Abstract
Vertebral artery injuries account for approximately 19% of cerebral vascular injuries and are typically managed conservatively. However, some patients require operative intervention to gain control of an active hemorrhage, either via surgical ligation or endovascular intervention. We present a case of iatrogenic vertebral artery injury occurring during cervical spine surgery which was treated emergently with a self-expanding covered stent. A 58-year-old male presented for cervical traction, C5 and C6 corpectomy, and possible C4 to T2 posterior fusion following a motor vehicle accident. Intraoperatively, following drilling the C5 endplate, copious bleeding was observed from injury to the right vertebral artery resulting in pseudoaneurysm formation. The patient was loaded with ticagrelor and a self-expanding covered stent was placed via a transfemoral approach, resulting in obliteration of the pseudoaneurysm prior to completion of his cervical spine surgery. Emergent self-expanding covered stent placement for iatrogenic vertebral artery injury in the setting of an intraoperative injury is a safe and effective option. Ticagrelor is a viable alternative to traditional dual antiplatelet therapy for preventing thromboembolic complications in this urgent setting.
Keywords: Covered stent, Endovascular therapy, Vertebral artery, Trauma, Pseudoaneurysm
INTRODUCTION
The incidence of vertebral artery injury has risen with the rise of routine angiography in neurosurgical practice, increasing from 3% to 19% of all cervical vascular injuries [10]. While previous work has demonstrated that clinically occult, radiographically detected, and minimally vascular injuries can safely be managed without operative intervention, some patients require emergency surgery to gain control of an active hemorrhage [12]. Vertebral artery injuries are technically challenging to even the most experienced surgeons, and aside from observation, have been traditionally treated with surgical ligation or endovascular occlusion [3]. We present a case of iatrogenic vertebral artery injury and subsequent pseudoaneurysm formation with active extravasation managed with endovascular self-expanding covered stent placement.
DESCRIPTION OF CASE
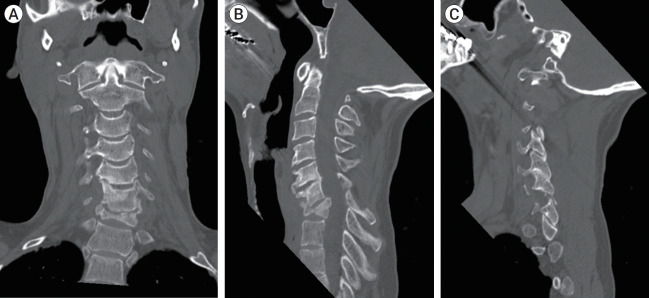
A 58-year-old male presented 8 months following a motor vehicle accident in which he was found to have a C7 fracture with a focal kyphotic deformity. At the time of his accident, he was managed conservatively with a cervical collar, but he continued to have severe neck pain, pain going in between his shoulder blades into his right scapula and limited right deltoid movement. Follow-up imaging revealed a persistent focal kyphosis at C6-C7 associated with a C7 burst fracture with retropulsion into the spinal canal and left C6-C7 perched facets (Fig. 1). Cervical traction followed by C6 and C7 corpectomy with anterior fusion, and possible C4 to T2 posterior fusion were planned. The patient’s physical exam prior to surgery was unremarkable with exception his kyphotic posture.
Fig. 1.
Pre-operative computed tomography. Coronal view (A) revealed C7 burst fracture. Mid-sagittal view (B) revealed retropulsion of the burst segment into the spinal canal. Sagittal view (C) revealed C6 on C7 perched facet fractures.
Intraoperatively, the patient underwent cervical traction (starting at 10 pounds and sequentially increased up to 50 pounds), which resulted in reduction of his kyphosis. The patient then underwent an anterior C6 and C7 corpectomy. While performing the final drilling of the C5 endplate to accommodate the expandable cage, brisk arterial bleeding was encountered. The bleeding was controlled with packing and direct pressure.
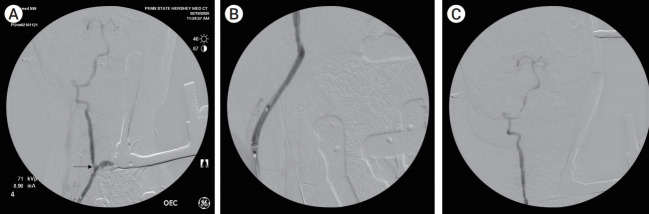
The neurovascular surgery team was consulted and an intraoperative diagnostic angiogram was performed via a transfemoral approach using OEC 9800 C-arm (GE Healthcare, Chicago, IL, USA). The right vertebral artery was catheterized with a 5-French Berenstein catheter (Cordis, Hialeah, FL, USA) navigated over a Terumo 0.035 inch Glidewire (Terumo Medical, Tokyo, Japan). Review of the images revealed medial deviation of the vertebral artery at C7 with a focal area of contrast extravasation, concerning for either active bleeding or pseudoaneurysm formation (Fig. 2). The artery remained patent and brisk flow into intracranial circulation was observed. Of note, based on pre-procedure imaging, the right vertebral artery was the dominant artery. Therefore, the decision was made to place a covered stent in order to preserve the vertebral artery and repair the area of injury. The patient was loaded with ticagrelor (180 mg) via orogastric tube. Intravenous heparin was not administered. A 7-French RAABE sheath (Flexor RAABE Guiding Sheath, Cook Medical, Bloomington, IN, USA) was placed in the proximal right vertebral artery. After the lesion was crossed with an 0.035 inch exchange wire, a self-expanding covered stent (Gore Viabahn Endoprosthesis, Gore Medical, Flagstaff, AZ, USA) was placed across the area of contrast extravasation (Fig. 2). Follow-up angiograms revealed no extravasation of contrast or further opacification of the suspected pseudoaneurysm. Intracranially, all major vessels remained patent (Fig. 2). The catheters were removed and an 8-French Angio-Seal closure device was deployed without difficulty at the femoral artery puncture site.
Fig. 2.
Diagnostic angiogram following severe bleeding due to iatrogenic right-sided vertebral injury. Angiogram (A) demonstrates medial deviation of the right vertebral artery and a focal area of extravasation at C7 (arrow). (B) Angiogram demonstrat es placement of Viabahn covered stent. Angiogram (C) does not demonstrate opacification of suspected pseudoaneurysm, signaling obliteration.
The patient’s cervical spine fusion was continued with placement of an expandable cage and C5 to T1 arthrodesis with synthetic bone matrix. The patient was admitted to the intensive care unit intubated but was quickly weaned off the ventilator and extubated. He was discharged on post-operative day two and ticagrelor 60 mg every 12 hours was prescribed for 3 months. The patient remained neurologically intact following his procedure with improved pain levels.
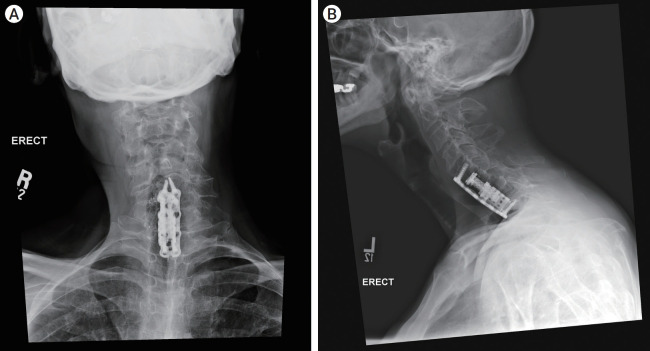
The patient was last seen nine months following his initial operation, at which time he was neurologically intact, and his pain levels were unchanged. He had good improvement in his cervical lordosis. Imaging revealed bony fusion and appropriate hardware placement (Fig. 3).
Fig. 3.
Post-operative cervical x-ray (A: AP view, B: lateral view) nine months post-operatively demonstrating correction of kyphosis, presence of bony fusion, and lack of hardware defects.
DISCUSSION
To our knowledge, we present only the third case of iatrogenic vertebral artery injury during cervical spine surgery treated with a covered stent (Table 1) [2,7]. Prior to our case, the vertebral artery lesions treated with covered stents consisted of two pseudoaneurysms; one due to a traction maneuver to place a prosthesis between C4 and C5 and another following drilling for a C5 and C6 corpectomy [2,7]. In the present case, the patient developed a pseudoaneurysm and active vertebral artery bleeding as a consequence of drilling the superior vertebral endplate while attempting to place an expandable cage. Unique to our case, however, is the successful implantation of a Viabahn self-expanding covered stent and the utilization of ticagrelor alone during and after the procedure for thromboembolism protection. Importantly, the emergent stenting procedure was performed at the time of the injury, in the operating room using portable C-arm technology.
Table 1.
A review of previous case reports and case series detailing iatrogenic, intraoperative injury of the vertebral artery during cervical spine surgery treated with covered stent placement
| Author/Year | Patients, n | Age/Gender | Etiology | AVF | VVF | Dissection | Pseudoaneurysm | Indication | Stent type |
|---|---|---|---|---|---|---|---|---|---|
| Carrillo-Martinez et al. (2020) [2] | 1 | 57/Male | Traction maneuver for C4 to C5 disc prosthesis- Intraoperative injury | No | No | No | Yes | Stroke pre- vention | Covered stent |
| Katsaridis et al. (2007) [7] | 1 | 74/Male | C5 and C6 corpectomy- Intraoperative injury | No | No | No | Yes | Active bleeding | Symbiot covered stent |
| Present case/2020 | 1 | 58/Male | Traction, C6 and C7 corpectomy, C5 to T1 arthrodesis and cage placement-Intraoperative injury | No | No | No | Yes | Active bleeding | Viabahn covered stent |
| Total | 3 | 1 | 0 | 0 | 3 |
AVF, arteriovenous fistula
In the present case, we report the use of the self-expanding Viabahn expanded polytetrafluoroethylene (ePTFE)-covered endoprosthesis, marking the first time its use has been described in iatrogenic vertebral artery injury. This covered stent has been primarily utilized in the treatment of peripheral vascular disease and has been studied in the VIASTAR, VIBRANT, and VIPER randomized clinical trials [4,9,11]. Compared to bare metal stents, the Viabahn covered stent has a significantly higher 12-month patency rate (70.9% to 73% vs. 53.5%) [9,11]. In extracranial vertebral artery iatrogenic injury, ePTFE-covered stents would intuitively appear to be more effective given their lack of porosity allows completely coverage of the area of injury. Of note, balloon-mounted covered stents were used in both of the previously reported cases and both procedures appear to have been performed in a dedicated angiography suite after closure of the spinal surgery. In one case, however, an initial attempt at treatment using a balloon mounted stent was unsuccessful as the rigidity of the stent precluded adequate placement [7]. Self-expanding stents, like the Viabahn stent used in this case offer the benefit of increased flexibility compared to balloon-expandable stents, this flexibility can be crucial when accessing the often tortuous neurovasculature.
In the peri-operative period, dual antiplatelet therapy (DAT) is traditionally initiated in order to reduce the risk of thromboembolic or ischemic events. Aspirin and clopidogrel are the most common components in DAT and have been associated with reducing death, reinfarction, and stroke by 15% [1]. In the two previously reported cases, intravenous heparin was also administered intraoperatively followed by aspirin and clopidogrel DAT with good results [2,7]. However, in one case the patient developed a symptomatic neck hematoma postoperatively, which required urgent surgical evacuation. It is quite possible that the combination of anticoagulation and dual antiplatelet therapy contributed to an increased risk of post-operative hemorrhage [2]. Conversely, the reported rate of clopidogrel hyporesponsiveness in patients undergoing neuroendovascular procedures varies from 21% to 53.1% [8] making the drug less than ideal for urgent or emergent situations where a potent and reliable antiplatelet effect is needed. Ticagrelor, unlike clopidogrel, is not a prodrug and therefore, does not require metabolic activation, the major source of variability in patient response to clopidogrel [5]. A study highlighting the safety of ticagrelor in neuroendovascular procedures in clopidogrel non-responders demonstrated immediate platelet inhibition following a ticagrelor loading dose [6]. Ticagrelor has been shown to be effective in reducing the prevalence of high platelet reactivity and patients given this antiplatelet agent have been found to have platelet reactivity below cutoffs associated with ischemic risk with minimal risk of hemorrhage [5,6]. The choice of ticagrelor alone in this case demonstrates the potential benefit of utilizing this agent in preventing thromboembolic complications while minimizing the risk of hemorrhage.
CONCLUSIONS
We present a case of a 58-year male with an iatrogenic vertebral artery injury during cervical spine surgery causing active extravasation and pseudoaneurysm formation. The patient was successfully treated with a self-expanding Viabahn covered stent, the first case utilizing this particular stent type in an acute iatrogenic vertebral artery injury. This case also demonstrates the feasibility of performing such stent repair intraoperatively in a standard operating room without specialized “hybrid” equipment while using ticagrelor as single antiplatelet therapy for the prevention of thromboembolic complications. It is important for spinal and neuroendovascular surgeons to be aware of these options for management of this fortunately rare complication.
Footnotes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
REFERENCES
- 1.Bowry AD, Brookhart MA, Choudhry NK. Meta-analysis of the efficacy and safety of clopidogrel plus aspirin as compared to antiplatelet monotherapy for the prevention of vascular events. Am J Cardiol. 2008 Apr 1;101(7):960–6. doi: 10.1016/j.amjcard.2007.11.057. [DOI] [PubMed] [Google Scholar]
- 2.Carrillo-Martínez MÁ, Garza García GA, Leal Jacinto JM. Iatrogenic left vertebral artery pseudoaneurysm treated with a covered stent. BJR Case Rep. 2020 Sep 29;6(2):20190051. doi: 10.1259/bjrcr.20190051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demetriades D, Theodorou D, Asensio J, Golshani S, Belzberg H, Yellin A, et al. Management options in vertebral artery injuries. Br J Surg. 1996 Jan;83(1):83–6. doi: 10.1002/bjs.1800830126. [DOI] [PubMed] [Google Scholar]
- 4.Geraghty PJ, Mewissen MW, Jaff MR, Ansel GM, VIBRANT Investigators Three-year results of the VIBRANT trial of VIABAHN endoprosthesis versus bare nitinol stent implantation for complex superficial femoral artery occlusive disease. J Vasc Surg. 2013 Aug;58(2):386–95. doi: 10.1016/j.jvs.2013.01.050. [DOI] [PubMed] [Google Scholar]
- 5.Gurbel PA, Bliden KP, Butler K, Antonino MJ, Wei C, Teng R, et al. Response to ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: the RESPOND study. Circulation. 2010 Mar 16;121(10):1188–99. doi: 10.1161/CIRCULATIONAHA.109.919456. [DOI] [PubMed] [Google Scholar]
- 6.Safety and efficacy of ticagrelor for neuroendovascular procedures. A single center initial experience. J Neurointerv Surg. 2014 May;6(4):320–2. doi: 10.1136/neurintsurg-2013-010699. [DOI] [PubMed] [Google Scholar]
- 7.Katsaridis V, Papagiannaki C, Violaris C. Treatment of an iatrogenic vertebral artery laceration with the Symbiot self expandable covered stent. Clin Neurol Neurosurg. 2007 Jul;109(6):512–5. doi: 10.1016/j.clineuro.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 8.Kim KS, Fraser JF, Grupke S, Cook AM. Management of antiplatelet therapy in patients undergoing neuroendovascular procedures. J Neurosurg. 2018 Oct;129(4):890–905. doi: 10.3171/2017.5.JNS162307. [DOI] [PubMed] [Google Scholar]
- 9.Lammer J, Zeller T, Hausegger KA, Schaefer PJ, Gschwendtner M, Mueller-Huelsbeck S, et al. Heparin-bonded covered stents versus bare-metal stents for complex femoropopliteal artery lesions: the randomized VIASTAR trial (Viabahn endoprosthesis with PROPATEN bioactive surface [VIA] versus bare nitinol stent in the treatment of long lesions in superficial femoral artery occlusive disease) J Am Coll Cardiol. 2013 Oct 8;62(15):1320–7. doi: 10.1016/j.jacc.2013.05.079. [DOI] [PubMed] [Google Scholar]
- 10.Meier DE, Brink BE, Fry WJ. Vertebral artery trauma: acute recognition and treatment. Arch Surg. 1981 Feb;116(2):236–9. doi: 10.1001/archsurg.1981.01380140082021. [DOI] [PubMed] [Google Scholar]
- 11.Saxon RR, Chervu A, Jones PA, Bajwa TK, Gable DR, Soukas PA, et al. Heparin-bonded, expanded polytetrafluoroethylene-lined stent graft in the treatment of femoropopliteal artery disease: 1-year results of the VIPER (Viabahn Endoprosthesis with Heparin Bioactive Surface in the Treatment of Superficial Femoral Artery Obstructive Disease) trial. J Vasc Interv Radiol. 2013 Feb;24(2):165–73. doi: 10.1016/j.jvir.2012.10.004. quiz 174. [DOI] [PubMed] [Google Scholar]
- 12.Stain SC, Yellin AE, Weaver FA, Pentecost MJ. Selective management of nonocclusive arterial injuries. Arch Surg. 1989 Oct;124(10):1136–40. doi: 10.1001/archsurg.1989.01410100034007. discussion 1140. [DOI] [PubMed] [Google Scholar]