Abstract
Objective:
To identify patterns of technology-based weight-related self-monitoring (WRSM) and assess associations between identified patterns and eating disorder behaviors among first year university students.
Methods:
First year university students (n=647) completed a web-based survey to assess their use of technology-based WRSM and eating disorder behaviors. The cross-sectional data were analyzed using gender-stratified latent class analysis to identify patterns of WRSM, followed by logistic regression to calculate the predicted probability of eating disorder behaviors for each pattern of WRSM.
Results:
Technology-based WRSM is common among first year university students, with patterns of WRSM differing by student gender. Further, unique patterns of WRSM were associated with differing probability of engaging in eating disorder behaviors. For example, compared to the 67.0% of females who did not use technology-based WRSM, females engaging in high amounts of technology-based WRSM (33.0%) were more likely to report fasting, skipping meals, excessively exercising, and using supplements. Among males, those who reported all forms of WRSM (9.5%) were more likely to report fasting, skipping meals, purging, and using supplements but those who only used exercise self-monitoring (11.9%) did not have increased likelihood of eating disorder behaviors.
Conclusions:
Using multiple forms of technology-based WRSM is associated with increased likelihood of engaging in eating disorder behaviors among both female and male, first year university students. Assessing technology-based WRSM may be a simple method to screen for elevated eating disorder risk among first year students.
Keywords: eating disorders, self-monitoring, university, epidemiology, public health, prevention
Introduction
The “quantified self,” or using technology to monitor and manage health, is now common in day-to-day life. From continuous glucose monitors, to smart phones to application (app)-based mood journals, to wearable devices that measure and report sleep duration and quality, many people today use technology to track one or more aspects of their health.(1) Using technology to monitor ones’ weight, and the behaviors that may impact weight, has become particularly common. Wearable fitness trackers and other new technologies have increased the ease of weight-related self-monitoring (WRSM), popularizing the practice. For example, FitBit, a wearable device that tracks physical activity, reports 27.4 million active users every month.(2) Further, apps like MyFitnessPal, which has 19 million active users every month,(2) allows users to easily log their dietary intake and quickly compare their intake to calorie and macronutrient goals.
Technology-based WRSM is touted as a health management tool because it increases awareness of one’s behavior and promotes goal setting, which may lead to behavior change.(3) However, the practice may not be harmless. Of particular concern is whether technology-based WRSM increases the risk of eating disorders. Cross-sectional studies have found that calorie counting, which is often conducted using apps like MyFitnessPal, is associated with increased eating disorder risk among college students.(4–6) The increased attention that makes WRSM an effective means for behavior change may also be accompanied by increased self-criticism,(7, 8) which could lead to obsessional thinking related to one’s eating habits and body weight, and use of eating disorder behaviors. Using technology-based WRSM specifically may increase risk because it is primed to make tracking easier thereby further increasing awareness compared to traditional tracking methods. Prior research on technology-based WRSM found that the use of calorie, but not fitness tracking, apps was associated with binge eating and purging.(4) However, two-thirds of those who used calorie tracking apps also used fitness tracking apps. While the study did not examine whether using multiple WRSM technologies simultaneously alters eating disorder risk compared to each independent behavior, it is possible that there may be differing risk if engaging in multiple forms of WRSM simultaneously or that different forms of WRSM would be associated with differential risk when used together.
College students are particularly frequent users of technology-based WRSM(1, 4, 9) and are at high risk for eating disorders.(10, 11) In a recent study of college students, 40% reported binge eating and 30% used a compensatory behavior such as compulsive exercise, vomiting, laxative or diuretic misuse, or diet pills in the past four weeks.(11) Preventing and treating these behaviors is of great public health importance given the known mental and physical health consequences of eating disorders and eating disorder behaviors including: decreased educational attainment(12) and classroom impairment,(13) increased likelihood of binge drinking,(14) substance abuse,(15) increased psychological distress over time,(16) gastrointestinal problems,(17) and other physiological problems.(18)
Given that little is known about how college students are using technology-based WRSM and how use is related to engagement in eating disorder behaviors, the objective of this study was to characterize how first-year college students use technology-based WRSM and identify associations between patterns of technology-based WRSM and eating disorder behaviors. We hypothesized that males and females would use technology-based WRSM differently, and that different patterns of WRSM would be associated with differential eating disorder risk. Study results can help inform eating disorder screening on college campuses and public health messaging regarding technology-based WRSM among young adults.
Methods
Participants
Data for the current study come from a web-based survey of nutrition and weight control behaviors among first year university students. The survey was conducted in January 2017 and included first year students, 18–22 years of age, at all three campuses of a large state university in the midwestern United States. Invitations to complete the survey were distributed via email to a random sample of 2,000 first year students at the main campus, and all first year students at the other two campuses (approximately 1,600 students combined). Eight hundred and thirteen students across the 3 campuses initiated the survey, a response rate of approximately 23%. Participants who did not respond to at least 50% of the questions examined in this analysis were excluded (n=158), resulting in 655 participants with sufficient data. Body mass index (BMI) was calculated from self-reported height and weight, and students with biologically implausible height, weight, or BMI were also excluded from the analytic sample (n=4).(19–21) Students who identified as a gender other than male or female were excluded from the analysis due to the inability to make valid inferences as a result of a small sample size (n=4), resulting in a final analytic sample size of 647 students.
Measures
Weight-Related Self-Monitoring (WRSM).
Common forms of technology-based WRSM assessed on the survey were identified by the study team through interviews with nutrition, medical, and psychology professionals who work with adolescents and young adults (n=12), a focus group of male first year university students, and a focus group of college-aged females. To then measure technology-based WRSM among participants, the survey first asked, “In the past year, have you used any apps or other technology, such as a Fitbit or MyFitnessPal, to monitor what you are eating, your exercise, or your weight?” If respondents answered “yes” they were asked, “Please indicate which apps and/or technology you used in the past year and how you used them (select all that apply)” with response options of: “Wearable fitness tracker (e.g. Fitbit, Jawbone, Garmin),” “Online or digital exercise log (e.g. MapMyRun, MyFitnessPal),” “Online or digital food log (e.g. MyFitnessPal, CalorieKing),” “Weight monitoring app/technology (e.g. iLostWhat or WIFI-connected scale),” and “An app or website for a specific diet or exercise plan (e.g. Kayla Itsines BBG, 21 day fix, etc.).” Because self-weighing often uses digital scales, and many individuals likely keep track of their weights within apps used primarily for other purposes, self-weighing was also assessed with the question, “How often do you weigh yourself?” with response options of: “Never,” “Every month or less,” “A few times per month,” “Every week,” “A few times per week,” “Every day,” and “More than once per day.” Respondents who reported that they weighed themselves once per week or more were categorized as engaging in frequent self-weighing, aligning with previous research.(22–24)
Eating Disorder Behaviors.
To assess eating disorder behaviors, we used a modified version of the assessments used by Project EAT which is an existing, frequently used measure with high test-retest agreement.(25–27) Questions were modified based on the aforementioned interviews with professionals and focus groups with college students to include more modern examples of weight management behaviors. In the survey, study participants were first asked, “How often have you done any of the following things in order to lose weight, keep from gaining weight, or change your body composition or shape during the past year?” The following behaviors were included: “Fasted (not eating for 24 hour or more),” “skipped meals,” “took diet pills,” “took laxatives,” “took diuretics/water pills,” “vomited after eating,” “excessively exercised,” and “used supplements or other products (protein powders, pre-workout, steroids, prescription drugs, ItWorks, waist trainers, etc.).” Response options included, “often,” “sometimes,” “rarely,” and “never”. Participants were categorized as using each of the behaviors if they indicated that they had used the behavior rarely or more often, as any use in the last year could be considered problematic. Use of diet pills, laxatives, diuretics, and/or vomiting were combined to a single variable of “purging or appetite suppressing”, which was considered positive with any use of any of the behaviors; all other behaviors were examined separately.
Sociodemographics and BMI.
To assess age, we used the question: “What is your age?” which had response options of 18–22. Based on distribution of the data, we dichotomized responses to 18 versus 19–22 years old. Gender was dichotomized into male and female and those who identified as another gender were excluded due to insufficient sample size. Ethnic/racial structured categories were assessed by the question, “What is your race/ethnicity? Select all that apply.” Response options included: “White,” “Hispanic or Latino,” “Black or African American,” “American Indian or Alaska Native,” “Asian/Pacific Islander,” “Middle Eastern/North African,” and “Other”. Any student who selected “Hispanic or Latino” were considered Hispanic/Latinx, all others who selected “Other,” more than one race/ethnicity, “American Indian or Alaska Native,” or “Middle Eastern/North American,” were included in the “Other” category of the ethnic/racial structured categories. Highest parental education was assessed using two questions 1) “How far in school did your mother go? (Mark the highest level),” and “How far in school did your father go? (Mark the highest level).” These two variables were combined to a single variable indicating the highest education level achieved by either parent, condensed to: high school or less, some college or training, bachelor’s degree, and graduate degree. Participants reported their height and weight, from which their BMI was calculated. Calculated BMIs were then categorized into the standard categories: less than 18.5, 18.5–24.9, 25–29.9, and 30 or above.(28)
Statistical Analyses
All analyses were performed using SAS 9.4 (Cary, NC) and STATA 16. Gender-stratified analyses were conducted based upon a priori hypotheses that WRSM patterns would differ by gender.(9, 29) Univariate and bivariate statistics were calculated for all methods of WRSM and eating disorder behaviors by gender. Latent class analysis (LCA) was used to identify gender-specific profiles of WRSM. All forms of WRSM assessed were included independently in the LCA. Because the seed used in PROC LCA(30) has the potential to impact the results, for each gender, one thousand randomly selected seeds were run for two through six classes. We then used Akaike’s Information Criterion (AIC), Bayesian Information Criteria (BIC), adjusted BIC, entropy, and interpretability to select the best fitting models for each gender.(30)
After establishing the patterns of use, sociodemographic characteristics of participants belonging to each of the identified patterns were examined. Chi-square, and Fisher’s exact tests were used to test for differences in pattern membership by categorical sociodemographic variables and ANOVA was used to examine mean BMI differed across patterns. Results for overall tests were considered statistically significant if p<.05. If significant, post hoc pairwise comparisons were conducted within rows to identify differences in the sociodemographic characteristics of members of each identified pattern. Post hoc pairwise comparisons were considered statistically significant at p<.01 to reduce the likelihood of type 1 error.
Logistic regression models were developed to assess the relationships between identified patterns of WRSM and eating disorder behaviors. Age, race/ethnicity, parental education and BMI were included in models as potential confounders.(11, 31–34) The predicted probabilities of eating disorder behaviors by identified pattern were calculated and pairwise comparisons conducted to identify differences in the probability of eating disorder behaviors between patterns of WRSM. Differences were determined to be statistically significant if p<.05.
Results
Description of the Study Sample
Approximately two thirds (68.9%) of the sample identified as female (Table 1). The sample was predominantly non-Hispanic White (66.0%), 5.0% identified as non-Hispanic Black or African American, 5.7% Hispanic/Latinx, 12.2% non-Hispanic Asian, and 11.1% another race or ethnicity. Nearly fifty percent of students had a parent with a graduate degree (49.2%), 32.8% had a parent with a bachelor’s degree, 10.6% had a parent with some college or training, and 7.5% had parents with a high school degree or less. The average BMI was 23.4 (standard deviation (SD) = 4.4); 5.1% had a BMI less than 18.5, 70.6% had a BMI between 18.5–24.9, 17.0% had a BMI between 25–29.9, and 7.3% had a BMI of 30 or above. Approximately two thirds of the sample were 18 years old (63.4%), and 36.6% were 19–22 years of age.
Table 1.
Sociodemographic characteristics of the study sample overall and by gender
| Overall (n=647) | Females (n=446) | Males (n=201) | |
|---|---|---|---|
| Prevalence % | |||
| Race/Ethnicity | |||
| White | 66.0 | 66.8 | 64.2 |
| Black or African American | 5.0 | 4.9 | 5.0 |
| Hispanic/Latino | 5.7 | 5.2 | 7.0 |
| Asian | 12.2 | 12.8 | 11.0 |
| Other | 11.1 | 10.3 | 12.9 |
| Parent Education | |||
| High school or less | 7.5 | 8.8 | 4.5 |
| Some college or training | 10.6 | 10.8 | 10.1 |
| Bachelor’s degree | 32.8 | 32.4 | 33.7 |
| Graduate degree | 49.2 | 48.1 | 51.8 |
| BMI Category | |||
| <18.5 | 5.1 | 6.1 | 3.0 |
| 18.5–24.9 | 70.6 | 69.2 | 73.5 |
| 25–29.9 | 17.0 | 15.8 | 19.5 |
| ≥30.0 | 7.3 | 8.8 | 4.0 |
| Age | |||
| 18 | 63.4 | 64.8 | 60.2 |
| 19–22 | 36.6 | 35.2 | 39.8 |
| Mean (SD) | |||
| BMI | 23.3 (4.4) | 23.4 (4.6) | 23.3 (4.0) |
BMI = body mass index; SD = Standard Deviation
Females were more likely than males to use an online fitness tracker (41.8% vs 20.5%, p<.0001) and online food journals (37.7% vs 16.0%, p<.0001) (Table 2). No differences were observed in the proportion of participants of using an app for a specific diet/exercise plan, using a wearable fitness tracker, self-weighing, or using a weight tracking app by gender. Females were more likely to skip meals for weight loss than males (62.7% vs 48.5%, p=0.0007), and males were more likely than females to excessively exercise (61.6% vs 47.6%, p=.001) and use supplements (54.5% vs 20.7%, p<.0001).
Table 2.
Prevalence of exposure and outcome variables overall and by gender
| Overall | Female | Male | p-value | |
|---|---|---|---|---|
| Prevalence % | ||||
| Weight-related self-monitoring (WRSM) | ||||
| App for a Specific Diet/Exercise Plan | 11.0 | 11.5 | 9.9 | .59 |
| Wearable Fitness Tracker | 28.2 | 29.5 | 25.3 | .30 |
| Online Fitness Tracker | 35.4 | 41.8 | 20.5 | <.0001 |
| Online Food Journal | 31.3 | 37.7 | 16.0 | <.0001 |
| Frequently Weigh | 20.4 | 18.9 | 23.9 | .14 |
| Weight Tracking app | 6.2 | 6.4 | 5.9 | .82 |
| Eating disorder behaviors | ||||
| Fasted | 15.4 | 16.9 | 12.1 | .12 |
| Skipped Meals | 58.3 | 62.7 | 48.5 | .0007 |
| Purging or Appetite Suppressing | 11.5 | 12.4 | 9.6 | .31 |
| Excessively Exercised | 52.0 | 47.6 | 61.6 | .001 |
| Supplement Use | 31.2 | 20.7 | 54.5 | <.0001 |
Latent Class Analysis (LCA) and Sociodemographic Characteristics by Identified Patterns
Females.
Using fit statistics and interpretability, we found that a model identifying two patterns of WRSM was best (Table 3). The probability of each WRSM behavior by latent class can be found in Figure 1. Latent Class 1 was characterized by low probability of all forms of WRSM (identified as “no WRSM”) and comprised 67.0% of the sample. Latent Class 2 was characterized by medium to high probability of all forms of WRSM (identified as “high WRSM”) and made up 33.0% of the sample. Bivariate analyses between identified patterns and sociodemographic characteristics can be found in Table 4. BMI differed by class (X2=16.9, p=.0007) with those with a BMI ≥ 30 were more likely to be in the “high WRSM” pattern (p<.01) compared to the “no WRSM” pattern, and the average BMI was higher in the “high WRSM” pattern (mean=24.9, SD=5.3) compared to the “no WRSM” pattern (mean=22.6, SD=4.1, p<.0001). There were no differences in race/ethnicity, parent education or age by identified pattern.
Table 3.
Women LCA Fit statistics
| Number of Classes | AIC | BIC | aBIC | Entropy |
|---|---|---|---|---|
| 2 | 73.44 | 126.74 | 85.49 | 0.73 |
| 3 | 73.28 | 155.28 | 91.81 | 0.71 |
| 4 | 77.45 | 188.15 | 102.47 | 0.71 |
| 5 | 84.52 | 223.93 | 116.03 | 0.75 |
| 6 | 94.19 | 262.30 | 132.19 | 0.78 |
LCA = Latent Class Analysis; AIC = Akaike’s Information Criterion; BIC = Bayesian
Information Criteria; aBIC = adjusted Bayesian Information Criteria.
Figure 1.
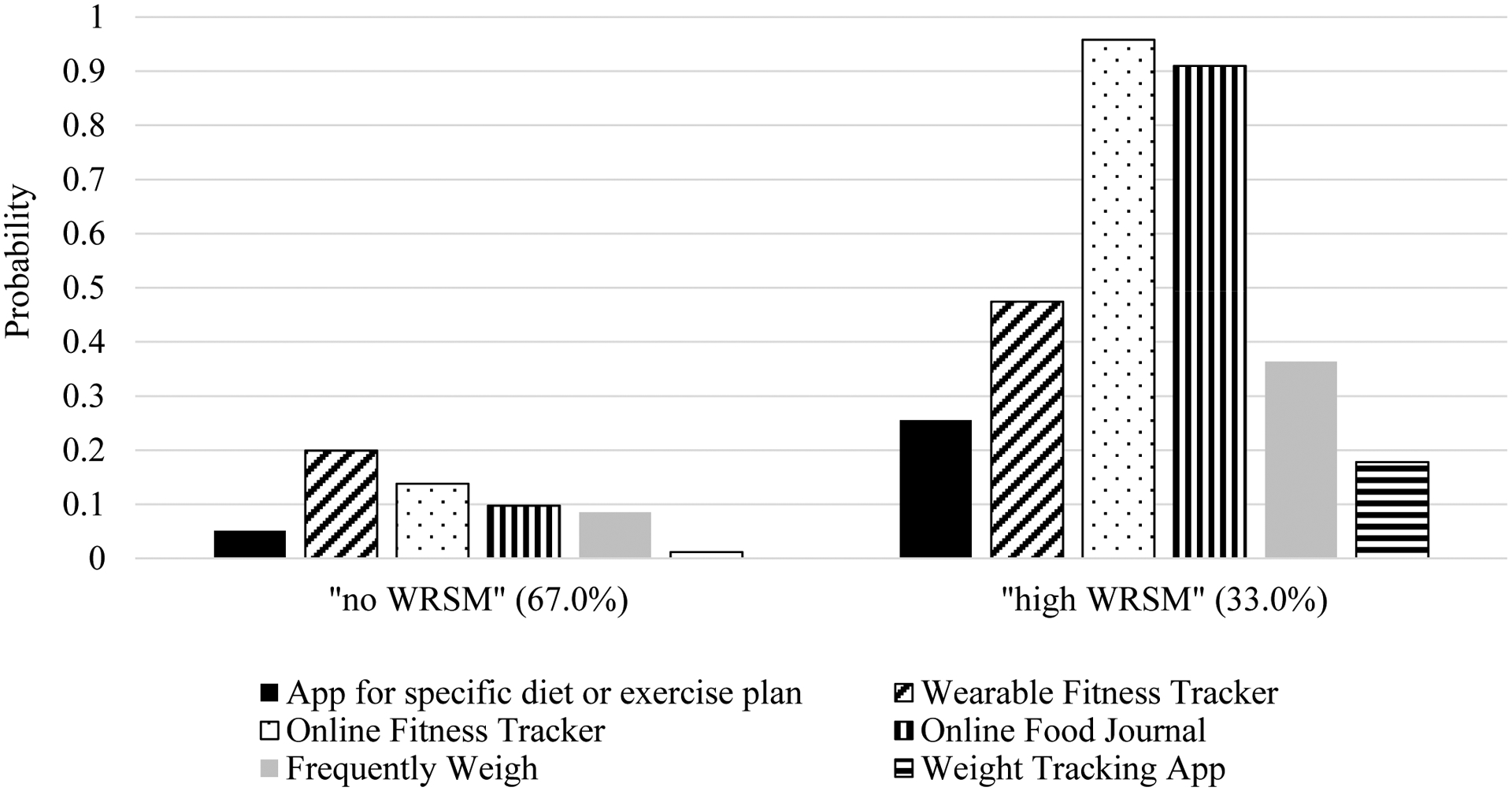
Probability estimates of each type of weight-related self-monitoring (WRSM) for each identified pattern of WRSM for females. Percentages represent proportion of population that are categorized into that identified pattern.
Table 4.
Overall prevalence and associations between sociodemographic characteristics and weight-related self-monitoring (WRSM) patterns among females
| Demographic | Overall | “no WRSM” | “high WRSM” | p-value |
|---|---|---|---|---|
| Overall prevalence | 299 (67.0) | 147 (33.0) | ||
| Race/Ethnicity | .78 | |||
| White | 298 (66.8) | 199 (66.6) | 99 (67.4) | |
| Black or African | 22 (4.9) | 13 (4.4) | 9 (6.1) | |
| American | ||||
| Hispanic/Latina | 23 (5.2) | 14 (4.7) | 9 (6.1) | |
| Asian | 57 (12.8) | 40 (13.4) | 17 (11.6) | |
| Other | 46 (10.3) | 33 (11.0) | 13 (8.8) | |
| Parent Education | .57 | |||
| High school or less | 39 (8.8) | 27 (9.1) | 12 (8.2) | |
| Some college or training | 48 (10.8) | 34 (11.4) | 14 (9.5) | |
| Bachelor’s degree | 144 (32.4) | 90 (30.2) | 54 (36.7) | |
| Graduate degree | 214 (48.1) | 147 (49.3) | 67 (45.6) | |
| BMI Category | .0007 | |||
| <18.5 | 27 (6.1) | 24 (8.1) a | 3 (2.0) a | |
| 18.5–24.9 | 306 (69.2) | 211 (71.5) a | 95 (64.6) a | |
| 25–29.9 | 70 (15.8) | 43 (14.6) a | 27 (18.4) a | |
| ≥30.0 | 39 (8.8) | 17 (5.8) a | 22 (15.0) b | |
| Age | .79 | |||
| 18 | 289 (64.8) | 104 (34.8) | 53 (36.1) | |
| 19–22 | 157 (35.2) | 195 (65.2) | 94 (64.0) | |
| Mean (SD) | ||||
| BMI | 23.4 (4.6) | 22.6 (4.1) a | 24.9 (5.3) b | <.0001 |
Superscripts are results of pairwise comparisons of proportions across identified patterns of WRSM within a row at p<.01; the same letter present at each prevalence indicates lack of statistical difference.
WRSM = weight-related self-monitoring; BMI = body mass index; SD = standard deviation
Males.
A model identifying three patterns of WRSM was deemed superior based on fit statistics and interpretability (Table 5). The probability of each form of WRSM by identified patterns can be found in Figure 2. Latent Class 1 was characterized by low probability of all forms of WRSM (identified as “no WRSM”) and made up 78.6% of the sample. Latent Class 2 was characterized by high probability of using a wearable fitness tracker and online fitness tracker, but not using an app for a specific diet/exercise plan, online food journals, frequently weighing, or using a weight tracking app (identified as “exercise self-monitoring”) and made up 11.9% of the sample. Latent class 3 was characterized by a high probability of all forms of WRSM (identified as “all WRSM”) and made up 9.5% of the sample. Participant race/ethnicity, parent education, age, and BMI category did not differ across the identified patterns (Table 6). Average BMI was higher among participants in the “all weight-related self-monitoring” class (mean=25.6, SD=6.3) compared to the “no weight-related self-monitoring” class (mean=23.0, SD=3.6).
Table 5.
Men LCA Fit statistics
| Number of Classes | AIC | BIC | aBIC | Entropy |
|---|---|---|---|---|
| 2 | 80.05 | 122.99 | 81.80 | 0.78 |
| 3 | 75.02 | 141.09 | 77.72 | 0.85 |
| 4 | 80.87 | 170.06 | 84.52 | 0.89 |
| 5 | 88.51 | 200.82 | 93.10 | 0.86 |
| 6 | 97.77 | 233.21 | 274.21 | 0.86 |
LCA = Latent Class Analysis; AIC = Akaike’s Information Criterion; BIC = Bayesian
Information Criteria; aBIC = adjusted Bayesian Information Criteria.
Figure 2.
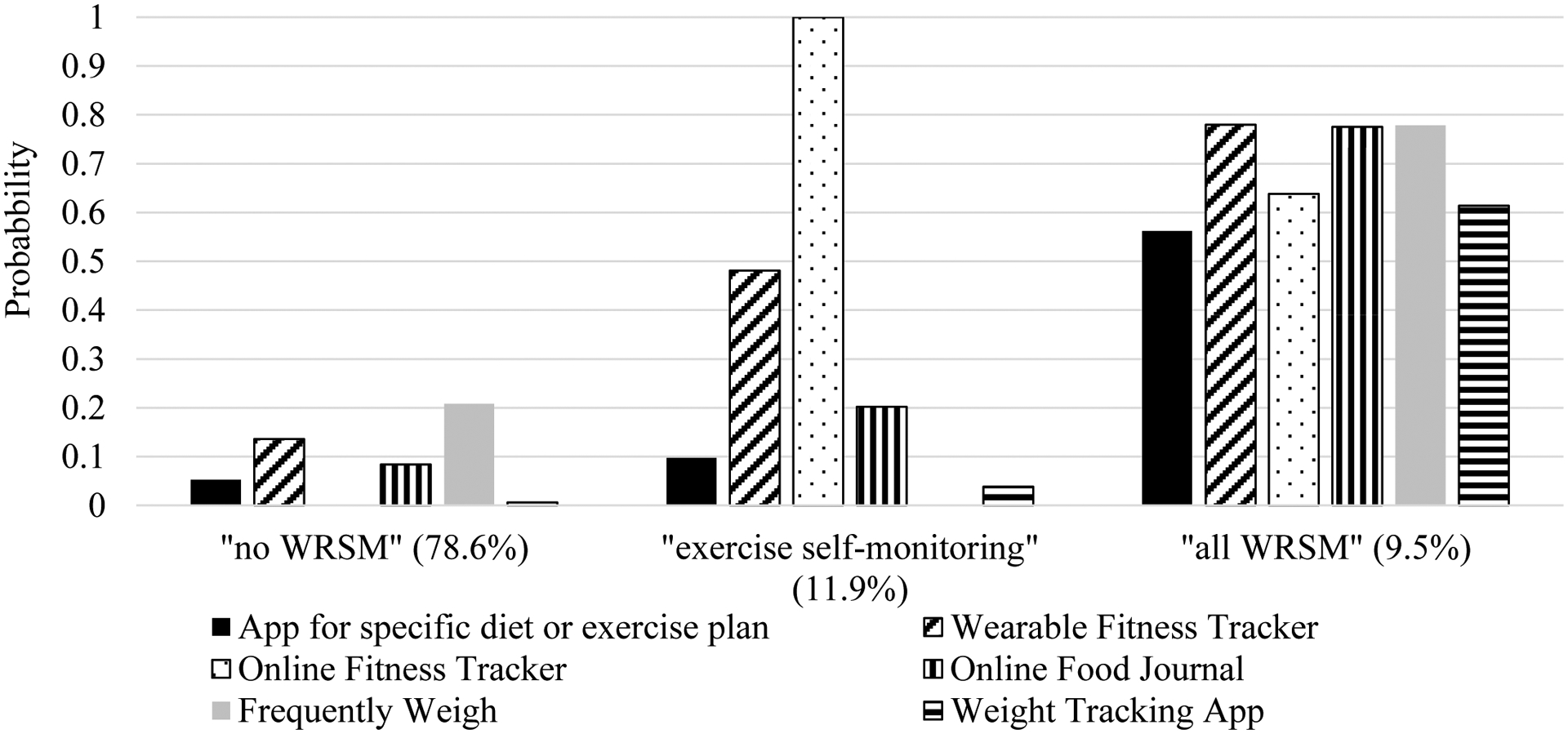
Probability estimates of each type of weight-related self-monitoring (WRSM) for each identified pattern of WRSM for males. Percentages represent proportion of population that are categorized into that identified pattern.
Table 6.
Overall prevalence and associations between sociodemographic characteristics and weight-related self-monitoring (WRSM) patterns among males
| Demographic | Overall | “no WRSM” | “exercise self-monitoring” | “all WRSM” | p-value |
|---|---|---|---|---|---|
| n (%) | |||||
| Overall prevalence | 158 (78.6) | 24 (11.9) | 19 (9.5) | ||
| Race/Ethnicity | 0.56 | ||||
| White | 129 (64.2) | 103 (65.2) | 16 (66.7) | 10 (52.6) | |
| Black or African | 10 (5.0) | 7 (4.4) | 1 (4.2) | 2 (10.5) | |
| American | |||||
| Hispanic/Latino | 14 (7.0) | 9 (5.7) | 2 (8.3) | 3 (15.8) | |
| Asian | 22 (11.0) | 19 (12.0) | 1 (4.2) | 2 (10.5) | |
| Other | 26 (12.9) | 20 (12.7) | 4 (167) | 2 (10.5) | |
| Parent Education | 0.79 | ||||
| High school or less | 9 (4.5) | 8 (5.1) | 0 (0.0) | 1 (5.3) | |
| Some college or training | 20 (10.1) | 14 (9.0) | 3 (12.5) | 3 (15.8) | |
| Bachelor’s degree | 67 (33.7) | 53 (34.0) | 7 (29.2) | 7 (36.8) | |
| Graduate degree | 103 (51.8) | 81 (51.9) | 14 (58.3) | 8 (42.1) | |
| BMI Category | 0.45 | ||||
| <18.5 | 6 (3.0) | 6 (3.8) | 0 (0.0) | 0 (0.0) | |
| 18.5–24.9 | 147 (73.5) | 118 (75.2) | 16 (66.7) | 13 (68.4) | |
| 25–29.9 | 39 (19.5) | 28 (17.8) | 7 (29.2) | 4 (21.1) | |
| ≥30.0 | 8 (4.0) | 5 (3.2) | 1 (4.2) | 2 (10.5) | |
| Age | 0.17 | ||||
| 18 | 121 (60.2) | 94 (59.5) | 18 (75.0) | 9 (47.4) | |
| 19–22 | 80 (39.8) | 64 (40.5) | 6 (25.0) | 10 (52.6) | |
| Mean (SD) | |||||
| BMI | 23.3 (4.0) | 23.0 (3.6) a | 24.0 (3.6) a b | 25.6 (6.3) b | 0.02 |
Superscripts are results of pairwise comparisons of proportions across identified patterns of WRSM within a row at p<.01; the same letter present at each prevalence indicates lack of statistical difference.
WRSM = weight-related self-monitoring; BMI = body mass index; SD = standard deviation
Predicted Probabilities
Females.
Female participants in the “high WRSM” class had a higher predicted probability of fasting, skipping meals, excessively exercising, and using supplements compared to those in the “no weight-related self-monitoring” class (Table 5). There were no differences in the predicted probability of purging or using appetite suppressants across classes.
Males.
Compared to males in the “no WRSM” pattern, males who were in the “all WRSM” pattern were more likely to report fasting, skipping meals, purging, and using supplements but not excessively exercising (Table 6). Among those classified into the “exercise self-monitoring” class, there was not a significant difference in predicted probability of any disordered eating behavior compared to those in the “no WRSM” class. However, when compared to the “all WRSM” class, those in the “exercise self-monitoring” class had a statistically significant lower probability of skipping meals, but no other eating disorder behavior. However, large effect estimates that were not statistically significant were seen for other behaviors such as fasting (4.8% for “exercise self-monitoring” versus 29.5% for “all WRSM” pattern) and supplement use (“53.2% for “exercise self-monitoring” versus 82.9% for “all WRSM” pattern).
Discussion
The objective of the study was to characterize the ways that first year university students use technology-based WRSM and to examine the relationships between patterns of WRSM use and eating disorder behaviors. Nearly half (43.2%) of females and one quarter (21.4%) of males used multiple forms of technology-based WRSM. Among females, those who engaged in multiple forms of of technology-based WRSM were more likely to report fasting, skipping meals, excessive exercise, and supplement use compared to those who did not use technology-based WRSM. Among males, the three identified patterns of WRSM were each associated with differential probability of eating disorder behaviors with the highest predicted probability of engaging in fasting, skipping meals, purging, and supplement use among those who use all forms of WRSM.
Findings from the present study build upon prior studies of technology-based WRSM among university students. Similar to prior studies that reported widespread use of apps or devices to count calories or physical activity,(4, 9) we similarly found use of online food journals (31.3%), online fitness trackers (35.4%), and wearable fitness trackers (28.2%) to be common. Using an app specifically for weight tracking was uncommon however, (6.3%) suggesting that self-weighing is either being conducted within apps whose main purpose is not self-weighing but allows for tracking self-weighing (i.e. MyFitnessPal or Fitbit), or that individuals engaging in self-weighing are not using apps to keep track of their weight. The current study also extended prior research, identifying that technology-based WRSM methods are often used together.(4) Examining the use of these methods in combination therefore is essential to understanding how the general population may be impacted by their use. The highest predicted probability of eating disorder behavior use among both male and female first year university students who engage in multiple forms of technology-based WRSM suggests that colleges may be able to screen for WRSM to identify students at high risk for eating disorders. It is possible that technology-based WRSM contributes to the onset use of eating disorder behaviors and therefore could be targeted in prevention efforts. Alternatively, if the relationship between technology-based WRSM and eating disorder behaviors is confounded by shared risk factors and is not causal, screening for WRSM may still serve as an risk indicator in population based screening. Additionally, individuals may be less reluctant to disclose WRSM compared to eating disorder behaviors; therefore, providing resources to those who engage in WRSM instead of only those who endorse eating disorder behaviors may allow for colleges to reach a higher proportion of students in need of support.
Similar to prior studies, we found that WRSM patterns differed among by gender and the present study adds to the literature on both technology-based WRSM and eating disorder behaviors among males. Approximately 20% of males reported using multiple forms of technology-based WRSM, though the current study may have been underpowered to detect statistical differences in eating disorder behaviors among males by patterns of technology-based WRSM, specifically the differences in those identified in the “exercise self-monitoring” pattern compared to the other two classes. Given that body ideals for men are often lean and muscular,(35–37) and reaching this ideal would often involve physical activity, it may be hypothesized that exercise self-monitoring would be associated with eating disorder behaviors which are strongly linked to these body ideals. Interestingly, however, we did not see any meaningful differences irrespective of statistical significance in the likelihood of engaging in eating disorder behaviors among males in the “exercise self-monitoring” pattern. It is possible that the types of physical activity tracked using exercise self-monitoring do not align with the types of exercise behaviors used by first year university students to achieve the unrealistic body ideals. Further research examining the associations between technology-based WRSM and eating disorder behaviors among males is warranted.
This study has a number of strengths. First, by examining females and males separately we were able to identify gender-specific patterns of technology-based WRSM and examine gender-specific relationships between WRSM and eating disorder behaviors. Males in particular are understudied with respect to eating disorders.(38) Moreover, we assessed technology-based WRSM methods that our formative research indicated are common among young adults but have not been previously studied, such as apps for a specific diet/exercise plan and weight tracking apps. Examining novel forms of WRSM allows us to gain a further understanding of how young adults are using these tools and identify associations with their use. We also assessed first year students from three campuses of a large midwestern university which made the sample more diverse in socioeconomic status and race/ethnicity. Additionally, we assessed the critical transitionary period between high school and college which is a unique developmental period, and also has important public health implications.
However, the study is not without limitations. Single item measures were used to assess WRSM and eating disorder behaviors. We were also unable to examine differences in WRSM between some race/ethnicity categories due to limited sample size and individuals in the Hispanic/Latinx category may be heterogeneous with respect to race. Further, because of sample size and need for stratification, we were unable to examine the relationships between WRSM and eating disorder behaviors in gender minorities, which are a population at high risk for using eating disorder behaviors.(11) Further, while the use of LCA allowed us to examine patterns of WRSM and associations with eating disorder behaviors, the methodology used may result in slight biases in classification such that individuals may be inaccurately assigned to an identified pattern and therefore biasing associations with eating disorder behaviors. Additionally, our response rate was 23%. Though this is similar to other online surveys conducted among college students, it is possible that those who responded to the survey are different than the general population of first year college students which may ultimately skew results. Therefore, our results may not be generalizable to the general population of first year college students.(39–41) The study was also cross-sectional, and thus the results cannot establish causality. Therefore, it is possible that WRSM causes engagement in eating disorder behaviors, that WRSM may be a maintenance factor of eating disorder behaviors, or that eating disorder behavior engagement may proceed use of WRSM. Additionally, because WRSM and eating disorder behaviors were assessed for any use in the last year, it is possible that some individuals may have used these behaviors before their first year at university. Future studies should assess temporality and causal impacts of technology-based WRSM and eating disorder behaviors using longitudinal studies and randomized controlled trials. Particular focus should be paid to understand if there are periods before or during college in which young people are particularly vulnerable, or if there are differences in trajectories based on how individuals are engaging with WRSM, for example length of time, rigor, or motivation of use.
The current study provides in depth understanding of how first year university use technology-based WRSM and whether different patterns of technology-based WRSM are associated with eating disorder behaviors. Many first year university students, particularly females, engage in technology-based WRSM, often using multiple methods together. Using multiple forms of technology-based WRSM may increase eating disorder behavior among this population, though temporality and causality cannot be established with the present study. While additional research is needed to determine the mechanisms underlying these relationships, universities may benefit from providing students who use multiple forms of technology-based WRSM increased access to eating disorder prevention programming.
Table 7.
Predicted probability of eating disorder behavior by weight-related self-monitoring (WRSM) pattern among females
| Fasted | Skipped Meals | Purging and Appetite Suppressing | Excessive Exercise | Supplement Use | |
|---|---|---|---|---|---|
| “no WRSM” | 12.5%a | 55.2%a | 11.6%a | 37.2%a | 15.7%a |
| “all WRSM” | 25.5%b | 78.2%b | 13.4%a | 67.7%b | 31.5%b |
Superscripts are results of pairwise comparisons obtained via odds ratios comparing within column probabilities at p<.05; the same letter present at each prevalence indicates lack of statistical difference. Models adjusted for age, BMI, parent education, and race/ethnicity.
Table 8.
Predicted probability of eating disorder behavior by weight-related self-monitoring pattern (WRSM) among males
| Fasted | Skipped Meals | Purging and Appetite Suppressing | Excessive Exercise | Supplement Use | |
|---|---|---|---|---|---|
| “no WRSM” | 11.2%a | 46.7%a | 9.5%a | 58.8%a | 51.2%a |
| “exercise self-monitoring” | 4.8%a,b | 40.5%a | ---† | 61.4%a | 53.2%a,b |
| “all WRSM” | 29.5%b | 72.2%b | 28.3%b | 64.7%a | 82.9%b |
Superscripts are results of pairwise comparisons obtained via odds ratios comparing within column probabilities at p<.05; the same letter present at each prevalence indicates lack of statistical difference. Models adjusted for age, BMI, parent education, and race/ethnicity.
No males in the “exercise self-monitoring” class engaged in purging or appetite suppressing and therefore predicted probability could not be calculated.
Highlights.
Using technology to self-monitor is common among first year university students
Males and females use WRSM1 technologies differently
WRSM is associated with increased risk of eating disorder behaviors
Different patterns of use of WRSM were associated with unique risk profiles
Role of Funding Sources
This research was supported by a pilot grant from the Michigan Nutrition Obesity Research Center (NIH P30 DK089503). SLH’s time was also supported by the University of Michigan Rackham Predoctoral Fellowship and the National Institute of Mental Health (T32MH082761, PI: Scott Crow). The funding sources had no role in study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors have no conflicts of interest to declare.
WRSM = weight-related self-monitoring
References
- 1.Fox S & Duggan M (2012) Mobile Health 2012. Mobile Health. Pew Research Center.
- 2.Verto Analytics (2018) Most popular health and fitness apps in the United States as of May 2018, by monthly active users (in millions). https://www.statista.com/statistics/650748/health-fitness-app-usage-usa/ (accessed April 1, 2019)
- 3.Bandura A (1998) Health promotion from the perspective of social cognitive theory. Psychology & Health 13, 623–649. [Google Scholar]
- 4.Simpson CC & Mazzeo SE (2017) Calorie counting and fitness tracking technology: Associations with eating disorder symptomatology. Eat Behav 26, 89–92. [DOI] [PubMed] [Google Scholar]
- 5.Plateau CR, Bone S, Lanning E et al. (2018) Monitoring eating and activity: Links with disordered eating, compulsive exercise, and general wellbeing among young adults. Int J Eat Disord 51, 1270–1276. [DOI] [PubMed] [Google Scholar]
- 6.Romano KA, Swanbrow Becker MA, Colgary CD et al. (2018) Helpful or harmful? The comparative value of self-weighing and calorie counting versus intuitive eating on the eating disorder symptomology of college students. Eat Weight Disord 23, 841–848. [DOI] [PubMed] [Google Scholar]
- 7.Neumark-Sztainer D, van den Berg P, Hannan PJ et al. (2006) Self-weighing in adolescents: helpful or harmful? Longitudinal associations with body weight changes and disordered eating. J Adolesc Health 39, 811–818. [DOI] [PubMed] [Google Scholar]
- 8.Ogden J & Whyman C (1997) The effect of repeated weighing on psychological state. European Eating Disorders Review 5, 121–130. [Google Scholar]
- 9.Papalia Z, Wilson O, Bopp M et al. (2018) Technology-Based Physical Activity Self-Monitoring Among College Students. Int J Exerc Sci 11, 1096–1104. [PMC free article] [PubMed] [Google Scholar]
- 10.Sonneville KR & Lipson SK (2018) Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. Int J Eat Disord 51, 518–526. [DOI] [PubMed] [Google Scholar]
- 11.Lipson SK & Sonneville KR (2017) Eating disorder symptoms among undergraduate and graduate students at 12 U.S. colleges and universities. Eat Behav 24, 81–88. [DOI] [PubMed] [Google Scholar]
- 12.Tabler J & Utz RL (2015) The influence of adolescent eating disorders or disordered eating behaviors on socioeconomic achievement in early adulthood. Int J Eat Disord 48, 622–632. [DOI] [PubMed] [Google Scholar]
- 13.Filipova AA & Stoffel CL (2016) The prevalence of binge eating disorder and its relationship to work and classroom productivity and activity impairment. J Am Coll Health 64, 349–361. [DOI] [PubMed] [Google Scholar]
- 14.Rush CC, Curry JF Looney JG (2016) Alcohol expectancies and drinking behaviors among college students with disordered eating. J Am Coll Health 64, 195–204. [DOI] [PubMed] [Google Scholar]
- 15.Piran N & Robinson SR (2011) Patterns of associations between eating disordered behaviors and substance use in two non-clinical samples: a university and a community based sample. J Health Psychol 16, 1027–1037. [DOI] [PubMed] [Google Scholar]
- 16.Karkkainen U, Mustelin L, Raevuori A et al. (2018) Do Disordered Eating Behaviours Have Long-term Health-related Consequences? Eur Eat Disord Rev 26, 22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forney KJ, Buchman-Schmitt JM, Keel PK et al. (2016) The medical complications associated with purging. Int J Eat Disord 49, 249–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ginty AT, Phillips AC, Higgs S et al. (2012) Disordered eating behaviour is associated with blunted cortisol and cardiovascular reactions to acute psychological stress. Psychoneuroendocrinology 37, 715–724. [DOI] [PubMed] [Google Scholar]
- 19.Noel PH, Copeland LA, Pugh MJ et al. (2010) Obesity diagnosis and care practices in the Veterans Health Administration. J Gen Intern Med 25, 510–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noel PH, Wang CP, Bollinger MJ et al. (2012) Intensity and duration of obesity-related counseling: association with 5-Year BMI trends among obese primary care patients. Obesity (Silver Spring) 20, 773–782. [DOI] [PubMed] [Google Scholar]
- 21.Li W, Kelsey JL, Zhang Z et al. (2009) Small-area estimation and prioritizing communities for obesity control in Massachusetts. Am J Public Health 99, 511–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pacanowski CR, Linde JA Neumark-Sztainer D (2015) Self-Weighing: Helpful or Harmful for Psychological Well-Being? A Review of the Literature. Curr Obes Rep 4, 65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jensen MD, Ryan DH, Apovian CM et al. (2014) 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 129, S102–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pacanowski CR, Crosby RD Grilo CM (2019) Self-weighing behavior in individuals with binge-eating disorder. Eat Disord, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eisenberg ME & Neumark-Sztainer D (2010) Friends’ dieting and disordered eating behaviors among adolescents five years later: findings from Project EAT. J Adolesc Health 47, 67–73. [DOI] [PubMed] [Google Scholar]
- 26.Hazzard VM, Loth KA, Berge JM et al. (2020) Does exposure to controlling parental feeding practices during adolescence predict disordered eating behaviors 8 years later in emerging adulthood? Pediatr Obes 15, e12709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Simone M, Hooper L, Eisenberg ME et al. (2019) Unhealthy weight control behaviors and substance use among adolescent girls: The harms of weight stigma. Soc Sci Med 233, 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.(2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894, i-xii, 1–253. [PubMed] [Google Scholar]
- 29.Hahn SL, Bauer KW, Kaciroti N et al. (2021) Relationships between patterns of weight-related self-monitoring and eating disorder symptomology among undergraduate and graduate students. Int J Eat Disord. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lanza ST, Collins LM, Lemmon DR et al. (2007) PROC LCA: A SAS Procedure for Latent Class Analysis. Struct Equ Modeling 14, 671–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoerr SL, Bokram R, Lugo B et al. (2002) Risk for disordered eating relates to both gender and ethnicity for college students. J Am Coll Nutr 21, 307–314. [DOI] [PubMed] [Google Scholar]
- 32.Eisenberg D, Nicklett EJ, Roeder K et al. (2011) Eating disorder symptoms among college students: prevalence, persistence, correlates, and treatment-seeking. J Am Coll Health 59, 700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lavender JM, De Young KP Anderson DA (2010) Eating Disorder Examination Questionnaire (EDE-Q): norms for undergraduate men. Eat Behav 11, 119–121. [DOI] [PubMed] [Google Scholar]
- 34.Goodman A, Heshmati A Koupil I (2014) Family history of education predicts eating disorders across multiple generations among 2 million Swedish males and females. PLoS One 9, e106475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nagata JM, Ganson KT Murray SB (2020) Eating disorders in adolescent boys and young men: an update. Curr Opin Pediatr 32, 476–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leit RA, Pope HG Jr. Gray JJ (2001) Cultural expectations of muscularity in men: the evolution of playgirl centerfolds. Int J Eat Disord 29, 90–93. [DOI] [PubMed] [Google Scholar]
- 37.Pope HG Jr., Olivardia R, Gruber A et al. (1999) Evolving ideals of male body image as seen through action toys. Int J Eat Disord 26, 65–72. [DOI] [PubMed] [Google Scholar]
- 38.Strother E, Lemberg R, Stanford SC et al. (2012) Eating disorders in men: underdiagnosed, undertreated, and misunderstood. Eat Disord 20, 346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bemel JE, Brower C, Chischillie A et al. (2016) The Impact of College Student Financial Health on Other Dimensions of Health. Am J Health Promot 30, 224–230. [DOI] [PubMed] [Google Scholar]
- 40.Chen AC, Szalacha LA Menon U (2014) Perceived discrimination and its associations with mental health and substance use among Asian American and Pacific Islander undergraduate and graduate students. J Am Coll Health 62, 390–398. [DOI] [PubMed] [Google Scholar]
- 41.Giles SM, Champion H, Sutfin EL et al. (2009) Calorie restriction on drinking days: an examination of drinking consequences among college students. J Am Coll Health 57, 603–609. [DOI] [PMC free article] [PubMed] [Google Scholar]


