Introduction
Recent observations of improvement in keloids with the administration of dupilumab have led to research that has implicated interleukin (IL) 4 and IL-13 signaling as potential mediators of sclerosing and fibrotic skin diseases, particularly with increased expression of transforming growth factor β downstream of IL-13.1, 2, 3 As such, dupilumab, an IL-4 receptor α antagonist, inhibits IL-4 and IL-13 signaling and has been suggested as a potential treatment for sclerosing disorders, with an active phase 2 interventional randomized placebo-controlled trial currently underway investigating its efficacy in morphea.
Here, we present the case of a patient developing morphea while being treated with dupilumab. This potential paradoxical reaction, where a postulated therapy appears to contribute to the pathogenesis of the disease, has been reported in psoriasis, in which the inhibition of tumor necrosis factor α through its inhibitors leads to increased activity of interferon α, postulated to induce disease development.4
Case report
A woman in her 20s with a history of atopy and a 2-year history of refractory dermatitis with components of atopic and allergic contact dermatitis was referred to our dermatology clinic for management. Previously, the patient's condition had not improved with topical steroids; phototherapy; and strict avoidance of her contact allergens elicited by patch testing, including rubber additives, dyes, formaldehyde, and textile allergens. The patient was started on dupilumab, which significantly improved her dermatitis and associated pruritus. However, 8 months into therapy, multiple indurated plaques developed on the bilateral upper and lower extremities.
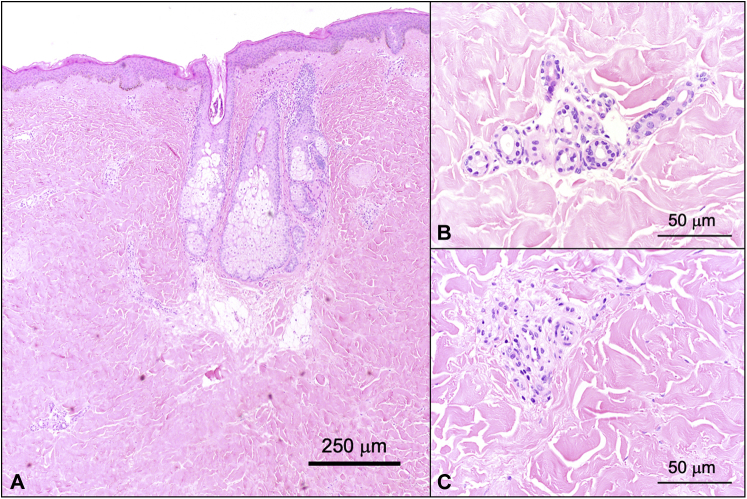
Suspecting an evolving sclerosing disorder such as morphea or eosinophilic fasciitis, a punch biopsy from the right upper extremity was obtained. Histopathology revealed evidence of sclerosing dermopathy (Fig 1). The patient had no history of Raynaud phenomenon, thickening of the skin of the hands, autoantibodies, or other systemic symptoms, and a diagnosis of morphea was favored. Dupilumab was discontinued in the setting of her morphea, and the patient was initiated on mycophenolate mofetil. Over the ensuing 7 months, she reported significant softening of the sclerotic plaques on her arms and legs.
Fig 1.
Localized scleroderma (morphea). Expansion of the dermis by thickened, sclerotic collagen bundles (A) with a paucity of dermal blood vessels and loss of adipose tissue surrounding the eccrine glands (B, C). (Original magnifications: A, ×40; B, ×400; C, ×400.)
Discussion
Herein, we discuss potential mechanisms that may explain this phenomenon. There are many splice variants of IL-4. Inhibition of IL-4 with dupilumab may result in enhanced production of 1 such variant, IL-4δ2, which has been implicated in sclerotic disorders such as systemic sclerosis. In vivo studies have demonstrated that IL-4δ2 leads to the accumulation of T and B lymphocytes, the production of proinflammatory cytokines such as interferon γ and tumor necrosis factor α, and an increased accumulation of collagen in the tissue.5 IL-4δ2 has been shown to be secreted when the levels of full-length IL-4 decline; thus, it is possible that targeting IL-4 with dupilumab increases the production of the proinflammatory splice variant, which may result in disease pathogenesis.5
We also hypothesize that dupilumab may participate in decoy receptor binding and, therefore, paradoxically signal transforming growth factor β and a profibrotic IL-13.2,6 Dupilumab's effect on IL-4/13 signaling may paradoxically shift the body's natural wound healing mechanisms into a state of over repair, characterized by pathologic collagen deposition and the inability to restore tissue function, resulting in excessive scar tissue. This case offers a presentation of morphea developing in the setting of dupilumab treatment for atopic and allergic contact dermatitis. We acknowledge that correlation does not equal causation; however, it is interesting to note a case of fibrosis developing while on dupilumab. Further investigation is warranted to fully elucidate the effect of IL-4 and IL-13 inhibition on sclerosing disorders of the skin.
Conflicts of interest
Dr Merola is a consultant and/or investigator for AbbVie, Dermavant, Eli Lilly, Novartis, Janssen, UCB, Celgene, Sanofi-Regeneron, Biogen, Pfizer, and Leo Pharma. Authors Kassamali, Elman, Sheets, and LaChance have no conflicts of interest to declare.
Footnotes
Drs Kassamali and Elman are cofirst authors.
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Diaz A., Tan K., He H. Keloid lesions show increased IL-4/IL-13 signaling and respond to Th2-targeting dupilumab therapy. J Eur Acad Dermatol Venereol. 2020;34(4):e161–e164. doi: 10.1111/jdv.16097. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen J.K., Austin E., Huang A., Mamalis A., Jagdeo J. The IL-4/IL-13 axis in skin fibrosis and scarring: mechanistic concepts and therapeutic targets. Arch Dermatol Res. 2020;312(2):81–92. doi: 10.1007/s00403-019-01972-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maeda D., Kubo T., Kiya K. Periostin is induced by IL-4/IL-13 in dermal fibroblasts and promotes RhoA/ROCK pathway-mediated TGF-β1 secretion in abnormal scar formation. J Plast Surg Hand Surg. 2019;53(5):288–294. doi: 10.1080/2000656X.2019.1612752. [DOI] [PubMed] [Google Scholar]
- 4.Vasconcellos J.B., Pereira D.D., Vargas T.J., Levy R.A., Pinheiro G.D., Cursi Í.B. Paradoxical psoriasis after the use of anti-TNF in a patient with rheumatoid arthritis. An Bras Dermatol. 2016;91(5 suppl 1):137–139. doi: 10.1590/abd1806-4841.20164456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luzina I.G., Keegan A.D., Heller N.M., Rook G.A.W., Shea-Donohue T., Atamas S.P. Regulation of inflammation by interleukin-4: a review of “alternatives.”. J Leukoc Biol. 2012;92(4):753–764. doi: 10.1189/jlb.0412214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fichtner-Feigl S., Strober W., Kawakami K., Puri R.K., Kitani A. IL-13 signaling through the IL-13α2 receptor is involved in induction of TGF-β1 production and fibrosis. Nat Med. 2006;12(1):99–106. doi: 10.1038/nm1332. [DOI] [PubMed] [Google Scholar]