Figure 2 |. Classifying drugs that potentially cause acute kidney injury.
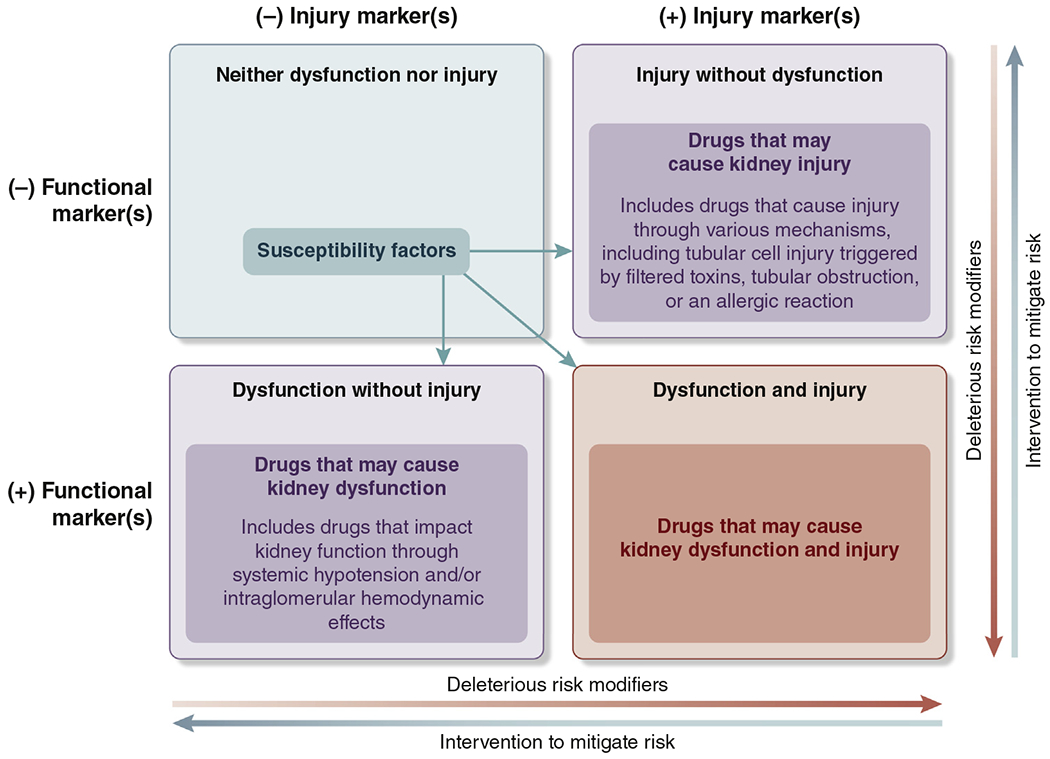
Iterative classification of agents that have potential to cause kidney dysfunction or kidney injury or both. Functional and injury biomarkers have a role in distinguishing among the different pathophysiological processes. Examples of deleterious risk modifiers are duration of therapy, drug burden, hypotension, and pharmacokinetic/pharmacodynamic interactions. Examples of interventions to mitigate risk are daily dynamic prescribing, kidney monitoring, and patient and provider education. Susceptibility factors include those listed in the 2012 Kidney Disease: Improving Global Outcomes Acute Kidney Injury guideline: dehydration or volume depletion; advanced age; female gender; black race; chronic kidney disease; chronic diseases of the heart, lung, or liver; diabetes mellitus; cancer; and anemia.1 Any final impact depends on underlying susceptibility, associated risk factors, clinical context, drug management, and modifying factors. Examples of drugs that correspond to the relevant categories above include trimethoprim, cimetidine (neither dysfunction nor injury); angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers (dysfunction without injury); aminoglycoside, acyclovir, vascular endothelial growth factor antagonists (injury without dysfunction); and nonsteroidal anti-inflammatory drugs (dysfunction and injury).
