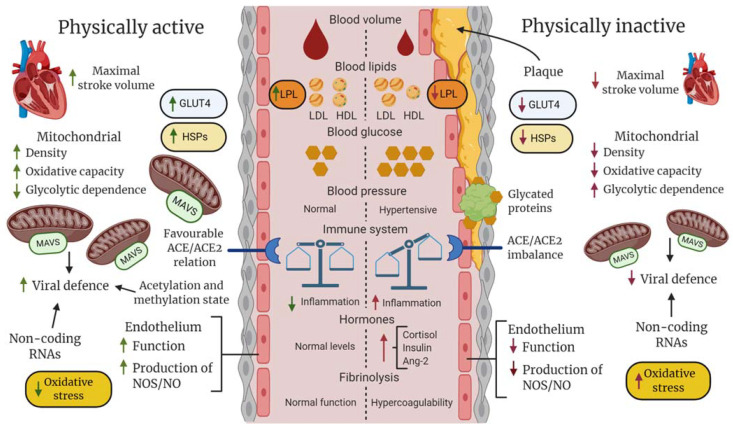
Figure 4.
Hypothetical description of differences between fit (physically active and non-obese) and unfit (physically inactive and obese) individuals in regard to general vascular, blood, and cellular components that could collectively determine clinical outcome following SARS-CoV-2 infection. At the systemic level, regular physical activity (PA), such as exercise training, promotes hormonal homeostasis and improves maximal stroke and blood volume, enhancing blood perfusion and oxygen saturation of tissues. In an unfit state with hypertension, an imbalance between the innate and adaptive immune systems, increased platelet aggregation, dyslipidemia, and abnormally high glucose levels increase the risk of lipid deposition, protein glycation and clot formation, inflammatory responses in the vascular wall, and atherosclerosis, which decrease blood perfusion and oxygen saturation, potentially leading to an infarct in the worst-case scenario. At the cellular level, the temporary metabolic and mechanical stress induced during PA results in improved stress-defense (e.g., heat shock proteins [HSPs], antioxidants), improved mitochondrial capacity in aerobic adenosine triphosphate production and antiviral response (mitochondrial antiviral signaling protein [MAVS]), enhanced uptake and utilization of glucose and fatty acids via increased expression of glucose transporter type 4 (GLUT-4) and lipoprotein lipase (LPL), and improved endothelial functions, including the balance between ACE/ACE2, nitric oxide (NO) production, and endothelin release. Regular PA may also produce a favorable balance between epigenetic factors that facilitate the expression of genes encoding proteins that enhance general cellular functions and activate proteins and non-coding genes that inhibit amplification of SARS-CoV-2.