To the Editor:
Venovenous extracorporeal membrane oxygenation (VV-ECMO) has been used as a rescue therapy for patients with refractory coronavirus disease (COVID-19)–associated severe acute respiratory distress syndrome (ARDS) with survival rates similar to those reported for ECMO support of ARDS of other causes (1, 2). However, the need for prolonged ventilation, sedation, and immobility may limit long-term benefits of ECMO in these patients. Specifically, they are exposed to a high risk of ventilator-associated pneumonia (3). According to a recent case series, single-access, dual-stage VV-ECMO with extubation on ECMO (median time to extubation: 13 d) appeared to be safe and associated with a favorable prognosis for patients with severe COVID-19–associated ARDS (4). VV-ECMO has anecdotally been applied as an alternative to invasive mechanical ventilation (MV) in awake, spontaneously breathing patients with ARDS caused by Pneumocystis pneumonia (5) or immunocompromised status (6).
We report herein a patient with COVID-19, with severe ARDS not responding to high-flow nasal oxygen and noninvasive ventilation (NIV), who was successfully treated with prolonged “awake ECMO,” thereby avoiding endotracheal intubation and MV. On November 5, 2020, a 57-year-old man (body mass index, 29 kg/m2) was admitted to our department 3 days after COVID-19 symptom onset. His oxygen saturation was 40% on room air and increased to 90% with 15 L/min of oxygen via a facemask. Real-time RT-PCR of his nasopharyngeal swab was positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Figure 1). His medical history was marked by chronic hypertension and coronary artery bypass surgery with preserved left ventricular function 26 days before admission. He had been discharged from the hospital 12 days after cardiac surgery. At ICU admission, he had signs of acute respiratory failure. Initial therapy consisted of high-flow nasal oxygen (50 L/min; FiO2, 100%) and dexamethasone (7). He did not require inotropes or vasopressors. On Day 5, he became tachypneic (respiratory rate > 35/min) and required continuous NIV for adequate oxygenation (V̇e, 28 L/min; positive end-expiratory pressure, 6 cm H2O; FiO2, 100%). Blood gas values were as follows: PaO2/FiO2, 55 mm Hg; PaCO2, 32 mm Hg; and lactate, 2.3 mmol/L. Surprisingly, he did not complain of intense dyspnea.
Figure 1.
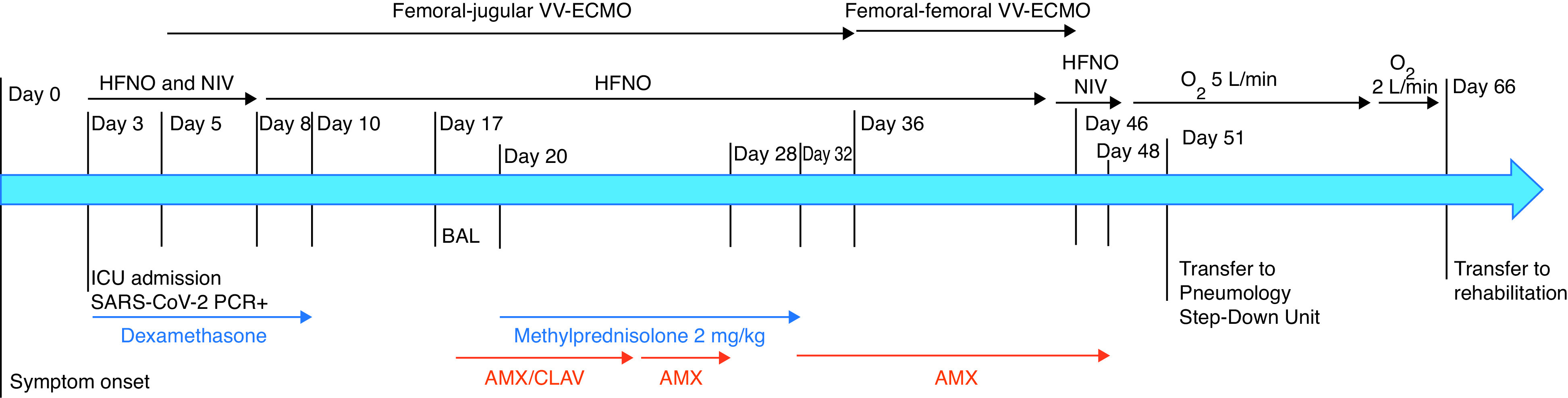
Patient timeline. AMX = amoxicillin; AMX/CLAV = amoxicillin/clavulanic acid; HFNO = high-flow nasal oxygen; NIV = noninvasive ventilation; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; VV-ECMO = venovenous extracorporeal membrane oxygenation.
Chest X-ray showed extensive bilateral pulmonary infiltrates (Figure 2). Intubation was discussed with the patient, who adamantly refused because of bad memories of it after heart surgery. Then awake VV-ECMO was proposed and he agreed. A 29F drainage cannula was inserted through the left femoral vein and a 21F return cannula into the right internal jugular vein under NIV, local anesthesia, and low-dose analgesia and sedation including 10 mg ketamine, 5 mg midazolam, and 10 mg morphine. During the 41 days of ECMO support, femoral–jugular ECMO blood flow ranged from 3.5 to 5.7 L/min and sweep gas flow from 2 to 6 L/min, with membrane O2 fraction set at 100%. The patient was comfortable with less tachypnea. He did not complain of dyspnea and, after Day 8, no longer required NIV. High-flow nasal oxygen (30–40 L/min) was maintained throughout the ECMO run to improve lung volume and lower hypoxic central drive (8). Chest computed tomography on Day 20 showed extensive bilateral parenchymatous condensations with traction bronchiectasis and no residual pulmonary embolism. Consequently, high-dose corticosteroids were initiated.
Figure 2.
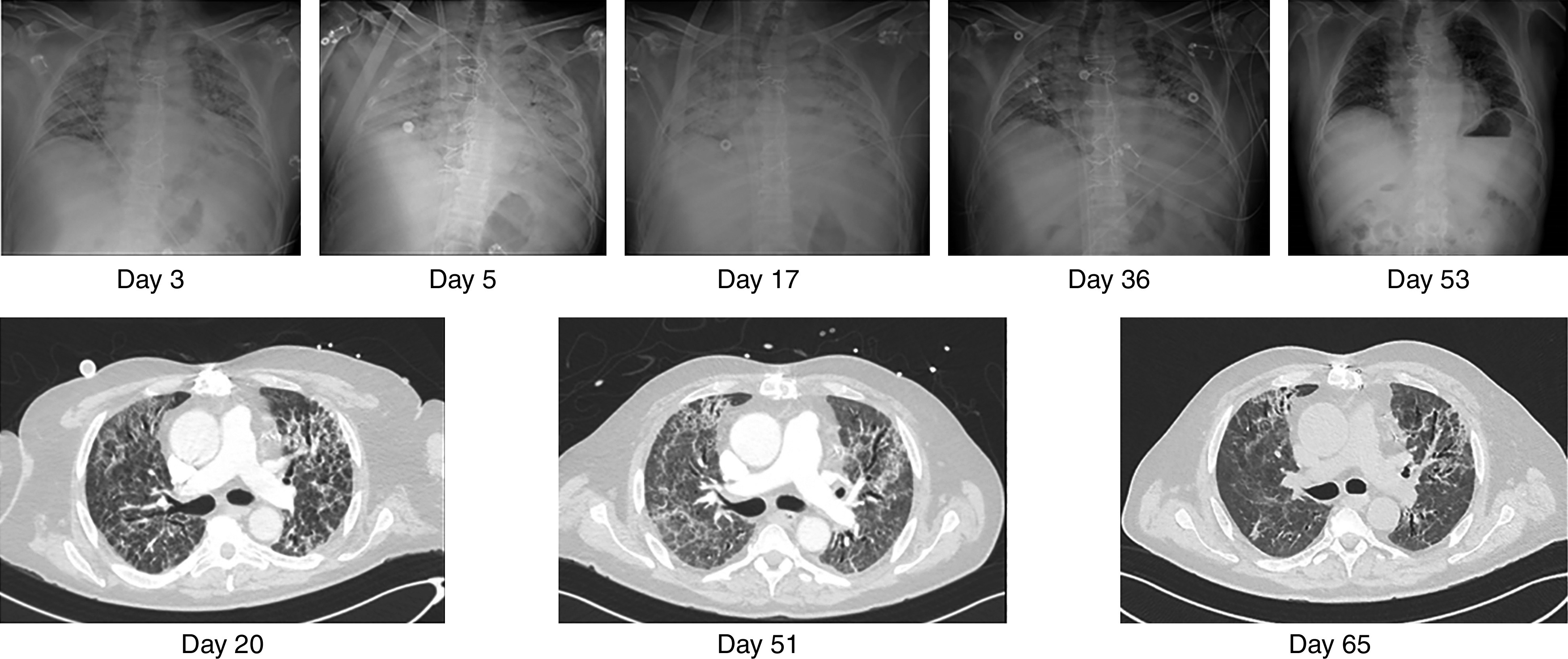
Radiological imaging during the hospital stay.
On Day 24, Enterococcus faecalis infection of the jugular cannula and bacteremia were diagnosed and corticosteroids suspended. Because positive blood cultures persisted despite prolonged intravenous amoxicillin on Day 36 and the patient could not be weaned off ECMO, the return jugular cannula was removed and replaced by a right femoral cannula. Amoxicillin was maintained until Day 48 (i.e., 48 h after ECMO weaning). Notably, he experienced only one nosocomial pneumonia episode on Day 17 during his 48 days in the ICU.
He performed active physical exercises daily in bed with a physiotherapist. On Day 18, he was able to stand up, with assistance. Oral feeding was maintained throughout his ICU stay, as was social interaction by phone or face to face with his relatives. Moreover, the patient was informed daily of his health status and medical decisions and was always able to express his preferences.
On Day 46, he was successfully weaned off ECMO (i.e., after 41 d). Forty-eight hours after ECMO weaning, the patient was able to walk around his bed and was cycling to a chair. He was discharged from the ICU to the Pulmonology Step-Down Unit on Day 51. He lost 7 kg during his ICU stay with serum albumin at 32 g/L at ICU discharge. He was discharged from the hospital and transferred to a rehabilitation center on Day 66 with oxygen 2 L/min at rest. At that time, his chest computed tomography showed significant regression of posterior basal, middle, and superior condensations, reticulations with the persistence of fibrosis features, and traction bronchiectasis (Figure 2).
This “fully awake” ECMO strategy enables active treatment participation and ambulation and might avoid complications associated with heavy sedation, paralyzing agents, and prolonged MV. Indeed, unlike data reported for patients with COVID-19 with long ECMO runs (1), our patient had only one episode of pulmonary bacterial superinfection due to oropharyngeal bacteria. Moreover, daily active mobilization limited ICU-acquired weakness and preserved consciousness. As previously suggested, awake VV-ECMO for nonintubated, spontaneously breathing patients with ARDS seems more suitable for selected patients with isolated lung injury (6). Furthermore, the remarkable dissociation between profound hypoxemic respiratory failure and low proportional signs of respiratory distress and sense of dyspnea frequently reported in COVID-19 (9) might have facilitated the control of our patient’s respiratory drive and contributed to the good tolerance of this “awake” strategy (10).
ECMO instead of invasive MV to maintain an awake patient is investigational and requires further exploration in patients with COVID-19–associated ARDS. This strategy could be theoretically proposed to a large number of patients with COVID-19 as 43–56% initially treated with high-flow nasal oxygen or NIV required invasive ventilation (11, 12). However, we have to acknowledge that these numbers are highly speculative, as necessary prerequisites, such as isolated lung impairment, preserved peripheral muscle strength and airway clearance, ability to remain immobilized supine during the procedure, no hemostasis disorder, experienced physician or surgeon for ECMO cannulation, and clear information of the patient and her or his relatives on the risks and remaining uncertainties of this strategy, are needed. Awake ECMO patients with strong spontaneous respiratory efforts and associated large transpulmonary pressure swings may also be at risk of harmful “self-inflicted lung injury” (13). Indeed, in a cohort of 30 patients with ARDS, only 8 (27%) could be maintained spontaneously breathing, for at least some time, during ECMO (14). Considering the overall severity of COVID-19–associated ARDS, it is likely that the final proportion of patients with COVID-19 who are candidates for an awake ECMO strategy would likely be lower, maybe in the 5–15% range.
For those carefully selected patients, this strategy would enable active physical therapy (i.e., dynamic quadriceps training, bed-to-chair mobilization, or standing or stationary marching) and ambulation (15). Besides, it could become a promising alternative to invasive MV to limit its associated delirium, infectious risks, loss of muscle mass, and critical illness myopathy and polyneuropathy, while maintaining the patient’s ability to communicate with relatives, friends, and medical staff (16). Of note, patients undergoing the femoro-jugular approach can be also successfully mobilized, independent of the cannulation site (15). However, careful monitoring of ECMO-associated risks is essential, and this strategy should be further evaluated in experienced ECMO centers.
Acknowledgments
Acknowledgment
The authors thank the patient, who gave his written consent for publication.
Footnotes
Author Contributions: M.S. and A.C. wrote the manuscript. All authors contributed to the revision of, read, and approved the final manuscript version of the manuscript. M.S. takes responsibility for the integrity of the work as a whole, from inception to published article.
Originally Published in Press as DOI: 10.1164/rccm.202102-0259LE on April 26, 2021
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Schmidt M, Hajage D, Lebreton G, Monsel A, Voiriot G, Levy D, et al. Groupe de Recherche Clinique en REanimation et Soins intensifs du Patient en Insuffisance Respiratoire aiguE (GRC-RESPIRE) Sorbonne Université; Paris-Sorbonne ECMO-COVID investigators. . Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med. 2020;8:1121–1131. doi: 10.1016/S2213-2600(20)30328-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, et al. Extracorporeal Life Support Organization. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet. 2020;396:1071–1078. doi: 10.1016/S0140-6736(20)32008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47:60–73. doi: 10.1007/s00134-020-06294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mustafa AK, Alexander PJ, Joshi DJ, Tabachnick DR, Cross CA, Pappas PS, et al. Extracorporeal membrane oxygenation for patients with COVID-19 in severe respiratory failure. JAMA Surg. 2020;155:990–992. doi: 10.1001/jamasurg.2020.3950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stahl K, Seeliger B, Hoeper MM, David S. “Better be awake”-a role for awake extracorporeal membrane oxygenation in acute respiratory distress syndrome due to Pneumocystis pneumonia. Crit Care. 2019;23:418. doi: 10.1186/s13054-019-2703-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hoeper MM, Wiesner O, Hadem J, Wahl O, Suhling H, Duesberg C, et al. Extracorporeal membrane oxygenation instead of invasive mechanical ventilation in patients with acute respiratory distress syndrome. Intensive Care Med. 2013;39:2056–2057. doi: 10.1007/s00134-013-3052-3. [DOI] [PubMed] [Google Scholar]
- 7. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. RECOVERY Collaborative Group Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mauri T, Turrini C, Eronia N, Grasselli G, Volta CA, Bellani G, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1207–1215. doi: 10.1164/rccm.201605-0916OC. [DOI] [PubMed] [Google Scholar]
- 9. Wilkerson RG, Adler JD, Shah NG, Brown R. Silent hypoxia: A harbinger of clinical deterioration in patients with COVID-19. Am J Emerg Med. 2020;38:2243.e5–2243.e6. doi: 10.1016/j.ajem.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dhont S, Derom E, Van Braeckel E, Depuydt P, Lambrecht BN. The pathophysiology of ‘happy’ hypoxemia in COVID-19. Respir Res. 2020;21:198. doi: 10.1186/s12931-020-01462-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Demoule A, Vieillard Baron A, Darmon M, Beurton A, Géri G, Voiriot G, et al. High-flow nasal cannula in critically iii patients with severe COVID-19. Am J Respir Crit Care Med. 2020;202:1039–1042. doi: 10.1164/rccm.202005-2007LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grieco DL, Menga LS, Cesarano M, Rosà T, Spadaro S, Bitondo MM, et al. COVID-ICU Gemelli Study Group. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: The HENIVOT randomized clinical trial. JAMA. doi: 10.1001/jama.2021.4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vaporidi K, Akoumianaki E, Telias I, Goligher EC, Brochard L, Georgopoulos D. Respiratory drive in critically ill patients. Pathophysiology and clinical implications. Am J Respir Crit Care Med. 2020;201:20–32. doi: 10.1164/rccm.201903-0596SO. [DOI] [PubMed] [Google Scholar]
- 14. Crotti S, Bottino N, Ruggeri GM, Spinelli E, Tubiolo D, Lissoni A, et al. Spontaneous Breathing during Extracorporeal Membrane Oxygenation in Acute Respiratory Failure. Anesthesiology. 2017;126:678–687. doi: 10.1097/ALN.0000000000001546. [DOI] [PubMed] [Google Scholar]
- 15. Hermens JA, Braithwaite SA, Platenkamp M, Wijnandts PR, Van de Graaf EA, van der Kaaij NP, et al. Awake ECMO on the move to lung transplantation: serial monitoring of physical condition. Intensive Care Med. 2017;43:707–708. doi: 10.1007/s00134-016-4667-y. [DOI] [PubMed] [Google Scholar]
- 16. Langer T, Santini A, Bottino N, Crotti S, Batchinsky AI, Pesenti A, et al. “Awake” extracorporeal membrane oxygenation (ECMO): pathophysiology, technical considerations, and clinical pioneering. Crit Care. 2016;20:150. doi: 10.1186/s13054-016-1329-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


