intervention is needed.
The association between COVID-19 impact and psychiatric symptoms was reliably stronger among adolescents low in either self-enhancing or affiliative humor. These two forms of humor may promote resilience through different pathways: self-enhancing humor through positive affect and affiliative humor through social engagement. Humor can be increased through targeted interventions, resulting in more positive emotions and less perceived stress [30,31]. This may occur in part because self-enhancing humor involves strategies that make light of daily experiences, which may be an important source of positive affect. Deficits in positive affective systems are prospective risk factors for and a hallmark of depression [32], as well as an increasingly important target of transdiagnostic interventions [33]. By contrast, affiliative humor involves using humor to bring people together. This may be particularly valuable during adolescence given the increased sensitivity of adolescents to peer influence and social rejection. Thus, interventions targeting self-enhancing and affiliative humor in vulnerable adolescent populations may promote resilience by providing skills that help to maintain social relationships and enhance the positive affective benefits that accompany them.
COVID-19 impact was also associated with more psychiatric symptoms among adolescents lower in cognitive reappraisal skills. It is well-established that cognitive reappraisal is protective in the development of both internalizing and externalizing psychopathology [34]. Cognitive reappraisal is a primary target of cognitive behavioral and emotion regulation therapies, in part because it promotes daily experiences of positive affect [35], and is effective in modulating fear and anxiety [36]. The ability to engage in cognitive reappraisal emerges in adolescence [37], and therefore, may be particularly malleable at this time. Training adolescents to implement this skill effectively may have the potential to confer lifelong protection from the mental health sequelae of severe and prolonged stressors such as the global COVID-19 pandemic.
These findings should be considered in the context of their limitations. While this vulnerable sample of youth was recruited before the COVID-19 pandemic, all measures in the present study were cross-sectional, and no causal inferences can be inferred. It is likely that while the impact of COVID-19 may lead to psychopathology, pre-existing psychopathology may also lead to more COVID-19 concerns. Experimental studies, including interventions, that modify cognitive reappraisal and humor can inform whether the association between pandemic impact and psychiatric symptoms are indeed bi-directional, which would ultimately inform decisions about intervention targeting and dissemination particularly for the most vulnerable adolescents. Our focus in this study was on modifiable psychosocial resources with previous evidence of a protective role in the aftermath of stressful experiences. The battery of assessments was not exhaustive, and exploration of other resources that could be leveraged for vulnerable youth is needed; for example, several coping strategies have been identified as protective among Chinese adolescents during COVID-19 [38,39]. Furthermore, this study included adolescent self-report of recent concerns about COVID-19 as part of the impact this pandemic has had on their lives. These concerns are nonpathological but may reflect a pre-existing vulnerability to negative affect, which is a risk factor for and shares variance with psychopathology. Studies engaging parent or third-party report of COVID-19 impact on the adolescent may be informative in this regard. Furthermore, the present data were collected from 88 adolescents from 70 families. Attention to the shared and unique experience of the pandemic within and across families is needed. Finally, our outcome measure of sleep disturbance showed low internal reliability in this sample, as it has in other adolescent samples. Thus, replication of these findings with a sleep measure developed specifically for adolescents is warranted.
While the focus of the present study was the COVID-19 pandemic, these findings may generalize to other prolonged stressors. Stress and psychopathology are intricately linked, and stress may increase vulnerability to psychopathology through multiple plausible pathways. The present analyses were tested using cross-sectional data in a prospective sample of adolescents at risk for psychopathology by virtue of their 2- to 5-fold greater ELA relative to the general population. Indeed, youth with pre-existing psychopathology or a history of ELA may be among the most vulnerable to the long-term consequences of the pandemic [40] and other prolonged stressors. Given the ubiquity of stressful life events at both the individual and community levels across the lifespan, investments in strategies that mitigate the long-term mental health consequences of stressors may ease growing mental health disparities. Doing so among the most vulnerable adolescents is especially imperative because disruptions to their social, emotional, and academic development have great potential to lead to lasting disparities.
Acknowledgments
The present study was conducted with the support of the National Institute of Mental Health (K08MH112773), the Brain and Behavior Research Foundation (27013), and the National Center for Advancing Translational Sciences (UL1 TR001414).
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
References
- 1.Araújo LA de, Veloso C.F., Souza M. de C. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. J Pediatr (Rio) 2021;97:369–377. doi: 10.1016/j.jped.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schippers M.C. For the greater good? The Devastating Ripple effects of the Covid-19 Crisis. Front Psychol. 2020;11:577740. doi: 10.3389/fpsyg.2020.577740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Imran N., Aamer I., Sharif M.I. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pak J Med Sci. 2020;36:1106–1116. doi: 10.12669/pjms.36.5.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orben A., Tomova L., Blakemore S.-J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc Health. 2020;4:634–640. doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallagher M.W., Long L.J., Phillips C.A. Hope, optimism, self-efficacy, and posttraumatic stress disorder: A meta-analytic review of the protective effects of positive expectancies. J Clin Psychol. 2020;76:329–355. doi: 10.1002/jclp.22882. [DOI] [PubMed] [Google Scholar]
- 6.Feder A., Ahmad S., Lee E.J. Coping and PTSD symptoms in Pakistani earthquake survivors: Purpose in life, religious coping and social support. J Affect Disord. 2013;147:156–163. doi: 10.1016/j.jad.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 7.Schaefer S.M., Morozink Boylan J., van Reekum C.M. Purpose in life predicts better emotional recovery from negative stimuli. PLoS One. 2013;8:e80329. doi: 10.1371/journal.pone.0080329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flouri E., Mavroveli S. Adverse life events and emotional and behavioural problems in adolescence: The role of coping and emotion regulation. Stress Health J Int Soc Investig Stress. 2013;29:360–368. doi: 10.1002/smi.2478. [DOI] [PubMed] [Google Scholar]
- 9.Troy A.S., Wilhelm F.H., Shallcross A.J. Seeing the silver lining: Cognitive reappraisal ability moderates the relationship between stress and depressive symptoms. Emot Wash DC. 2010;10:783–795. doi: 10.1037/a0020262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzpatrick K.M. How positive is their future? Assessing the role of optimism and social support in Understanding mental health Symptomatology among Homeless adults. Stress Health J Int Soc Investig Stress. 2017;33:92–101. doi: 10.1002/smi.2676. [DOI] [PubMed] [Google Scholar]
- 11.Nichter B., Haller M., Norman S. Risk and protective factors associated with comorbid PTSD and depression in U.S. military veterans: Results from the National Health and Resilience in Veterans Study. J Psychiatr Res. 2020;121:56–61. doi: 10.1016/j.jpsychires.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Fritz H.L., Russek L.N., Dillon M.M. Humor Use moderates the relation of stressful life events with psychological distress. Pers Soc Psychol Bull. 2017;43:845–859. doi: 10.1177/0146167217699583. [DOI] [PubMed] [Google Scholar]
- 13.Killgore W.D.S., Taylor E.C., Cloonan S.A. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291:113216. doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu C., Xu Y., Xu S. Cognitive reappraisal and the association between perceived stress and anxiety symptoms in COVID-19 Isolated people. Front Psychiatry. 2020;11:858. doi: 10.3389/fpsyt.2020.00858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hawke L.D., Barbic S.P., Voineskos A. Impacts of COVID-19 on youth mental health, substance Use, and well-being: A rapid survey of clinical and community samples: Répercussions de la COVID-19 sur la santé mentale, l’utilisation de substances et le bien-être des adolescents : Un sondage rapide d’échantillons cliniques et communautaires. Can J Psychiatry Rev Can Psychiatr. 2020;65:701–709. doi: 10.1177/0706743720940562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou S.-J., Zhang L.-G., Wang L.-L. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roubinov D., Bush N.R., Boyce W.T. How a pandemic could advance the Science of early adversity. JAMA Pediatr. 2020;174:1131–1132. doi: 10.1001/jamapediatrics.2020.2354. [DOI] [PubMed] [Google Scholar]
- 18.Doom J., Seok D., Narayan A., Fox K. Adverse and Benevolent childhood experiences Predict mental health during the COVID-19 pandemic. Advers Resil Sci. 2020 doi: 10.1007/s42844-021-00038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo J., Fu M., Liu D. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110:104667. doi: 10.1016/j.chiabu.2020.104667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thakur N., Hessler D., Koita K. Pediatrics adverse childhood experiences and related life events screener (PEARLS) and health in a safety-net practice. Child Abuse Negl. 2020;108:104685. doi: 10.1016/j.chiabu.2020.104685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koita K., Long D., Hessler D. Development and implementation of a pediatric adverse childhood experiences (ACEs) and other determinants of health questionnaire in the pediatric medical home: A pilot study. PLOS ONE. 2018;13:e0208088. doi: 10.1371/journal.pone.0208088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NIH; 2020. COVID-19 adolescent symptom and psychological experience questionnaire (CASPE)https://www.nlm.nih.gov/dr2/CASPE_AdolSelfReport_Qualtrics.pdf Available at: [Google Scholar]
- 23.Kuhlman K.R., Chiang J.J., Bower J.E. Persistent low positive affect and sleep disturbance across adolescence moderate link between stress and depressive symptoms in early adulthood. J Abnorm Child Psychol. 2020;48:109. doi: 10.1007/s10802-019-00581-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gross J.J., John O.P. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 25.Martin R.A., Puhlik-Doris P., Larsen G. Individual differences in uses of humor and their relation to psychological well-being: Development of the Humor Styles Questionnaire. J Res Personal. 2003;37:48–75. [Google Scholar]
- 26.Scheier M.F., Carver C.S., Bridges M.W. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the life Orientation test. J Pers Soc Psychol. 1994;67:1063. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 27.Scheier M.F., Wrosch C., Baum A. The life engagement test: Assessing purpose in life. J Behav Med. 2006;29:291. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 28.Shakespeare-Finch J., Obst P.L. The development of the 2-way social support scale: A measure of giving and receiving emotional and instrumental support. J Pers Assess. 2011;93:483–490. doi: 10.1080/00223891.2011.594124. [DOI] [PubMed] [Google Scholar]
- 29.Hayes A.F. Guilford Press; New York, NY: 2013. Introduction to Mediation, moderation, and conditional process analysis: A regression-Based Approach. [Google Scholar]
- 30.Sánchez J.C., Echeverri L.F., Londoño M.J. Effects of a humor Therapy Program on stress levels in pediatric Inpatients. Hosp Pediatr. 2017;7:46–53. doi: 10.1542/hpeds.2016-0128. [DOI] [PubMed] [Google Scholar]
- 31.Tagalidou N., Loderer V., Distlberger E. Feasibility of a humor Training to promote humor and Decrease stress in a Subclinical sample: A single-Arm pilot study. Front Psychol. 2018;9 doi: 10.3389/fpsyg.2018.00577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rawal A., Collishaw S., Thapar A. “The risks of playing it safe”: A prospective longitudinal study of response to reward in the adolescent offspring of depressed parents. Psychol Med. 2013;43:27–38. doi: 10.1017/S0033291712001158. [DOI] [PubMed] [Google Scholar]
- 33.Craske M.G., Meuret A.E., Ritz T. Positive affect treatment for depression and anxiety: A randomized clinical trial for a core feature of anhedonia. J Consult Clin Psychol. 2019;87:457–471. doi: 10.1037/ccp0000396. [DOI] [PubMed] [Google Scholar]
- 34.Compas B.E., Jaser S.S., Bettis A.H. Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychol Bull. 2017;143:939–991. doi: 10.1037/bul0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brockman R., Ciarrochi J., Parker P. Emotion regulation strategies in daily life: Mindfulness, cognitive reappraisal and emotion suppression. Cogn Behav Ther. 2017;46:91–113. doi: 10.1080/16506073.2016.1218926. [DOI] [PubMed] [Google Scholar]
- 36.Theurel A., Gentaz E. The regulation of emotions in adolescents: Age differences and emotion-specific patterns. PLoS One. 2018;13:e0195501. doi: 10.1371/journal.pone.0195501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silvers J.A., McRae K., Gabrieli J.D.E. Age-related differences in emotional reactivity, regulation, and rejection sensitivity in adolescence. Emot Wash DC. 2012;12:1235–1247. doi: 10.1037/a0028297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duan L., Shao X., Wang Y. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang C., Ye M., Fu Y. The psychological impact of the COVID-19 pandemic on Teenagers in China. J Adolesc Health. 2020;67:747–755. doi: 10.1016/j.jadohealth.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Novins D.K., Althoff R.R., Billingsley M.K. JAACAP’s role in Advancing the Science of pediatric mental health and promoting the care of youth and families during the COVID-19 pandemic. J Am Acad Child Adolesc Psychiatry. 2020;59:686–688. doi: 10.1016/j.jaac.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]