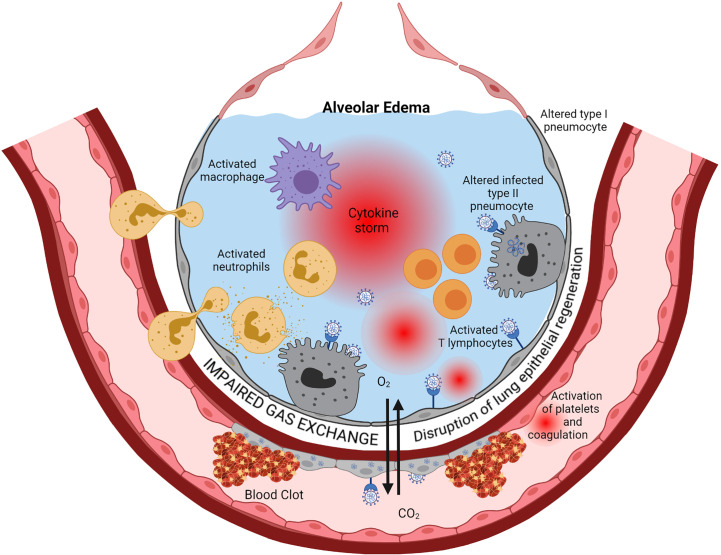
Figure 1.
Immunopathology of ARDS. Cytopathic SARS-CoV-2 infection of pulmonary epithelial cells and endothelial cells is the starting point of a series of cascading pro-inflammatory events leading to ARDS eventually. Viral replication, via activation of the innate immune response components such as TLR, triggers the production of interferons, inflammatory cytokines, and chemokines. This inflammation induces infiltration into the alveoli and activation of neutrophils, macrophages, and lymphocytes. Activated immune cells produce large amounts of pro-inflammatory cytokines such as IL-6, IL-1β, TNF-α, and IL-8 that exacerbate local cell recruitment and activation, leading to a “cytokine storm” through this amplification loop. The increase of capillary permeability causes pulmonary edema. Thrombosis occurs via several mechanisms, including injury of endothelial cells by the virus and subsequent activation of the coagulation cascade, activation of neutrophils that secrete procoagulant factors, and activation of complement that leads to activation of platelet and coagulation. Regeneration of the lung epithelia is impaired. This cascade of events ends in a severe impairment of Gas exchanges between alveoli and lung capillaries, causing hypoxemia. Created with BioRender.com.