Abstract
Background
The Centers for Medicare & Medicaid Services (CMS) use hospital readmissions as a performance metric to incentivize hospital care for acute conditions including pneumonia. However, there are limitations to using readmission alone as a hospital performance metric.
Objective
To characterize 30-day risk-standardized home time (RSHT), a novel patient-centered post-discharge performance metric for acute pneumonia hospitalizations in Medicare patients, and compare hospital rankings based on this metric with mortality and readmissions.
Study Design
Retrospective, cohort study.
Participants
A cohort of Medicare fee-for-service beneficiaries admitted between January 01, 2015 and November 30, 2017.
Interventions
None.
Main Measures
Risk-standardized hospital-level home time within 30 days of discharge was evaluated as a novel performance metric. Multilevel regression models were used to calculate hospital-level estimates and rank hospitals based on RSHT, readmission rate (RSRR), and mortality rate (RSMR).
Key Results
A total of 1.7 million pneumonia admissions admitted to one of the 3116 hospitals were eligible for inclusion. The median 30-day RSHT was 20.5 days (interquartile range: 18.9–21.9 days; range: 5–29 days). Hospital-level characteristics such as case volume, bed size, for-profit ownership, rural location of the hospital, teaching status, and participation in the bundled payment program were significantly associated with home time. We found a modest, inverse correlation of RSHT with RSRR (rho: −0.233, p< 0.0001) and RSMR (rho: −0.223, p< 0.0001) for pneumonia. About 1/3rd of hospitals were reclassified as high performers based on their RSHT metric compared with the rank on their RSRR and RSMR metrics.
Conclusion
Home time is a novel, patient-centered, hospital-level metric that can be easily calculated using claims data and accounts for mortality, readmission to an acute care facility, and admission to a skilled nursing facility or long-term care facility after discharge. Utilization of this patient-centered metric could have policy implications in assessing hospital performance on delivery of healthcare to pneumonia patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06712-w.
KEY WORDS: home time, pneumonia, CMS, metrics
INTRODUCTION
Pneumonia is a leading infectious cause of hospitalization and death among adults in the USA.1, 2 The risk of acquiring pneumonia increases with age, and adults ≥ 65 years are 3–7 times more likely to be hospitalized with pneumonia compared with younger adults.3 A systematic review reported that at least one in six patients hospitalized for pneumonia are readmitted within 30 days with the median all-cause readmission rate as high as 17.3%.4
Readmissions are common and costly especially if they are a result of poor quality of care during the index admission.5 Starting in 2012, the Hospital Readmissions Reduction Program (HRRP) was implemented by the Centers for Medicare & Medicaid Services (CMS) that financially penalizes hospitals with 30-day readmission rates that are higher than expected for health conditions such as heart failure (HF), acute myocardial infarction (AMI), and pneumonia, among Medicare fee-for-service (FFS) beneficiaries.6, 7 In response to the HRRP policy, hospitals have invested in several interventions such as patient self-management strategies, monitoring patients closely, and ensuring timely follow-up to reduce readmission rates during the first 30 days.8, 9 While these efforts have reduced hospital readmissions overall,8 concerns exist about aggressive readmission reduction policies that may lower readmissions at the expense of patient survival after discharge.10 Early discharge from acute care settings, driven in part by hospitals’ efforts to reduce patient length of stay and readmissions, may result in increased use of post-acute care (PAC) services.11 Current CMS performance metrics do not reflect the trade-offs between readmissions, mortality, and the use of PAC settings.
Several studies have assessed home time as a patient-centered quality metric, which can be calculated using readily available administrative claims data.12–15 These studies have shown increased home time to be associated with improved clinical and patient-reported outcomes while being an easily interpretable measure for patients and providers. Home time may be especially relevant for pneumonia given the potential for higher use of PAC facilities after discharge from an acute pneumonia admission. Our objective was to assess home time within 30 days after discharge among pneumonia hospitalizations, where home time reflects days alive after discharge and not spent in acute or PAC settings. The association of this metric with CMS performance metrics 30-day risk-standardized readmission rate (RSRR) and 30-day risk-standardized mortality rate (RSMR) was also evaluated.
METHODS
Study Population and Design
The institutional review board (IRB) at the University of Iowa approved and waived informed consent for this study due to the large number of patients and lack of patient contact information. This study used the CMS Medicare Provider Analysis and Review (MedPAR) data which includes administrative billing claims for all acute care hospitalizations and rehabilitation or skilled nursing facility (SNF) stays of Medicare beneficiaries.
Inclusion and Exclusion Criteria
The cohort was identified using the 2016 CMS pneumonia criteria.16 Medicare FFS beneficiaries admitted with a diagnosis of pneumonia at a short-term acute care hospital between January 01, 2015 and November 30, 2017 comprised the target population (n=2,508,587). Patients ≥ 65 years of age hospitalized with a primary diagnosis of pneumonia or, a primary diagnosis of sepsis with a secondary diagnosis of pneumonia were included in the cohort (e Table 1). Only the first hospitalization was included in patients with multiple pneumonia admissions within a 30-day period. Hospitals were excluded if they had ≤ 25 pneumonia admissions during the 3-year study period. The final analytical cohort included 1,662,980 patients from 3116 hospitals (Fig. 1).
Figure 1.
Flow chart of development of the analysis cohort from raw dataset.
Study Measures
Hospital characteristics were assessed from the 2016 American Hospital Association Survey. Hospitals were classified as teaching or non-teaching, for-profit or not-for-profit, private or public, and rural or urban. Patient-level data included information on age, race, comorbidities, and discharge disposition assigned during the hospital stay. Comorbidities were defined by secondary diagnoses using previously established algorithms based on International Classification of Diseases codes.17
Time spent at home by each patient within 30 days of hospital discharge was the primary outcome, defined as the number of days spent alive and out of an acute care inpatient setting, SNF, or a long-term care facility. If a patient spent any part of a day in a care facility, then that day did not contribute toward home time. If a patient died, then only the days prior to death that were not spent in a facility contributed to home time. Patients who remained alive at home after discharge without readmission to an acute care hospital, SNF, or rehabilitation facility were assessed as contributing a home time of 30 days. RSRR within 30 days after discharge and RSMR within 30 days from index admission were also estimated. Consistent with CMS methodology, patients who were transferred from one acute care hospital to another were assigned to the transferring acute care hospital for RSMR estimation, and assigned to the discharging acute care hospital for the RSRR or RSHT estimation.
Statistical Analyses
Maximum likelihood estimates generated from generalized linear mixed models with log link and Poisson distribution were used to calculate RSHT, while separate hierarchical logistic regression models were used to calculate RSRR and RSMR estimates, per published methodology.18, 19 Patients who had an in-hospital death were retained in the model to estimate RSMR but excluded from models to generate estimates for RSHT and RSRR.
The statistical analyses were consistent with the CMS risk-standardization methodology. The risk adjustment models included candidate comorbidity variables which the CMS selected and categorized based on clinician review to develop a clinically meaningful yet parsimonious set of comorbid risk variables (e Tables 2, 3, and 4). Consistent with the CMS approach, race and socioeconomic status were not included in risk adjustment. For variable selection, 25% of patients from each year were randomly selected and pooled to construct model development and validation cohorts. Next, 100 bootstrapped samples were generated from the development cohort and separate models were run for each sample replicate including all variables suggested by the CMS for each performance metric as candidate variables, selected using a stepwise selection approach. For each metric, variables that were selected in more than 80% of the initial 100 bootstrap models were used as final risk adjustment variables. Hospital identifiers were included as random effects to account for clustering of admissions within hospitals.20, 21
To estimate hospital-level RSHT, RSRR, and RSMR, we used the final multivariable hierarchical models to calculate predicted and expected rates for each estimate. The overall unadjusted grand mean for home time, readmission, and mortality were multiplied by the hospital-specific predicted to expected ratio to calculate the hospital-level risk-standardized rate estimates for home time (RSHT), readmission (RSRR), and mortality (RSMR), respectively.
Baseline patient- and hospital-level characteristics were reported for each quartile of the RSHT. These characteristics were compared across quartiles using ANOVA for continuous variables and chi-square for categorical variables. Median and interquartile range (IQR) or mean and standard deviation (SD) were reported for continuous variables while frequency and percentage were reported for categorical variables. Correlation between the risk-standardized estimates was calculated using the Pearson’s coefficient test.
Hospitals were ranked as low or high performing based on their quartile for each risk-standardized estimate. Quartiles (Q1 to Q4: low to high performance for RSHT and high to low performance for RSRR and RSMR) were created for RSHT, RSRR, and RSMR. A hospital was assigned a positive score (+1 to +3) if they were in a higher performance group for RSHT compared with RSRR or RSMR, and a negative score (−1 to −3) if they were in a lower performance group for RSHT compared with RSRR or RSMR. Hospitals that ranked in the same performance group on both metrics were assigned a score of 0. A positive reclassification score of 2 or higher was considered as meaningful up-classification in performance status and a negative reclassification score of 2 or lower was considered as meaningful down-classification.
Sensitivity analysis was conducted to assess correlation of RSHT with RSMR in a subset of patients who were discharged alive. A second sensitivity analysis was conducted to evaluate the association of RSHT with RSRR and RSMR in a subset of patients with a primary diagnosis of pneumonia to explore if correlation between metrics in a cohort of relatively less sick patients was similar to the overall cohort. Patients with sepsis as the primary diagnosis were excluded for this second analysis. All analyses were conducted using the SAS software version 9.4 and p-value < 0.05 was considered significant.
RESULTS
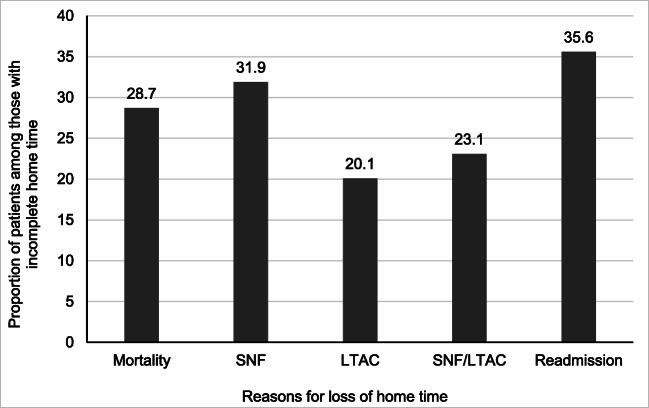
About 1.7 million pneumonia admissions for patients 65 years of age and above admitted to one of the 3116 hospitals between January 01, 2015 and November 30, 2017 were included in the study (Fig. 1). The majority (68.1%) had a primary diagnosis of pneumonia at admission, while the remaining (31.9%) were assigned a primary diagnosis of sepsis and a secondary diagnosis of pneumonia. More than half of the study patients (n=943,110, 56.7%) were alive and stayed home for all 30 days. Among 719,870 patients with home time < 30 days, mortality (206,838, 28.7%), only SNF stays (229,385, 31.9%), only long-term acute care (LTAC) stays (144,937, 20.1%), SNF or LTAC stays (165,882, 23.1%), and readmission to an acute care facility (256,145, 35.6%) were observed reasons for incomplete home time (Fig. 2). Death accounted for a mean loss of home time of 2.2 days (SD=7.6), while SNF, LTAC, and acute care readmissions accounted for mean home time loss of 5.1 days (SD=10.1), 2.8 days (SD=6.8), and 0.9 days (SD=2.9), respectively. A comparison between patients with complete home time and those that lost home time is provided in e Table 5.
Figure 2.
Distribution for outcomes in patients who lost home time (n=719,870).
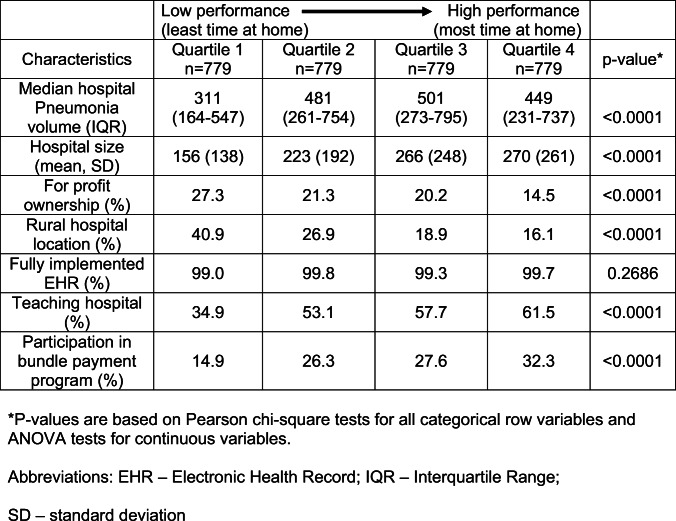
In Table 1, patients admitted to the lowest performance quartile of RSHT were older, white, and had higher likelihood of having a secondary diagnosis of AMI, HF, or chronic obstructive pulmonary disease compared with patients in the highest performance quartile of RSHT. The proportion of admissions discharged to home was significantly lower (34.0% vs. 45.5%) while the proportion of patients discharged to a SNF or a LTAC facility were higher (36.0% vs. 22.6%) in the lowest quartile of RSHT compared with the highest quartile of RSHT. Table 2 shows that hospitals in the lowest RSHT quartile admitted 31% fewer median pneumonia cases and were smaller sized hospitals, two times more likely to be for-profit ownership, almost three times more likely to be rural, 40% less likely to be teaching hospitals, and 46% less likely to participate in the bundled payment program, compared with hospitals in the highest RSHT quartile.
Table 1.
Patient-Level Characteristics Across Quartiles of 30-Day Risk-Standardized Home Time
Table 2.
Hospital-Level Characteristics Across Quartiles of 30-Day Risk-Standardized Home Time
There is substantial variability in hospital-level 30-day RSHT shown in Figure 3. The median 30-day RSHT was 20.5 days (IQR: 18.9–21.9 days; range: 5–29 days). The proportion of hospitals with perfect home time of 30 days was 26% higher in the highest quartile compared with the lowest RSHT quartile (64.2% vs. 47.5%). Patients from low-performance hospitals spent on average an additional 3.8 days in a SNF (mean: 7.1 days vs. 3.3 days) and 1.3 days (mean: 3.5 days vs. 2.2 days) in a LTAC facility after discharge compared with patients discharged from high-performance hospitals. One additional day was lost to death or acute care readmission during the follow-up period in the lowest compared with the highest RSHT quartiles.
Figure 3.

Vertical box plots of 30-day risk-standardized estimates for a cohort of Medicare fee-for-service beneficiaries discharged after hospitalization for pneumonia. Upper panel shows risk-standardized home time. Middle panel shows risk-standardized mortality rate. Lower panel shows risk-standardized readmission rate. X-axis labels: Q1, low-performance hospitals (least time at home); Q4, high-performance hospitals (most time at home). Dashed line, median value; diamond symbol, mean value; bottom edge of box, 25th percentile; top edge of box, 75th percentile; whiskers, range of values beyond 25th and 75th percentiles.
The median RSRR was 16.8% (IQR: 15.7–18.2%) and the median RSMR was 10.7% (IQR: 9.3–12.5%). A modest statistically significant inverse correlation was observed between RSHT and RSRR (rho: −0.23, p<0.0001), and RSMR (rho: −0.22, p<0.0001), respectively (e Figure 1). These correlations suggest that longer home time was associated with lower rates of readmission and mortality. The strength and direction of these correlations were consistent in a subset that excluded all in-hospital deaths (RSMR rho: −0.422) or included only patients with a primary diagnosis of pneumonia (RSRR rho: −0.193, RSMR rho: −0.187).
A 5.8% relative difference (1% absolute difference) was observed between estimated RSRR among hospitals in the lowest and highest RSHT quartiles (Q1: 17.2%, Q2: 17.1%, Q3: 16.9%, Q4: 16.2%). A larger magnitude of relative difference (19.1%) and absolute difference (2.3%) was noted for RSMR between RSHT quartiles (Q1: 12.1%, Q2: 10.8%, Q3: 10.3%, Q4: 9.8%). Almost two-thirds of the 3116 hospitals (n=2178) had a meaningful reclassification in their performance status based on RSHT compared with RSRR, 35.5% were up-classified and 34.4% were down-classified. Similarly, close to two-third (n=2044) hospitals were meaningfully reclassified based on RSHT compared with RSMR (up-classified: 32.0%, down-classified: 33.6%).
DISCUSSION
In this retrospective cohort study of 3116 hospitals, results on the 30-day RSHT suggest that this metric may be complementary to RSRR and RSMR in ranking hospitals based on patient outcomes. Substantial variation was observed between hospitals in the low- and high-performance quartiles for RSHT, even after adjusting for differences in patient risk factors. Admission to a SNF or LTAC facility (75%), death within 30 days from admission (29%), and readmission to an acute care facility (39%) were observed among patients who had incomplete home time.
Low-performance hospitals had a higher prevalence of older, white patients with comorbidities than hospitals with high performance on RSHT. Hospitals with the lowest home time patients were smaller hospitals, were located in rural areas, were non-teaching hospitals, had lower pneumonia case volume, and did not participate in the bundled payment program compared with hospitals that kept patients home longer after discharge. There was a modest, inverse correlation between hospital-level RSHT and RSRR or RSMR. About 36% and 32% of hospitals were reclassified as good performance hospitals based on their RSHT metric compared to their performance on the RSRR and RSMR metrics, respectively.
Prior studies have examined home time for acute conditions such as stroke, AMI, and HF.14, 19, 22 A study conducted in community-dwelling Medicare beneficiaries observed an association between estimated home time and patient-reported quality of life outcomes such as mobility impairment and difficulty in self-care.14 Home time has also been extensively studied in stroke patients where studies observed an association of this metric with clinical outcomes such as global disability, stroke risk scores, and functional status.23–25 Similarly, our findings are consistent with recent studies from our group which found hospital-level risk-standardized home time to be associated with hospital rates of post-discharge readmission and mortality for AMI and HF.19, 26 The strength of the home time metric is that it not only captures the risk of mortality but also considers readmissions, length of stay during readmission, and need for extended care in SNF or LTAC facilities. Overall, this novel metric accounts for the mortality and morbidity burden in a health system by considering all the above-mentioned patient-centered factors.
Post-discharge stays at LTAC facilities and SNF were the main contributors to loss of home time over 30-day follow-up. A study conducted to assess utilization of PAC services before and after implementation of the HRRP noted a small but significant increase in the use of skilled nursing care among patients with pneumonia.27 This loss of home time to PAC settings is an expected finding given the requirement for continued intravenous antibiotics and respiratory therapy in clinically stable pneumonia patients and higher likelihood of SNF admissions for continued care in complex cases such as patients with a diagnosis of sepsis with pneumonia.28, 29 Variation in the quality of care across PAC facilities could potentially impact patient’s long-term outcomes.30 Utilization of home time metric may lead to detailed assessment on use of PAC facilities and encourage discharging providers and hospitals to consider judicious use of services.
Existing CMS metrics such as RSRR and Excess Days of Acute Care capture all acute care stays in the 30-day post-discharge period. However, these metrics do not account for the post-discharge mortality or SNF/LTAC stays. Hospitals with high mortality rates could misleadingly appear to have low readmission rates and vice versa. Similarly, hospitals that are high utilizers of PAC facilities may appear to have low readmission rates but also accrue high medical costs in this process. These factors potentially result in inappropriate hospital performance rankings based on readmission rates alone and could influence financial penalties applied to the hospital. As a metric, the RSHT not only accounts for the competing risk from mortality but also considers only the time spent out of a care facility after discharge. The relatively modest correlations between RSHT and RSRR or RSMR reinforce the potential for home time as a complementary metric to assess hospital performance on patient outcomes. Consideration of our findings could have important policy implications in hospital reimbursement for pneumonia admissions.
This study has several important limitations. First, the quality of home time, use of home health care services, or symptom severity could not be determined using the administrative claims dataset.31 We also did not assess the reason for use of PAC facilities within 30 days after discharge which could be influenced by patient and caregiver decisions based on costs of care.32 Home time in the context of this study could also mean difficulty in access to medical care due to socioeconomic barriers or inclination to enroll in hospice care. However, time spent at home is generally known to provide more psychological comfort and better quality of life than the time at a care facility.33, 34 Second, the RSHT was based on administrative claims data and could be biased due to temporal changes in coding practices. Third, our study findings may not be generalizable to younger patients or those with other forms of insurance as our analysis was limited to Medicare FFS beneficiaries. Fourth, we did not include emergency department (ED) visits in the calculation of home time metrics.35 ED visits are typically ≤ 2 days so we do not anticipate a significant difference in performance of hospitals based on the inclusion of these visits. Finally, risk adjustment variables were derived only from inpatient administrative claims data and do not incorporate outpatient clinical data. Nevertheless, inpatient claims data can include up to 26 possible patient problems which should capture the patient’s clinical comorbidities.
In summary, 30-day home time is a novel, post-discharge, patient-centric, hospital-level performance metric that can be calculated with data that is readily available in the CMS administrative claims dataset, accounts for differences in post-discharge mortality and use of healthcare facilities, and can be intuitively interpreted. Utilization of this novel metric in conjunction with other existing metrics could have policy implications in delivery of healthcare to pneumonia patients.
Supplementary Information
(PDF 592 kb)
Author Contribution
A.P. and M.V-S. designed and directed the project, Y.G. and R.N. analyzed the data and summarized results, and R.N. took the lead in writing the manuscript. All authors provided critical feedback and helped shape the research, analysis, and manuscript.
Funding
Dr Pandey is supported by the Texas Health Resources Clinical Scholarship , the Gilead Sciences Research Scholar Program, the National Institute of Aging GEMSSTAR Grant (1R03AG067960-01), and Applied Therapeutics. Dr Girotra reports receiving grants from the Department of Veterans Affairs Health Services Research and Development Service during the conduct of the study. Dr Vaughan-Sarrazin was supported by award R01-AG055663 from the National Institutes of Health and by the Health Services Research and Development Service of the US Department of Veterans Affairs.
Data Availability
The data that support the findings of this study are available from the Centers for Medicare & Medicaid Services (CMS) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Centers for Medicare & Medicaid Services (CMS).
Declarations
Conflict of Interest
Dr Girotra reports receiving grants from the Department of Veterans Affairs Health Services Research and Development Service during the conduct of the study. Dr Vaughan-Sarrazin was supported by award R01-AG055663 from the National Institutes of Health and by the Health Services Research and Development Service of the US Department of Veterans Affairs. Dr Pandey served on the advisory board of Roche Diagnostics. The other authors report no conflicts.
Footnotes
Prior Presentations
Interim results from this study were presented at the IDWeekTM, Virtual Conference, October 21-25, 2020 and the Annual Research Day, Department of Internal Medicine, Virtual Conference, October 20-21, 2020. Interim results from this study were presented at the Society for Healthcare Epidemiology of America (SHEA) Spring meeting, St. Louis, MO, March 29-30, 2017.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA. 2005;294(21):2712–9. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- 2.Thomas CP, Ryan M, Chapman JD, Stason WB, Tompkins CP, Suaya JA, et al. Incidence and cost of pneumonia in medicare beneficiaries. Chest. 2012;142(4):973–81. doi: 10.1378/chest.11-1160. [DOI] [PubMed] [Google Scholar]
- 3.Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N Engl J Med. 2015;373(5):415–27. doi: 10.1056/NEJMoa1500245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinreich M, Nguyen OK, Wang D, Mayo H, Mortensen EM, Halm EA, et al. Predicting the Risk of Readmission in Pneumonia. A Systematic Review of Model Performance. Ann Am Thorac Soc. 2016;13(9):1607–14. doi: 10.1513/AnnalsATS.201602-135SR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med. 2010;170(4):340–6. doi: 10.1001/archinternmed.2009.511. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare and Medicaid Services. Readmissions Reduction Program. [cited 2020 May 12]. Available from: www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 7.Henry J. Kaiser Family Foundation. Aiming for fewer hospital U-turns. [cited 2020 May 12]. Available from: www.kff.org/report-section/aiming-for-fewer-hospital-uturns-issue-brief/.
- 8.Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nuckols TK, Keeler E, Morton S, Anderson L, Doyle BJ, Pevnick J, et al. Economic Evaluation of Quality Improvement Interventions Designed to Prevent Hospital Readmission: A Systematic Review and Meta-analysis. JAMA Intern Med. 2017;177(7):975–85. doi: 10.1001/jamainternmed.2017.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta A, Fonarow GC. The Hospital Readmissions Reduction Program: Evidence for Harm. JACC Heart Fail. 2018;6(7):607–9. doi: 10.1016/j.jchf.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Patient and Hospitalization Characteristics Associated With Increased Postacute Care Facility Discharges From US Hospitals. Med Care. 2015;53(6):492–500. doi: 10.1097/MLR.0000000000000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dewilde S, Annemans L, Peeters A, Hemelsoet D, Vandermeeren Y, Desfontaines P, et al. The relationship between Home-time, quality of life and costs after ischemic stroke: the impact of the need for mobility aids, home and car modifications on Home-time. Disabil Rehabil. 2020;42(3):419–25. doi: 10.1080/09638288.2018.1501438. [DOI] [PubMed] [Google Scholar]
- 13.Greene SJ, O’Brien EC, Mentz RJ, Luo N, Hardy NC, Laskey WK, et al. Home-Time After Discharge Among Patients Hospitalized With Heart Failure. J Am Coll Cardiol. 2018;71(23):2643–52. doi: 10.1016/j.jacc.2018.03.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee H, Shi SM, Kim DH. Home Time as a Patient-Centered Outcome in Administrative Claims Data. J Am Geriatr Soc. 2019;67(2):347–51. doi: 10.1111/jgs.15705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Brien EC, Xian Y, Xu H, Wu J, Saver JL, Smith EE, et al. Hospital Variation in Home-Time After Acute Ischemic Stroke: Insights From the PROSPER Study (Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research) Stroke. 2016;47(10):2627–33. doi: 10.1161/STROKEAHA.116.013563. [DOI] [PubMed] [Google Scholar]
- 16.(CMS) CfMMS. 2016 Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Readmission Measures 2016 [cited 2020 December 3]. Available from: http://aann.org/uploads/Condition_Specific_Readmission_Measures.pdf.
- 17.Elixhauser A. Clinical Classifications Software (CCS) 2009. http://wwwhcug-usahrqgov/toolssoft-ware/ccs/ccsjsp. 2009.
- 18.Centers for Medicare & Medicaid Services (CMS) 2013 Measures Updates and Specifications: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measure (Version 7.0) [cited 2020 May 13]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Mortality_AMI-HF-PN_Measures_Updates_Report_FINAL_06-13-2013.pdf.
- 19.Pandey A, Keshvani N, Vaughan-Sarrazin MS, Gao Y, Girotra S. Evaluation of Risk-Adjusted Home Time After Acute Myocardial Infarction as a Novel Hospital-Level Performance Metric for Medicare Beneficiaries. Circulation. 2020;142(1):29–39. doi: 10.1161/CIRCULATIONAHA.119.044765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keenan PS, Normand SL, Lin Z, Drye EE, Bhat KR, Ross JS, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1(1):29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 21.Krumholz HM, Wang Y, Mattera JA, Wang Y, Han LF, Ingber MJ, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113(13):1683–92. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 22.McDermid I, Barber M, Dennis M, Langhorne P, Macleod MJ, McAlpine CH, et al. Home-Time Is a Feasible and Valid Stroke Outcome Measure in National Datasets. Stroke. 2019;50(5):1282–5. doi: 10.1161/STROKEAHA.118.023916. [DOI] [PubMed] [Google Scholar]
- 23.Fonarow GC, Liang L, Thomas L, Xian Y, Saver JL, Smith EE, et al. Assessment of Home-Time After Acute Ischemic Stroke in Medicare Beneficiaries. Stroke. 2016;47(3):836–42. doi: 10.1161/STROKEAHA.115.011599. [DOI] [PubMed] [Google Scholar]
- 24.Mishra NK, Shuaib A, Lyden P, Diener HC, Grotta J, Davis S, et al. Home time is extended in patients with ischemic stroke who receive thrombolytic therapy: a validation study of home time as an outcome measure. Stroke. 2011;42(4):1046–50. doi: 10.1161/STROKEAHA.110.601302. [DOI] [PubMed] [Google Scholar]
- 25.Yu AYX, Rogers E, Wang M, Sajobi TT, Coutts SB, Menon BK, et al. Population-based study of home-time by stroke type and correlation with modified Rankin score. Neurology. 2017;89(19):1970–6. doi: 10.1212/WNL.0000000000004631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pandey A, Keshvani N, Vaughan-Sarrazin MS, Gao Y, Fonarow GC, Yancy C, et al. Evaluation of Risk-Adjusted Home Time After Hospitalization for Heart Failure as a Potential Hospital Performance Metric. JAMA Cardiol. 2021;6(2):169-176 [DOI] [PMC free article] [PubMed]
- 27.Popescu I, Sood N, Joshi S, Huckfeldt P, Escarce J, Nuckols TK. Trends in the Use of Skilled Nursing Facility and Home Health Care Under the Hospital Readmissions Reduction Program: An Interrupted Time-series Analysis. Med Care. 2019;57(10):757–65. doi: 10.1097/MLR.0000000000001184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Rise of post-acute care facilities as a discharge destination of US hospitalizations. JAMA Intern Med. 2015;175(2):295–6. doi: 10.1001/jamainternmed.2014.6383. [DOI] [PubMed] [Google Scholar]
- 29.Jones TK, Fuchs BD, Small DS, Halpern SD, Hanish A, Umscheid CA, et al. Post-Acute Care Use and Hospital Readmission after Sepsis. Ann Am Thorac Soc. 2015;12(6):904–13. doi: 10.1513/AnnalsATS.201411-504OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood). 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dong T, Cursio JF, Qadir S, Lindenauer PK, Ruhnke GW. Discharge disposition as an independent predictor of readmission among patients hospitalised for community-acquired pneumonia. Int J Clin Pract. 2017;71(3-4). [DOI] [PubMed]
- 32.Ayele R, Jones J, Ladebue A, Lawrence E, Valverde P, Leonard C, et al. Perceived Costs of Care Influence Post-Acute Care Choices by Clinicians, Patients, and Caregivers. J Am Geriatr Soc. 2019;67(4):703–10. doi: 10.1111/jgs.15768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fowler E, MacRae S, Stern A, Harrison T, Gerteis M, Walker J, et al. The built environment as a component of quality care: understanding and including the patient’s perspective. Jt Comm J Qual Improv. 1999;25(7):352–62. doi: 10.1016/s1070-3241(16)30450-3. [DOI] [PubMed] [Google Scholar]
- 34.Hack TF, McClement SE, Chochinov HM, Dufault B, Johnston W, Enns MW, et al. Assessing Symptoms, Concerns, and Quality of Life in Noncancer Patients at End of Life: How Concordant Are Patients and Family Proxy Members? J Pain Symptom Manage. 2018;56(5):760–6. doi: 10.1016/j.jpainsymman.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 35.Vashi AA, Fox JP, Carr BG, D’Onofrio G, Pines JM, Ross JS, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364–71. doi: 10.1001/jama.2012.216219. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 592 kb)
Data Availability Statement
The data that support the findings of this study are available from the Centers for Medicare & Medicaid Services (CMS) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Centers for Medicare & Medicaid Services (CMS).