Abstract
The coronavirus disease 2019 (COVID-19) pandemic has stretched our healthcare system to the brink, highlighting the importance of efficient resource utilization without compromising healthcare provider safety. While advanced imaging is a great resource for diagnostic purposes, the risk of contamination and infection transmission is high and requires extensive logistical planning for intrahospital patient transport, healthcare provider safety, and post-imaging decontamination. This dilemma has necessitated the transition to more bedside imaging. More so than ever, during the current pandemic, the clinical utility and importance of point-of-care ultrasound (POCUS) cannot be overstressed. It allows for safe and efficient beside procedural guidance and provides front line providers with valuable diagnostic information that can be acted upon in real-time for immediate clinical decision-making. The authors have been routinely using POCUS for the management of COVID-19 patients both in the emergency department and in intensive care units turned into “COVID-units.” In this article, we review the nuances of using POCUS in a pandemic situation and maximizing diagnostic output from this bedside technology. Additionally, we review various methods and diagnostic uses of POCUS which can replace conventional imaging and bridge current literature and common clinical practices in critically ill patients. We discuss practical guidance and pertinent review of the literature for the most relevant procedural and diagnostic guidance of respiratory illness, hemodynamic decompensation, renal failure, and gastrointestinal disorders experienced by many patients admitted to COVID-units.
Keywords: COVID-19, SARS-CoV-2, Point-of-care ultrasound, COVID-intensive care units, COVID-unit, Critical care, Decontamination, Pandemic, Imaging in COVID-19, Point-of-care ultrasound in a pandemic
Core Tip: In the current coronavirus disease 2019 (COVID-19) pandemic, advanced imaging is a great resource for diagnostic purposes but the risk of contamination and intra-hospital infection transmission is high and requires extensive logistical planning for intrahospital patient transport, healthcare provider safety, and post-imaging decontamination. Point-of-care ultrasonography is a reliable and resourceful tool for bedside diagnosis and clinical assessment. We discuss practical guidance and pertinent review of the literature for the most relevant procedural and diagnostic guidance of respiratory illness, hemodynamic decompensation, renal failure, and gastrointestinal disorders experienced by many patients admitted to COVID-units.
INTRODUCTION
The novel coronavirus disease of 2019 (COVID-19) has led to over two million deaths till date. Given 4.6 per 100000 patients with COVID-19 pneumonia require hospitalization, and 9%-11% of these requiring intensive care units (ICU) care, diagnostic imaging will likely be necessary during their hospitalization. Some conventional imaging modalities, such as computed tomography (CT), carry high sensitivity and specificity for diagnoses. However, there are logistical concerns associated with isolation, intra-hospital transport, time and person-power expenditure, as well as risk for healthcare exposures. They also require a labor-intensive decontamination process of the imaging location and the intra-hospital pathway. This has caused most institutions to shift toward reliance on point-of-care imaging. The American College of Radiology and Radiological Society of North America have established guidelines for preparedness and decontamination of imaging equipment for special pathogen units such as COVID-units[1]. The challenge of using imaging equipment lies in protecting caregivers and preventing disease transmission. Additionally, it requires maneuvering a portable X-ray machine in and out of isolation rooms (“hot zones”), double-bagging of X-ray detectors with impermeable plastic sheets, and often multiple caregivers protected by personal protective equipment (PPE). The process of efficient and safe decontamination can be time-consuming and requires an investment of substantial resources and regular training of technicians.
Instead, point-of-care ultrasound (POCUS) can replace X-rays and CTs in many situations and thus mitigate logistical problems associated with large equipment for radiography. Numerous studies have reported the accuracy and non-inferiority of POCUS compared to conventional imaging for clinical diagnosis and decision-making[2]. Moreover, POCUS has become a standard part of the critical care medicine training curriculum and is recommended by several international society guidelines for the care of critically ill patients[3-8]. Its use has also been highlighted in epidemics, specifically the Ebola epidemic, where it proved as a useful clinical tool in patient care[9].
The goal of this article is to provide readers with an understanding of how to best use POCUS for acutely ill patients during the time of a pandemic, where resources are stretched thin and routine imaging studies such as X-rays and CT scans occur with diminished frequency due to logistical constraints. Using real-time ultrasound images from our COVID-19 patients, we want to highlight those POCUS techniques that can rapidly replace conventional imaging modalities during this COVID pandemic, offer instruction on performance, and provide an evidence-based anchor via reference literature.
General considerations with POCUS in COVID-units
A few general considerations with POCUS in COVID-units.
Dedicated ultrasound and location: In COVID-units hosting multiple patients, it is essential to have an ultrasound machine dedicated strictly to that unit. The machine should be stored at a specified location for easy retrieval during emergent use[10].
Bundling of ultrasound examinations with patient care: Given the logistics of donning and doffing PPE and ultrasound machine decontamination, along with risks to healthcare workers, ultrasound examinations should be bundled with other patient care-related activities when possible.
Ultrasound machine and probe decontamination: Although easier to clean compared to large X-ray machines, ultrasound machines used on COVID-19 patients still need to be thoroughly disinfected according to institutional protocols. Thoroughly wipe down with a probe-friendly Environmental Protection Agency-approved disinfectant wipe for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the transducer probes, screen, keypad, wires, and plug before bringing it outside the patient’s room, to prevent contamination of “warm” and “cold zones”[11]. We advocate for cleaning the machine before leaving the patient’s room, and once again immediately outside the patient room thereafter, as argued by other authors[12]. Despite cohorting of COVID-19 patients, disinfecting ultrasound machines in between patient care is paramount to protect healthcare workers from potential occupational exposure. An ultrasound probe cover should be used for sterile procedures to prevent nosocomial infection to the patients and also maintain a barrier for the machine from bodily fluids[13]. Consider individual ultrasound gel packets to prevent cross-contamination as well as ultrasound machine covers for more easily wipeable decontamination surface[14].
Ultraportable ultrasound devices: Handheld pocket ultrasounds are commonly being used in emergency departments, and ICUs and can be ideal for pandemic situations. Regular probe covers can be used for a handheld device with the decontamination process similar to that used for cart-based machines after use.
Training: Care must be taken to ensure that providers using POCUS are sufficiently trained, credentialed as relevant, and that appropriate supervision is provided institutionally. This becomes relevant, particularly where providers are being repurposed for clinical duties outside their prior scope of practice. Simulation-based training in using and decontaminating ultrasound devices can help providers to become accustomed to institutional procedures and protocols[15].
Saving images and documentation: It is important to save images obtained on POCUS to the patient charts using picture archiving and communication system or digital imaging and communications in medicine for review and interpretation by other care providers and consultants on the team[11]. A brief procedure note can be documented in the patient chart highlighting the findings on the POCUS examination along with pictures of highlighted findings if possible. Saving images and documenting reports are important, as they provide accessible records and allows for comparison through serial imaging. In order to minimize contact time and exposure risk, it is imperative to focus only on the acquisition of quality images while in the patient’s room with the ability to interpret outside the room subsequently.
Overview of diagnostic utility of POCUS
POCUS has been increasingly utilized for both, procedural guidance and bedside diagnosis of a multitude of conditions. Table 1 lists many of these applications, which are summarized below.
Table 1.
Various applications of point-of-care ultrasound in a coronavirus disease 2019-units
|
Point of care ultrasound in COVID-units
| |
| Procedural guidance | Endotracheal intubation |
| Peripheral intravenous access | |
| Central venous access | |
| Gastric tube placement | |
| Thoracentesis | |
| Paracentesis | |
| Lumbar puncture | |
| Airways and lung | Pleural effusions |
| Patchy B-lines and rugged pleural surface | |
| Consolidations | |
| Atelectasis | |
| Pneumothorax | |
| Shock physiology | Fluid responsiveness |
| Stroke volume assessment | |
| Pericardial effusion | |
| Right ventricular function | |
| Tricuspid annular planar systolic excursion | |
| Shunt physiology with agitated saline | |
| Deep vein thrombosis | |
| Abdomen and hepatobiliary | Ascites |
| Small bowel obstruction | |
| Acute cholecystitis | |
| Acute cholangitis | |
| Pancreatic evaluation | |
| Aortic evaluation | |
| Genitourinary | Acute kidney injury |
| Hydronephrosis | |
| Renal stones | |
| Renal vascular resistive indices for volume overload | |
| Neurovascular | Optic nerve sheath diameter |
COVID-19: Coronavirus disease 2019.
Procedural guidance
POCUS has been found to improve first attempt success in many procedures needed in a COVID-unit.
Endotracheal intubation
One of the most common reasons for admission to a COVID-unit is acute hypoxemic respiratory failure requiring invasive mechanical ventilation. During the COVID-19 outbreak, many hospitals have protocols for direct invasive mechanical ventilation, opting against non-invasive positive pressure ventilation to reduce the risk of aerosolized exposure[16,17]. A chest radiograph (CXR) to confirm the correct placement of the endotracheal tube (ETT) is often performed after intubation. Instead, ultrasonography can be used to confirm successful ETT placement. The advantages of POCUS are its easy availability, high specificity, speed of detection, safety (without radiation exposure), and ease of repeat imaging. A high-frequency linear probe is used to ultrasound the neck during or after the endotracheal intubation. With the probe placed in a transverse position at the base of the neck, the trachea appears as a round hypoechoic structure in the center of the neck with a reverberation artifact and hypoechoic shadow. If the probe is moved slightly to the left of the trachea, the esophagus appears as a thick-walled collapsed structure with the hypoechoic center just posterior to the trachea. As the ETT passes through the trachea, one can visualize fluttering in the trachea as immediate confirmation of endotracheal intubation. This is known as the “Snowstorm sign”[18]. On successful endotracheal intubation, the widening of the vocal cord with a hyperechoic circular tube in the trachea with an acoustic shadow beneath it is seen. This is known as a “Bullet Sign”[18] (Figure 1). In the event of esophageal intubation, the tube will be visualized in the esophagus and gives the impression of a second trachea. This is known as the “double-track sign”[19]. The accuracy of linear-probe ultrasound for successful intubation is 98%[20]. Once the successful endotracheal intubation is performed, mainstem bronchus intubation can be ruled out by performing a lung ultrasound using a linear high-frequency probe with a sensitivity of 98.7% and specificity of 97.1%[21]. In tracheal intubations, bilateral lung sliding should be visualized on POCUS. In the case of right mainstem bronchus intubation, the left contralateral lung exam will not demonstrate lung sliding due to absent lung ventilation. Cardiac pulsations, visualized on the pleural surface (lung pulse) can help differentiate main stem intubation from a pneumothorax[22] (Video 1). Once identified, the ETT can be retracted by a few centimeters during simultaneous ultrasound visualization of left lung to assess for lung sliding, which confirms correct placement of ETT.
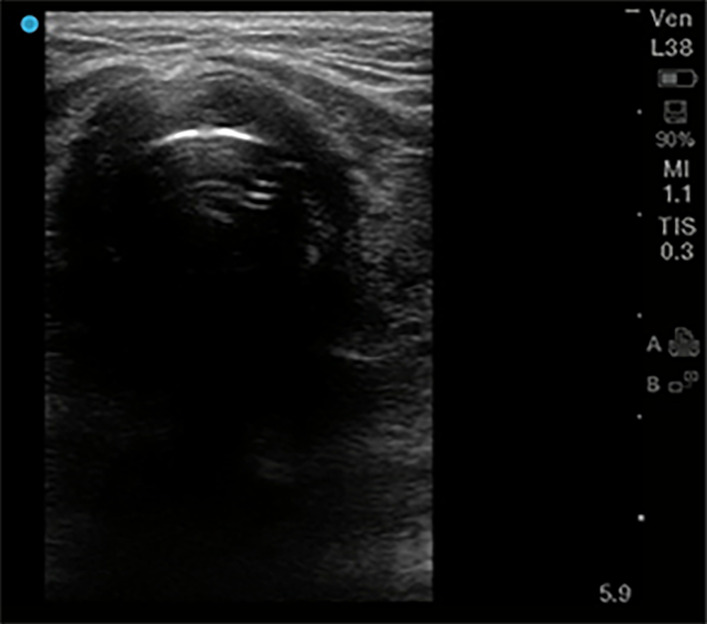
Figure 1.
Endotracheal intubation. High frequency 5-10 MHz linear probe with probe marker facing toward patients’ right side, placed at base of neck midline just superior to suprasternal notch. “Bullet sign” of proper endotracheal intubation seen here, with hyperechoic air-mucosal interface and posterior shadowing.
Peripheral venous access
A high-frequency linear probe can be used to place peripheral venous access swiftly if superficial veins are not identified on a physical exam. Ideally, a superficial vein that is 3 mm to 10 mm beneath the skin is visualized in transverse and longitudinal axis with an ultrasound. This allows the provider to gauge the path of the vein and decide the length of the intravenous catheter to use. A color Doppler can be utilized to differentiate an artery from a vein when in doubt. The success rate of ultrasound-guided peripheral venous access is 81% compared to 70% in the control group with palpation/visualization approach. It also reduces the number of attempts and time to achieve a venous access[23,24].
Arterial access
Arterial access is often required in patients requiring vasopressor therapy and invasive mechanical ventilation for close hemodynamic monitoring and frequent arterial blood gases. The radial artery is the most common site utilized for arterial line placement. Using POCUS, first-pass success can be improved by up to 71%[25]. Since the vessel and the catheter tip can be directly visualized in real-time during the procedure, the chances of complications are lower compared to palpation method[26]. POCUS also offers superiority in deeper located arteries decreasing serious complications and improving the first-pass success.
Central venous access and confirmation
There are several advantages of having central venous access in patients admitted to a COVID-ICU. It reduces the number of venous punctures for frequent blood draws, allows for hemodynamic monitoring, and consistent access for sedation and vasoactive medications. Standard of care is for central venous line (CVL) placement to be performed under direct ultrasonographic visualization as its use reduces complications and improves first-pass success when conducted by trained personnel[27]. Real-time POCUS can be utilized to visualize and capture the image of the guide-wire in the intended central vessel during the procedure. Once the CVL is placed, an agitated saline bolus can identify correct placement by finding immediate microbubbles in the right atrium on the subcostal cardiac view (also known as rapid atrial swirl sign) (Video 2)[28]. The same probe can be utilized post-procedure to ensure lung sliding and rule out procedure-related pneumothorax. A prospective study identified correct CVL placement using POCUS with a sensitivity of 86.8% and a specificity of 100%[29]. They found that the median time to POCUS completion for confirmation of line placement was 16 min compared to 32 min for a CXR[29]. This time difference is further accentuated in COVID-units, given the intricate process of PPE and decontamination needs with X-ray machines.
Gastric tube placement
Patients admitted to COVID-units are often intubated for mechanical ventilation and require nutrition via an enteral feeding tube. Gastric tube placement is generally a safe procedure, but in rare instances, complications such as bronchial placement, pneumothorax, pneumonia, tracheal or esophageal injury can occur[30]. Typically, a CXR is required for confirmation of the tube placement in the stomach. However, in COVID-units, this can be time- and resource-consuming. Instead, a POCUS can be used to identify the correct placement of a gastric tube with a 91%-98% sensitivity and 67%-100% specificity using a two-point approach[31,32]. Using a micro-convex (2-4 Hz) probe or a small footprint high-frequency linear probe (5-10 MHz), the trachea and esophagus are visualized in the suprasternal notch. A gastric tube appears as a hyperechoic circular structure within the esophagus, posterior to the trachea with an acoustic shadow below it. Once confirmed, using a low-frequency probe (2-5 MHz the curvilinear probe or 1-5 MHz phased array probe) in the epigastric region angling towards the left subcostal region, the gastric tube can be identified as a hyperechoic line within the stomach (Figure 2). It is important to note that in an air-filled stomach, visualization of the gastric tube may be difficult. Attaching the tube to suction before performing the POCUS examination can increase the diagnostic yield.
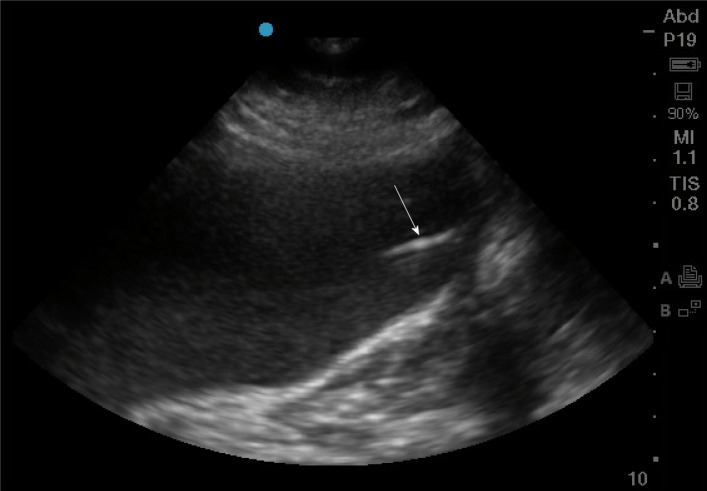
Figure 2.
Gastric enteral tube placement. Phased array probe (1-5 MHz) in “Abdominal” preset with probe marker facing cephalad placed in left mid-clavicular subcostal location. The stomach here is distended with hypoechoic fluid, and inside it can be seen a linear hyperechoic density representing the gastric enteral tube (arrow).
DIAGNOSTIC POCUS
Lungs
Studies have demonstrated that a CT scan of the chest is 86% sensitive in making a clinical diagnosis of COVID-19[33]. Typical findings include peripheral based patchy ground-glass opacities with increasing lung involvement with the severity of illness[34]. Pleural effusions, cavitary lesions, nodules, and mediastinal lymphadenopathy are uncommon in COVID-19[34,35]. POCUS can better characterize COVID-19 Lung disease, and lung ultrasound patterns have been described[36]. A multiple-point lung examination with ultrasound can be a quick and efficient way to demonstrate patchy B-lines with interspersed normal lung parenchyma in early disease (Figure 3). Subsequently, subpleural consolidation with bronchograms can also be appreciated. Lung ultrasonography can also help in identifying early disease even before symptom onset[35] (Video 3).
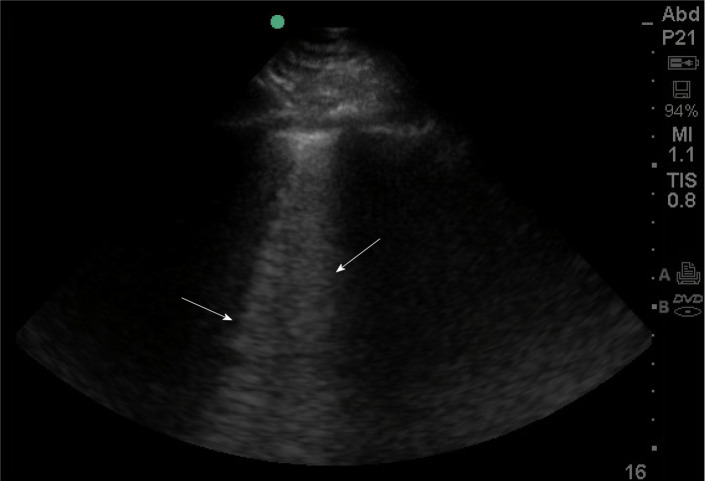
Figure 3.
B-lines on lung ultrasound. Phased array probe (1-5 MHz) with probe marker facing cephalad placed in an intercostal space. B lines (denoted by arrows), are well-defined comet-tail, vertical hyperechoic artifacts arising from the pleural line that obliterate normal A-lines, and descend to the bottom of the screen. Multiple B-lines in an interspace indicates an interstitial syndrome, where there are increased air-fluid interfaces creating this artifact.
Ultrasound is superior to CXR in assessing for pleural effusions[37]. Development of secondary bacterial pneumonia and parapneumonic loculated effusions can be seen on POCUS and can guide if draining is required (Video 4). Early literature from China suggests an incidence of pneumothorax in SARS-CoV-2 to be 2% compared to 25% in SARS-CoV-1[38,39]. However, the incidence may be much higher based on our experience and multiple reported cases in the literature[40,41]. A sudden hemodynamic decompensation with acute hypoxemia in an otherwise stable intubated patient should raise suspicion for a pneumothorax that may need prompt identification and intervention. Identifying a lung point in the absence of B-lines and lung sliding can quickly identify a pneumothorax and help decide on early intervention with chest tube placement and decompression[42] (Video 5). The M-mode can be used to observe lung pulse and “sandy-beach” appearance of healthy lungs to reasonably exclude the possibility of a pneumothorax[42] (Video 6, Figure 4). Since most COVID-19 patients present with severe CXR and require prolonged mechanical ventilation, POCUS can be used to assess diaphragm atrophy and chances of liberation from the ventilator. While several methods of examining the diaphragm exist, the easiest methods include assessing diaphragmatic thickness in anterior subcostal space using curvilinear low-frequency probe and M-mode to assess the amplitude of diaphragmatic excursion and the velocity of the contraction[43]. The normal thickness of the diaphragm is 22-28 mm[44]. The thickness of less than 20 mm may suggest the presence of diaphragmatic atrophy[45].
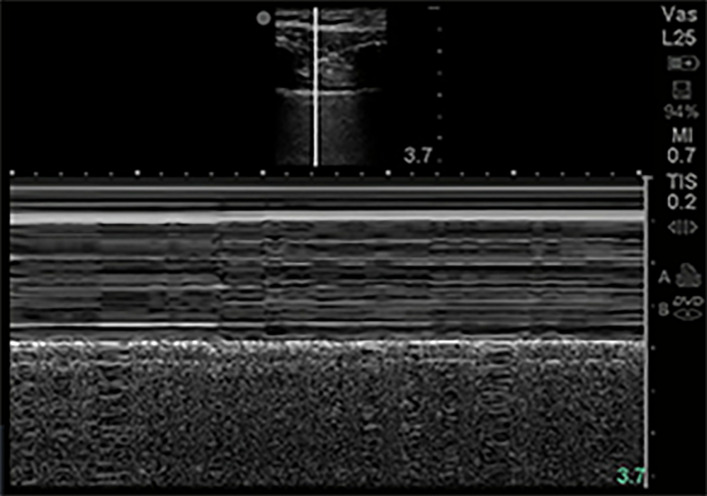
Figure 4.
M-Mode normal lung. M-mode of normal lung demonstrates linear shadows from soft tissue followed by granular deeper shadows commonly described as “Sandy-beach sign”.
Cardiac
Cardiac ultrasound is an excellent tool to assess for global and regional wall motion of the cardiac chambers, pericardial, valvular pathology, right ventricular dysfunction, volume responsiveness, and to differentiate etiologies of shock. American Society of Echocardiography recently published a statement on POCUS use in COVID-19 patients, with a recommended protocol for relevant cardiac views[11].
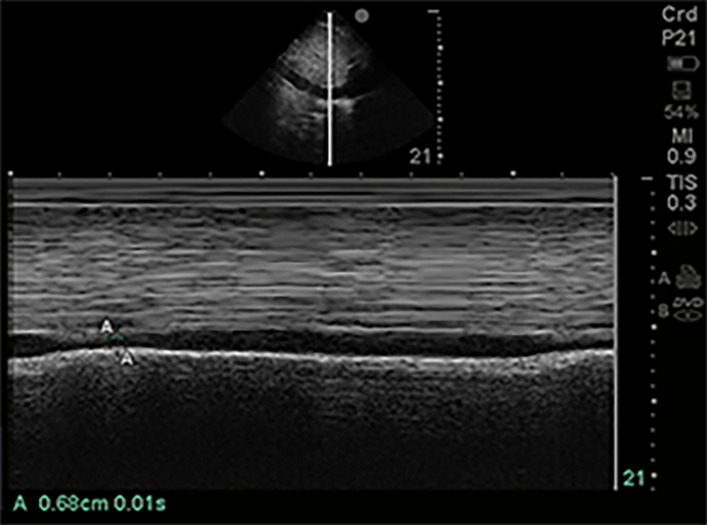
Often assessment of volume status in COVID-19 patients is pertinent but challenging. Several methods have been used for volume status assessment with varying limitations[46]. In mechanically ventilated patients who are not breathing spontaneously, measuring the distensibility of the inferior vena cava (IVC) can help assess volume status (Figure 5). More importantly, the respiratory variation in IVC diameter (known as ΔIVC) can predict fluid responsiveness in mechanically ventilated patients with a sensitivity of 76% and specificity of 86% according to a meta-analysis[47]. Vignon et al[48] assessed various parameters, including variation in superior vena cava (SVC) using transesophageal ultrasonography, variation in IVC, and change in left ventricular outflow tract (LVOT) velocity using pulsed-wave doppler for fluid responsiveness. While SVC variation had the best specificity (84%) in predicting fluid responsiveness, variation in IVC diameter (greater than 8%) had a specificity of 70%. It is imperative to note that patients IVC variability may not be accurate in spontaneously breathing patients experiencing significant dyspnea as it can lead to significant variation in intrathoracic pressures and IVC diameter[49]. Variation in IVC diameter, coupled with lung and cardiac ultrasound exams can be helpful for clinical decision-making about volume status. A hyperdynamic left ventricle (LV) may suggest underfilling and need for intravascular volume resuscitation[50]. For a more accurate assessment, an M-mode can be used in the parasternal short-axis across the LV to assess papillary muscle apposition[50].
Figure 5.
Inferior vena cava size in M-mode. Of 1-5 MHz phased array probe with probe marker facing cephalad, subcostal location, inferior vena cava (IVC) visualized in sagittal plane. M-mode line centered on IVC just inferior to hepatic vein inflow. IVC measured in this M-mode image at 1.70 cm maximally and 0.68 cm minimally.
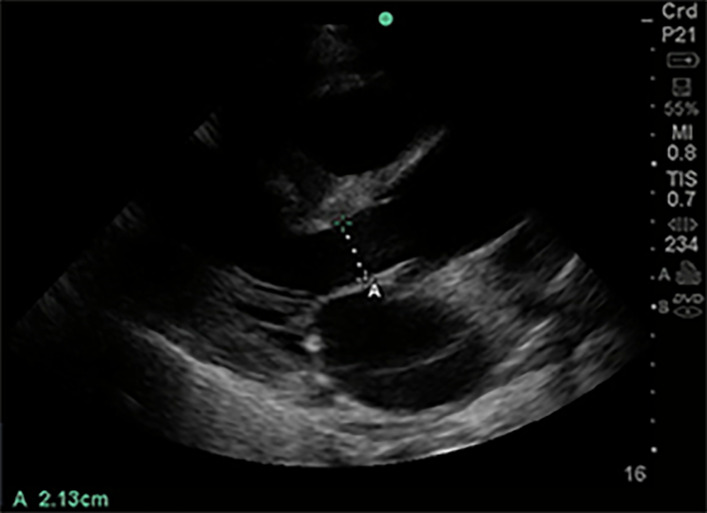
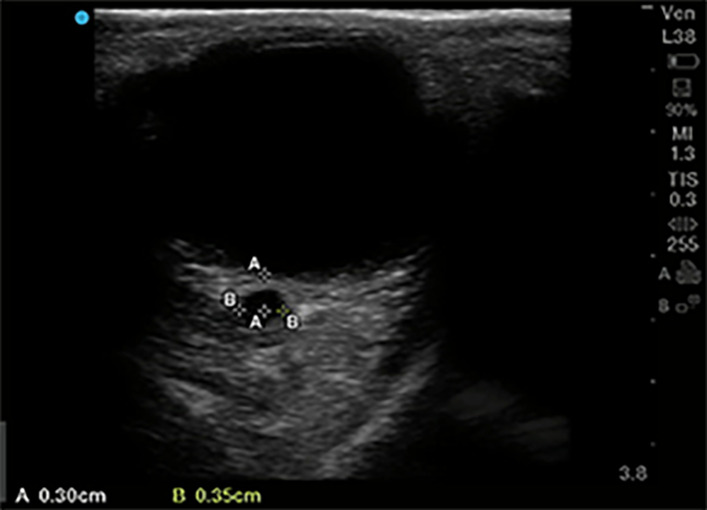
For providers trained in advanced critical care echocardiography, the use of spectral Doppler can help assess stroke volume and cardiac output[51]. In the parasternal long-axis view, the LVOT diameter can be measured to estimate LVOT area[51] (Figure 6). Using a pulsed wave Doppler, the LVOT velocity time integral (VTI) can be calculated in a five-chamber apical cardiac view (Figure 7). This estimates the distance traveled by blood in one heartbeat. Multiplying the LVOT VTI by the LVOT area equals the stroke volume for each cardiac contraction (Figure 8)[51,52]. If the stroke volume or cardiac output is reduced, depending on the clinical picture, it could result in the initiation of inotropy or volume resuscitation. The key is for repeated measurement of stroke volume/cardiac output with any given intervention.
Figure 6.
Left ventricular outflow tract diameter parasternal long axis view. Of 1-5 MHz phased array probe with probe marker facing patient’s right shoulder, parasternal long axis view. Left ventricular outflow tract diameter measured during mid-systole, inner edge to inner edge, from septal endocardium to anterior mitral leaflet, in order to calculate cross-sectional area (πr2).
Figure 7.
Left ventricular outflow tract velocity time integral. Of 1-5 MHz phased array probe, apical 5 chamber view. Pulsed wave doppler selected, with sample volume placed 5 mm proximal to aortic valve in center of the left ventricular outflow tract. Notice narrow signal with rapid upstroke in velocities, with end-systolic click terminating flow signal. In this case traced velocity time integral was 19.9 cm.
Figure 8.
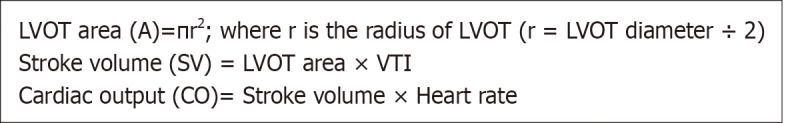
Formula to calculate stroke volume and cardiac output using pulsed wave doppler. LVOT: Left ventricular outflow tract; VTI: Velocity time integral.
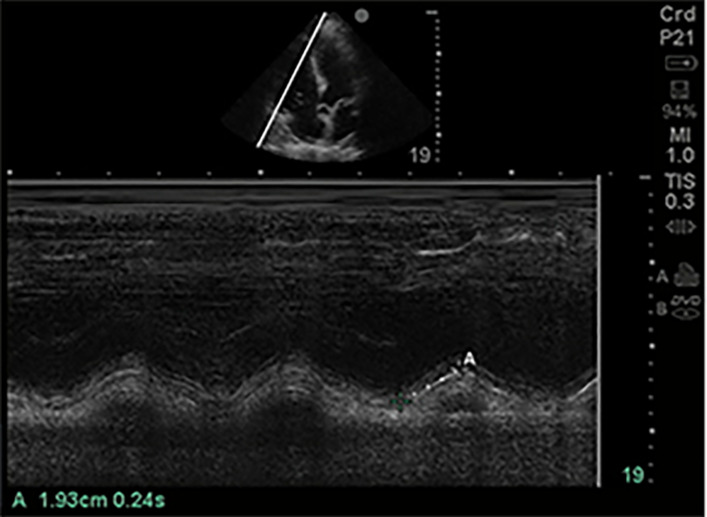
Another utility of cardiac ultrasound is to assess the etiology of the shock state. The presence of a large pericardial effusion with right ventricular and atrial wall collapse may suggest tamponade physiology. A large, dilated right ventricle (RV) with hypokinetic longitudinal walls and hyperkinetic apex may suggest RV outflow obstruction secondary to pulmonary embolism (PE). However, severe hypoxemia with pulmonary vasoconstriction can be seen in COVID-19, and so the presence of a dilated RV may not be specific for a PE and should correlate clinically (Video 7). Using M-mode, tricuspid annular planar systolic excursion can be obtained to estimate RV function in these cases[53] (Figure 9). Although, in cases of negative findings or normal RV function, PE cannot be ruled out as it has a low negative predictive value.
Figure 9.
Tricuspid annular planar systolic excursion (tricuspid annular plane systolic excursion). Phased array probe (1-5 MHz) in “Cardiac” preset, placed in apical 4 chamber view. M-mode line is placed across the lateral tricuspid annulus to assess longitudinal contraction of the right ventricle (RV) free wall, a regional surrogate for RV function. The tricuspid annular planar systolic excursion of this patient was 1.93 cm which is low normal.
POCUS can also be used to investigate the hypoxemia of unclear etiology. A contrast study can be performed at the bedside by injecting agitated sterile saline via a three-way stopcock to look for an intracardiac or intrapulmonary shunt. The appearance of agitated saline bubbles in the LV within three heartbeats suggests an intracardiac shunt, while after five beats may suggest intrapulmonary shunt (late-appearance)[54,55].
Vascular
The risk of venous thromboembolism in COVID-19 has been reported in 25%-31% of COVID-19 patients[56,57] (Video 8). Increasing D-dimer, PT, or aPTT independently predicts the risk of venous thrombus embolism in these patients, thus necessitating assessment for deep vein thrombosis and PE[56-58]. For diagnostic accuracy, a high frequency, the linear probe can be used to assess deep veins of the lower extremities for evidence of thromboembolism[59] (Video 9). Evaluation of two regions (common femoral vein from the bifurcation with the greater saphenous vein to the bifurcation of superficial and deep femoral veins distally, and the popliteal vein) on both legs can be performed rapidly using compression ultrasonography.
Genitourinary
Acute kidney injury (AKI) is a common complication in critically ill patients with COVID-19[60]. Direct viral tropism, cytokine storming, rhabdomyolysis, and acute tubular necrosis (ATN) have been hypothesized as causes of AKI in COVID-19, similar to Ebola or SARS-CoV-1[60-63].
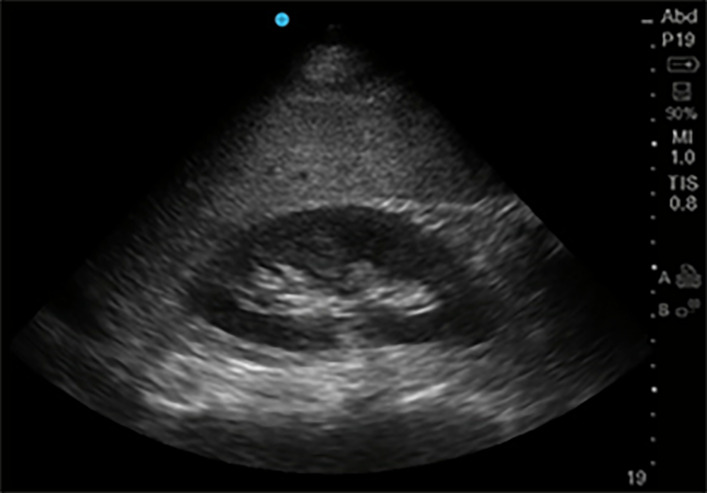
Gray-scale ultrasonography with a low frequency (2-5 MHz) curvilinear probe can be used to assess renal anatomy[64] (Figure 10). In states of hypoperfusion, the kidney appears hypoechoic. In contrast, kidneys appear hyperechoic in ATN secondary to rhabdomyolysis due to myoglobin deposits in the renal tubules[64]. Color Doppler can be utilized to evaluate lobar vessels and can provide information regarding flow states and underlying pathology. The vessels are poorly visible in poor perfusion states and may also indicate poor splanchnic perfusion. In these COVID-19 patients with renal failure, malfunction of a urinary catheter, particularly given duration of the length of indwelling placement, may go unnoticed and misinterpreted as acute kidney injury and anuria. Anechoic bladder volume can be easily seen qualitatively and measured quantitatively on POCUS to help rule out urinary retention and urinary catheter malfunction[65].
Figure 10.
Kidney in its Longitudinal axis. Phased array probe (1-5 MHz) in “Abdominal” preset placed with probe marker facing cephalad in right mid-axillary location. In this normal ultrasound, the liver serves as an acoustic window, under which can be seen the thin hyperechoic kidney capsule, the hypoechoic parenchymal cortex, and the central hyperechoic renal sinus.
Abdominal
Gastrointestinal symptoms in COVID-19 patients are common on presentation as well as complications from hospitalization[66,67]. COVID-19 patients are particularly at risk for bowel hypomotility due to opiates and paralytics[67]. POCUS can be utilized as a diagnostic tool to identify the etiology of the abdominal symptoms in these patients. Using a curvilinear low-frequency probe, paralytic ileus can be identified as both small and large intestinal dilation and bowel wall thickening. A random movement instead of unidirectional flow of spot echogenic material can be seen in fluid-filled bowel, suggesting a downstream bowel obstruction. If the probe is kept still to observe the bowel, one can identify the sedimentation of intestinal content and “pearl-string” like a pattern of gas in the bowel[68]. Distended proximal bowel with collapsed distal bowel can help differentiate mechanical obstruction from paralytic ileus. Studies have demonstrated a sensitivity of 94%-100% and a specificity of 81%-100% for the lung ultrasound in diagnosing small bowel obstruction outperforming plain radiography (sensitivity of 77% and specificity of 50%)[69,70].
Ascites can also be identified easily on POCUS. Assessment of Morrison’s pouch (hepatorenal recess), the splenorenal recess, and the pelvis for fluid collection is a common approach[71] (Video 10). The ideal site for paracentesis can be identified with the largest fluid pocket and least bowel presence. Color Doppler can be used via a linear high-frequency probe to look for abdominal wall vessels to prevent abdominal sheath hematomas and bleeding during paracentesis[71].
Neurologic
Many patients with COVID-19 suffer neurologic complications, and CT imaging of the head can be logistically challenging[72]. Ultrasound has been used as a non-invasive tool to identify elevated intracranial pressures by measuring optic nerve sheath diameter (ONSD)[73]. A high-frequency linear probe can be used to measure the optic nerve sheath diameter at 3 mm beyond the globe, where the contrast is maximum (Figure 11). Since the sensitivity of ONSD greater than 5 mm for intracranial hypertension is 100%, it serves as a useful screening tool for altered mental status in the emergency d and outperforms ophthalmoscopic evidence of papilledema, which can take 12 h to develop[74-76].
Figure 11.
Optic nerve sheath diameter. High frequency 5-10 MHz linear probe in “Ophthalmic” or “Venous” preset with probe gently placed on upper eyelid in horizontal plane. Diameter of optic nerve is measured in transverse dimension, 3 mm posterior to where optic nerve enters the globe. In this patient optic nerve sheath diameter is measured at 3.5 mm.
Limitations
There are several limitations to the use of POCUS in the critical care setting. It requires expertise in general ultrasound knowledge, image acquisition skills, image interpretation skills, and the ability to integrate that information with other data appropriately to make clinical decisions affecting patient care. Certain clinical situations, such as obesity, high PEEP ventilation, bowel gas, and overlying catheters and wires, may interfere with the acquisition of good images. POCUS also requires sufficient experience and confidence to know when imaging is inadequate for interpretation and instead requires a formal sonogram or another imaging modality such as an X-ray or a CT scan.
CONCLUSION
In summary, we noticed a practice gap between literature on critical care ultrasonography and clinical practices commonly employed by many intensivists due to easily available conventional imaging modalities. In the setting of a pandemic, however, conventional imaging modalities become resource limited; therefore, we highlight how POCUS can fill this need in a timely, repetitive and evidence-based manner.
POCUS is an excellent tool for use in COVID-units as it provides essential bedside clinical information reliably and cost-effectively while maintaining patient and provider safety without the need for radiation exposure or arduous decontamination. Its use can improve first-pass success and reduce complications with bedside procedures. Simulation-based training sessions can prepare healthcare providers to utilize this tool efficiently in COVID-units, though obtaining proficiency in some applications requires substantial hands-on experience[77]. Where feasible, handheld POCUS devices can be assigned to each isolation room to prevent the spread of the pathogen and improve patient care. While the use of POCUS in the inpatient setting is continually increasing, provider proficiency and experience must also continuously improve. In a contained situation where limited exposure to healthcare providers is recommended, POCUS can be a useful diagnostic tool and allow for a complete assessment of the patient, as highlighted in this article. Further imaging can be considered if POCUS is unrevealing or non-specific, but it is certain to reduce the requirement of advanced imaging. It is essential to acknowledge the advantages and limitations of POCUS for its appropriate application in COVID-units.
ACKNOWLEDGEMENTS
We would like to express are gratitude to Dr. Henwood PC, Dr. Klopman MA, Dr. Liteplo A and Dr. Kendall JL for critically reviewing the manuscript and suggesting important changes.
Footnotes
Conflict-of-interest statement: All authors have no conflict of interests to declare.
Manuscript source: Unsolicited manuscript
Peer-review started: April 4, 2021
First decision: June 5, 2021
Article in press: July 6, 2021
Specialty type: Critical care medicine
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Inal V, Villalba R S-Editor: Wu YXJ L-Editor: A P-Editor: Wang LYT
Contributor Information
Himanshu Deshwal, Division of Pulmonary, Sleep and Critical Care Medicine, New York University Grossman School of Medicine, New York, NY 10016, United States. himanshu.deshwal@gmail.com.
Deepak Pradhan, Division of Pulmonary, Sleep and Critical Care Medicine, New York University Grossman School of Medicine, New York, NY 10016, United States.
Vikramjit Mukherjee, Division of Pulmonary, Sleep and Critical Care Medicine, New York University Grossman School of Medicine, New York, NY 10016, United States.
References
- 1.Mollura DJ, Palmore TN, Folio LR, Bluemke DA. Radiology preparedness in ebola virus disease: guidelines and challenges for disinfection of medical imaging equipment for the protection of staff and patients. Radiology. 2015;275:538–544. doi: 10.1148/radiol.15142670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lentz B, Fong T, Rhyne R, Risko N. A systematic review of the cost-effectiveness of ultrasound in emergency care settings. Ultrasound J. 2021;13:16. doi: 10.1186/s13089-021-00216-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayo PH, Beaulieu Y, Doelken P, Feller-Kopman D, Harrod C, Kaplan A, Oropello J, Vieillard-Baron A, Axler O, Lichtenstein D, Maury E, Slama M, Vignon P. American College of Chest Physicians/La Société de Réanimation de Langue Française statement on competence in critical care ultrasonography. Chest. 2009;135:1050–1060. doi: 10.1378/chest.08-2305. [DOI] [PubMed] [Google Scholar]
- 4.Guidelines: Emergency, Point-of-Care and Clinical Ultrasound Guidelines in Medicine. Ann Emerg Med. 2017;69:e27–e54. doi: 10.1016/j.annemergmed.2016.08.457. [DOI] [PubMed] [Google Scholar]
- 5.Frankel HL, Kirkpatrick AW, Elbarbary M, Blaivas M, Desai H, Evans D, Summerfield DT, Slonim A, Breitkreutz R, Price S, Marik PE, Talmor D, Levitov A. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part I: General Ultrasonography. Crit Care Med. 2015;43:2479–2502. doi: 10.1097/CCM.0000000000001216. [DOI] [PubMed] [Google Scholar]
- 6.Levitov A, Frankel HL, Blaivas M, Kirkpatrick AW, Su E, Evans D, Summerfield DT, Slonim A, Breitkreutz R, Price S, McLaughlin M, Marik PE, Elbarbary M. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part II: Cardiac Ultrasonography. Crit Care Med. 2016;44:1206–1227. doi: 10.1097/CCM.0000000000001847. [DOI] [PubMed] [Google Scholar]
- 7.Expert Round Table on Ultrasound in ICU. International expert statement on training standards for critical care ultrasonography. Intensive Care Med. 2011;37:1077–1083. doi: 10.1007/s00134-011-2246-9. [DOI] [PubMed] [Google Scholar]
- 8.Arntfield R, Millington S, Ainsworth C, Arora R, Boyd J, Finlayson G, Gallagher W, Gebhardt C, Goffi A, Hockman E, Kirkpatrick A, McDermid R, Waechter J, Wong N, Zavalkoff S, Beaulieu Y. Canadian recommendations for critical care ultrasound training and competency. Can Respir J. 2014;21:341–345. doi: 10.1155/2014/216591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henwood PC. Imaging an Outbreak - Ultrasound in an Ebola Treatment Unit. N Engl J Med. 2019;381:6–9. doi: 10.1056/NEJMp1902830. [DOI] [PubMed] [Google Scholar]
- 10.Kirkpatrick JN, Mitchell C, Taub C, Kort S, Hung J, Swaminathan M. ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak: Endorsed by the American College of Cardiology. J Am Coll Cardiol. 2020;75:3078–3084. doi: 10.1016/j.jacc.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johri AM, Galen B, Kirkpatrick JN, Lanspa M, Mulvagh S, Thamman R. ASE Statement on Point-of-Care Ultrasound during the 2019 Novel Coronavirus Pandemic. J Am Soc Echocardiogr. 2020;33:670–673. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guideline on COVID-19: Ultrasound Machine and Transducer Cleaning. Ann Emerg Med. 2020;76:e95–e97. doi: 10.1016/j.annemergmed.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim DJ, Jelic T, Woo MY, Heslop C, Olszynski P. Just the Facts: Recommendations on point-of-care ultrasound use and machine infection control during the coronavirus disease 2019 pandemic. CJEM. 2020;22:445–449. doi: 10.1017/cem.2020.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nyhsen CM, Humphreys H, Koerner RJ, Grenier N, Brady A, Sidhu P, Nicolau C, Mostbeck G, D'Onofrio M, Gangi A, Claudon M. Infection prevention and control in ultrasound - best practice recommendations from the European Society of Radiology Ultrasound Working Group. Insights Imaging. 2017;8:523–535. doi: 10.1007/s13244-017-0580-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bluemke DA, Meltzer CC. Ebola virus disease: radiology preparedness. Radiology. 2015;274:527–531. doi: 10.1148/radiol.14142502. [DOI] [PubMed] [Google Scholar]
- 16.Cheung JC, Ho LT, Cheng JV, Cham EYK, Lam KN. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020;8:e19. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ñamendys-Silva SA. Respiratory support for patients with COVID-19 infection. Lancet Respir Med. 2020;8:e18. doi: 10.1016/S2213-2600(20)30110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahmani F, Parsian Z, Shahsavarinia K, Pouraghaei M, Negargar S, Mehdizadeh Esfanjani R, Soleimanpour H. Diagnostic Value of Sonography for Confirmation of Endotracheal Intubation in the Emergency Department. Anesth Pain Med. 2017;7:e58350. doi: 10.5812/aapm.58350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das SK, Choupoo NS, Haldar R, Lahkar A. Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Can J Anaesth. 2015;62:413–423. doi: 10.1007/s12630-014-0301-z. [DOI] [PubMed] [Google Scholar]
- 20.Gottlieb M, Holladay D, Burns K, Gore SR, Wulff C, Shah S, Bailitz J. Accuracy of ultrasound for endotracheal intubation between different transducer types. Am J Emerg Med. 2019;37:2182–2185. doi: 10.1016/j.ajem.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 21.Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the Confirmation of Endotracheal Tube Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2018;72:627–636. doi: 10.1016/j.annemergmed.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 22.Blaivas M, Tsung JW. Point-of-care sonographic detection of left endobronchial main stem intubation and obstruction vs endotracheal intubation. J Ultrasound Med. 2008;27:785–789. doi: 10.7863/jum.2008.27.5.785. [DOI] [PubMed] [Google Scholar]
- 23.van Loon FHJ, Buise MP, Claassen JJF, Dierick-van Daele ATM, Bouwman ARA. Comparison of ultrasound guidance with palpation and direct visualisation for peripheral vein cannulation in adult patients: a systematic review and meta-analysis. Br J Anaesth. 2018;121:358–366. doi: 10.1016/j.bja.2018.04.047. [DOI] [PubMed] [Google Scholar]
- 24.Egan G, Healy D, O'Neill H, Clarke-Moloney M, Grace PA, Walsh SR. Ultrasound guidance for difficult peripheral venous access: systematic review and meta-analysis. Emerg Med J. 2013;30:521–526. doi: 10.1136/emermed-2012-201652. [DOI] [PubMed] [Google Scholar]
- 25.Shiloh AL, Savel RH, Paulin LM, Eisen LA. Ultrasound-guided catheterization of the radial artery: a systematic review and meta-analysis of randomized controlled trials. Chest. 2011;139:524–529. doi: 10.1378/chest.10-0919. [DOI] [PubMed] [Google Scholar]
- 26.Miller AG, Bardin AJ. Review of Ultrasound-Guided Radial Artery Catheter Placement. Respir Care. 2016;61:383–388. doi: 10.4187/respcare.04190. [DOI] [PubMed] [Google Scholar]
- 27.Weekes AJ, Keller SM, Efune B, Ghali S, Runyon M. Prospective comparison of ultrasound and CXR for confirmation of central vascular catheter placement. Emerg Med J. 2016;33:176–180. doi: 10.1136/emermed-2015-205000. [DOI] [PubMed] [Google Scholar]
- 28.Korsten P, Mavropoulou E, Wienbeck S, Ellenberger D, Patschan D, Zeisberg M, Vasko R, Tampe B, Müller GA. The "rapid atrial swirl sign" for assessing central venous catheters: Performance by medical residents after limited training. PLoS One. 2018;13:e0199345. doi: 10.1371/journal.pone.0199345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilson SP, Assaf S, Lahham S, Subeh M, Chiem A, Anderson C, Shwe S, Nguyen R, Fox JC. Simplified point-of-care ultrasound protocol to confirm central venous catheter placement: A prospective study. World J Emerg Med. 2017;8:25–28. doi: 10.5847/wjem.j.1920-8642.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gupta PK, Gupta K, Jain M, Garg T. Postprocedural chest radiograph: Impact on the management in critical care unit. Anesth Essays Res. 2014;8:139–144. doi: 10.4103/0259-1162.134481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsujimoto H, Tsujimoto Y, Nakata Y, Akazawa M, Kataoka Y. Ultrasonography for confirmation of gastric tube placement. Cochrane Database Syst Rev. 2017;4:CD012083. doi: 10.1002/14651858.CD012083.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brun PM, Chenaitia H, Lablanche C, Pradel AL, Deniel C, Bessereau J, Melaine R. 2-point ultrasonography to confirm correct position of the gastric tube in prehospital setting. Mil Med. 2014;179:959–963. doi: 10.7205/MILMED-D-14-00044. [DOI] [PubMed] [Google Scholar]
- 33.Xu B, Xing Y, Peng J, Zheng Z, Tang W, Sun Y, Xu C, Peng F. Chest CT for detecting COVID-19: a systematic review and meta-analysis of diagnostic accuracy. Eur Radiol. 2020;30:5720–5727. doi: 10.1007/s00330-020-06934-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, Chen B, Zhang Z, Guan W, Ling Z, Jiang R, Hu T, Ding Y, Lin L, Gan Q, Luo L, Tang X, Liu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Volpicelli G, Gargani L. Sonographic signs and patterns of COVID-19 pneumonia. Ultrasound J. 2020;12:22. doi: 10.1186/s13089-020-00171-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xirouchaki N, Magkanas E, Vaporidi K, Kondili E, Plataki M, Patrianakos A, Akoumianaki E, Georgopoulos D. Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med. 2011;37:1488–1493. doi: 10.1007/s00134-011-2317-y. [DOI] [PubMed] [Google Scholar]
- 38.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gomersall CD, Joynt GM, Lam P, Li T, Yap F, Lam D, Buckley TA, Sung JJ, Hui DS, Antonio GE, Ahuja AT, Leung P. Short-term outcome of critically ill patients with severe acute respiratory syndrome. Intensive Care Med. 2004;30:381–387. doi: 10.1007/s00134-003-2143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang W, Gao R, Zheng Y, Jiang L. COVID-19 with spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu K, Zeng Y, Xie P, Ye X, Xu G, Liu J, Wang H, Qian J. COVID-19 with cystic features on computed tomography: A case report. Medicine (Baltimore) 2020;99:e20175. doi: 10.1097/MD.0000000000020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012;5:76–81. doi: 10.4103/0974-2700.93116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sarwal A, Walker FO, Cartwright MS. Neuromuscular ultrasound for evaluation of the diaphragm. Muscle Nerve. 2013;47:319–329. doi: 10.1002/mus.23671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wait JL, Nahormek PA, Yost WT, Rochester DP. Diaphragmatic thickness-lung volume relationship in vivo. J Appl Physiol (1985) 1989;67:1560–1568. doi: 10.1152/jappl.1989.67.4.1560. [DOI] [PubMed] [Google Scholar]
- 45.McCool FD, Tzelepis GE. Dysfunction of the diaphragm. N Engl J Med. 2012;366:932–942. doi: 10.1056/NEJMra1007236. [DOI] [PubMed] [Google Scholar]
- 46.Jozwiak M, Monnet X, Teboul JL. Prediction of fluid responsiveness in ventilated patients. Ann Transl Med. 2018;6:352. doi: 10.21037/atm.2018.05.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Z, Xu X, Ye S, Xu L. Ultrasonographic measurement of the respiratory variation in the inferior vena cava diameter is predictive of fluid responsiveness in critically ill patients: systematic review and meta-analysis. Ultrasound Med Biol. 2014;40:845–853. doi: 10.1016/j.ultrasmedbio.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 48.Vignon P, Repessé X, Bégot E, Léger J, Jacob C, Bouferrache K, Slama M, Prat G, Vieillard-Baron A. Comparison of Echocardiographic Indices Used to Predict Fluid Responsiveness in Ventilated Patients. Am J Respir Crit Care Med. 2017;195:1022–1032. doi: 10.1164/rccm.201604-0844OC. [DOI] [PubMed] [Google Scholar]
- 49.Kimura BJ, Dalugdugan R, Gilcrease GW 3rd, Phan JN, Showalter BK, Wolfson T. The effect of breathing manner on inferior vena caval diameter. Eur J Echocardiogr. 2011;12:120–123. doi: 10.1093/ejechocard/jeq157. [DOI] [PubMed] [Google Scholar]
- 50.De Backer D, Fagnoul D. Intensive care ultrasound: VI. Fluid responsiveness and shock assessment. Ann Am Thorac Soc. 2014;11:129–136. doi: 10.1513/AnnalsATS.201309-320OT. [DOI] [PubMed] [Google Scholar]
- 51.Villavicencio C, Leache J, Marin J, Oliva I, Rodriguez A, Bodí M, Soni NJ. Basic critical care echocardiography training of intensivists allows reproducible and reliable measurements of cardiac output. Ultrasound J. 2019;11:5. doi: 10.1186/s13089-019-0120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patel AR, Patel AR, Singh S, Khawaja I. Cardiac Ultrasound in the Intensive Care Unit: A Review. Cureus. 2019;11:e4612. doi: 10.7759/cureus.4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, Vonk Noordegraaf A, Zamorano JL, Zompatori M Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033–3069, 3069a. doi: 10.1093/eurheartj/ehu283. [DOI] [PubMed] [Google Scholar]
- 54.Attaran RR, Ata I, Kudithipudi V, Foster L, Sorrell VL. Protocol for optimal detection and exclusion of a patent foramen ovale using transthoracic echocardiography with agitated saline microbubbles. Echocardiography. 2006;23:616–622. doi: 10.1111/j.1540-8175.2006.00272.x. [DOI] [PubMed] [Google Scholar]
- 55.Gupta SK, Shetkar SS, Ramakrishnan S, Kothari SS. Saline Contrast Echocardiography in the Era of Multimodality Imaging--Importance of "Bubbling It Right". Echocardiography. 2015;32:1707–1719. doi: 10.1111/echo.13035. [DOI] [PubMed] [Google Scholar]
- 56.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Squizzato A, Galli L, Gerdes VE. Point-of-care ultrasound in the diagnosis of pulmonary embolism. Crit Ultrasound J. 2015;7:7. doi: 10.1186/s13089-015-0025-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shao M, Li X, Liu F, Tian T, Luo J, Yang Y. Acute kidney injury is associated with severe infection and fatality in patients with COVID-19: A systematic review and meta-analysis of 40 studies and 24,527 patients. Pharmacol Res. 2020;161:105107. doi: 10.1016/j.phrs.2020.105107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Connor MJ Jr, Kraft C, Mehta AK, Varkey JB, Lyon GM, Crozier I, Ströher U, Ribner BS, Franch HA. Successful delivery of RRT in Ebola virus disease. J Am Soc Nephrol. 2015;26:31–37. doi: 10.1681/ASN.2014111057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cournac JM, Karkowski L, Bordes J, Aletti M, Duron S, Janvier F, Foissaud V, Savini H, de Greslan T, Rousseau C, Billhot M, Gagnon N, Mac Nab C, Dubrous P, Moroge S, Broto H, Cotte J, Maugey N, Cordier PY, Sagui E, Merens A, Rapp C, Quentin B, Granier H, Carmoi T, Cellarier G. Rhabdomyolysis in Ebola Virus Disease. Results of an Observational Study in a Treatment Center in Guinea. Clin Infect Dis. 2016;62:19–23. doi: 10.1093/cid/civ779. [DOI] [PubMed] [Google Scholar]
- 63.Panitchote A, Mehkri O, Hastings A, Hanane T, Demirjian S, Torbic H, Mireles-Cabodevila E, Krishnan S, Duggal A. Factors associated with acute kidney injury in acute respiratory distress syndrome. Ann Intensive Care. 2019;9:74. doi: 10.1186/s13613-019-0552-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barozzi L, Valentino M, Santoro A, Mancini E, Pavlica P. Renal ultrasonography in critically ill patients. Crit Care Med. 2007;35:S198–S205. doi: 10.1097/01.CCM.0000260631.62219.B9. [DOI] [PubMed] [Google Scholar]
- 65.Sullivan R, Baston CM. When Not to Trust the Bladder Scanner. The Use of Point-of-Care Ultrasound to Estimate Urinary Bladder Volume. Ann Am Thorac Soc. 2019;16:1582–1584. doi: 10.1513/AnnalsATS.201905-414CC. [DOI] [PubMed] [Google Scholar]
- 66.Zhang H, Liao YS, Gong J, Liu J, Xia X, Zhang H. Clinical characteristics of coronavirus disease (COVID-19) patients with gastrointestinal symptoms: A report of 164 cases. Dig Liver Dis. 2020;52:1076–1079. doi: 10.1016/j.dld.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kaafarani HMA, El Moheb M, Hwabejire JO, Naar L, Christensen MA, Breen K, Gaitanidis A, Alser O, Mashbari H, Bankhead-Kendall B, Mokhtari A, Maurer L, Kapoen C, Langeveld K, El Hechi MW, Lee J, Mendoza AE, Saillant NN, Parks J, Fawley J, King DR, Fagenholz PJ, Velmahos GC. Gastrointestinal Complications in Critically Ill Patients With COVID-19. Ann Surg. 2020;272:e61–e62. doi: 10.1097/SLA.0000000000004004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seitz K, Merz M. [Ultrasound ileus diagnosis] Ultraschall Med. 1998;19:242–249. doi: 10.1055/s-2007-1000499. [DOI] [PubMed] [Google Scholar]
- 69.Pourmand A, Dimbil U, Drake A, Shokoohi H. The Accuracy of Point-of-Care Ultrasound in Detecting Small Bowel Obstruction in Emergency Department. Emerg Med Int. 2018;2018:3684081. doi: 10.1155/2018/3684081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Suri S, Gupta S, Sudhakar PJ, Venkataramu NK, Sood B, Wig JD. Comparative evaluation of plain films, ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol. 1999;40:422–428. doi: 10.3109/02841859909177758. [DOI] [PubMed] [Google Scholar]
- 71.Cho J, Jensen TP, Reierson K, Mathews BK, Bhagra A, Franco-Sadud R, Grikis L, Mader M, Dancel R, Lucas BP Society of Hospital Medicine Point-of-care Ultrasound Task Force, Soni NJ. Recommendations on the Use of Ultrasound Guidance for Adult Abdominal Paracentesis: A Position Statement of the Society of Hospital Medicine. J Hosp Med. 2019;14:E7–E15. doi: 10.12788/jhm.3095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Whittaker A, Anson M, Harky A. Neurological Manifestations of COVID-19: A systematic review and current update. Acta Neurol Scand. 2020;142:14–22. doi: 10.1111/ane.13266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87:34–40. doi: 10.3171/jns.1997.87.1.0034. [DOI] [PubMed] [Google Scholar]
- 74.Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49:508–514. doi: 10.1016/j.annemergmed.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 75.Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10:376–381. doi: 10.1111/j.1553-2712.2003.tb01352.x. [DOI] [PubMed] [Google Scholar]
- 76.Toscano M, Spadetta G, Pulitano P, Rocco M, Di Piero V, Mecarelli O, Vicenzini E. Optic Nerve Sheath Diameter Ultrasound Evaluation in Intensive Care Unit: Possible Role and Clinical Aspects in Neurological Critical Patients' Daily Monitoring. Biomed Res Int. 2017;2017:1621428. doi: 10.1155/2017/1621428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mellor TE, Junga Z, Ordway S, Hunter T, Shimeall WT, Krajnik S, Tibbs L, Mikita J, Zeman J, Clark P. Not Just Hocus POCUS: Implementation of a Point of Care Ultrasound Curriculum for Internal Medicine Trainees at a Large Residency Program. Mil Med. 2019;184:901–906. doi: 10.1093/milmed/usz124. [DOI] [PubMed] [Google Scholar]