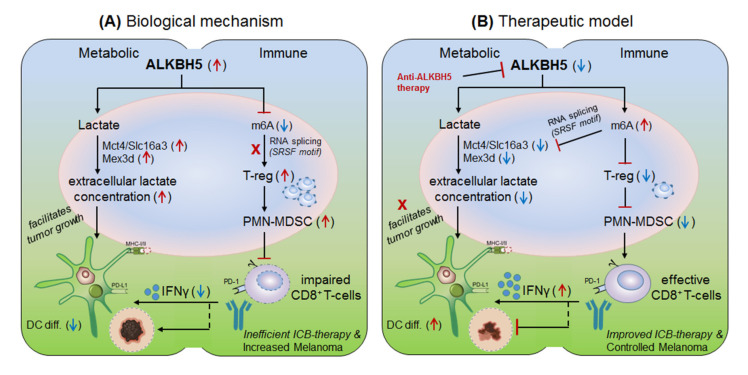
Figure 6.
Therapeutic model targeting intracellular checkpoint ‘ALKBH5’ in melanoma. (A) Biological mechanism: The ALKBH5 abnormally expressed in melanoma and colorectal cell carcinomas, and impairs the efficacy of anti-PD-1 therapy by (i) recruiting immunosuppressive; regulatory T-cell (T-reg) and polymorphonuclear myeloid derived suppressor cells (PMN-MDSC) abundances in the TME. (ii) by impairing DC-differentiation resulting in decreased CD8+T-cell effector functions. (iii) by increasing extracellular lactate availability to the tumors by up-regulating the expression of Mct4/Slc16a3 genes due to decreased m6A-methylation mark associated mechanism. (B) Therapeutic model: (i) Anti-ALKBH5 therapy: selective inhibition of ALKBH5 [168] by increasing m6A methylation-mediated inhibition of crucial genes essential to increase the efficacy of CD8+T-effector cells. (ii) T-reg/PMN-MDSCs depletion therapy: could also show the therapeutic propensity by rescuing the immunosuppressive environment. (iii) Increasing DC-differentiation: could be also a promising approach to enhance DC-mediated CD8+T-cell effector function. (iv) Targeting metabolic genes: could be an alternative approach to control melanoma tumorigenesis by limiting extracellular lactate accumulation in the TME. Collectively, all these approach seems promising in overcoming the issues associated with ICB drug-resistance.