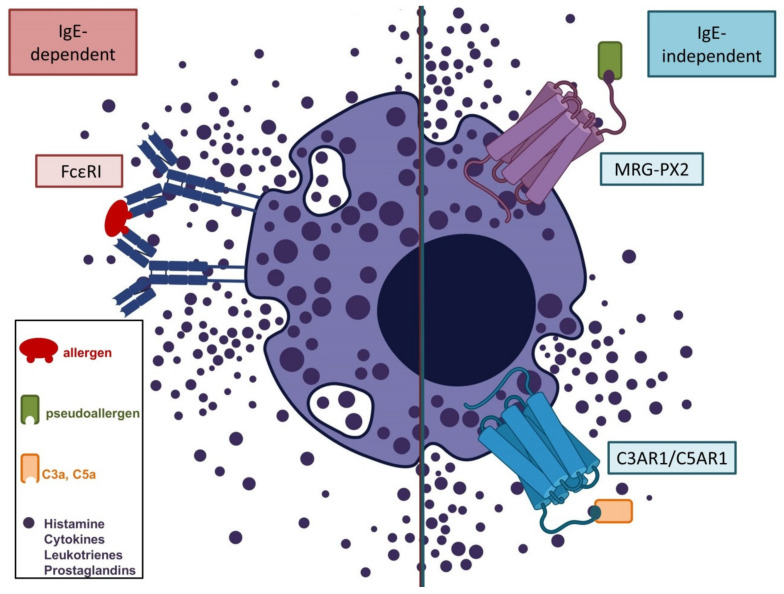
Figure 2.
Supposed mechanisms of IgE-dependent (type I allergic) and non-IgE-dependent (pseudoallergic) immediate reactions to COVID-19 vaccines adapted from [27,30,32]. Type I allergic reactions occur due to dimerization of high-affinity IgE receptors (FcεRI) in sensitized individuals after contact with an allergen (e.g., PEGs). Non-IgE-dependent immediate reactions may occur via direct interaction of pseudoallergens with G-protein-coupled receptors (e.g., MRG-PX2), or as a result of complement activation (C3a, C5a) in individuals with specific IgG against components of the vaccine (e.g., anti-PEG IgG). Synchronized mast cell degranulation is the result of all three pathways, and causes an abrupt increase in blood levels of histamine, leukotrienes, prostaglandins, and other cytokines. Clinical symptoms such as angioedema, bronchial obstruction, and decreased blood pressure (shock) occur according to the extent of the anaphylactic/anaphylactoid reaction, and may be life-threatening.