Abstract
This study aimed to explore the differences between the effectiveness of using a combination of rehabilitation and acceptance commitment therapy (ACT), and rehabilitation therapy alone for the treatment of spinal cord injury (SCI). The newly admitted patients with spinal cord injury whose post-traumatic stress disorder (PTSD) score was higher than 38 points were randomly categorized into the treatment group and control group, with 30 patients in each group. One group underwent ACT and rehabilitation treatment, while the other underwent rehabilitation treatment only. PTSD and functional independence measure (FIM) scores were evaluated. Changes in scores were compared between the two groups before, one month, two months, and three months after treatment. The total PTSD score in SCI patients who were treated with ACT was significantly different before and after treatment (P < 0.05). Total FIM scores were also significantly different before and after treatment (P < 0.05). The FIM score in the treatment group was significantly higher than that in the control group after 2 and 3 months of treatment (P < 0.05). The combination of rehabilitation therapy and ACT could immediately reduce stress levels and significantly improve impaired function, lifelong self-care ability, and the impact of rehabilitation therapy.
Keywords: Acceptance commitment therapy, Spinal cord injury, Motor function, Stress level, Rehabilitation therapy
1. Introduction
Spinal cord injury (SCI) refers to spinal cord conduction and motor function impairment caused by direct or indirect external factors. These injuries manifest as various motor, sensory, and sphincter dysfunctions; abnormal muscle tension; and a pathological reflex in the area controlled by the corresponding damaged segments.
SCI sites include the cervical spinal cord, thoracic spinal cord, lumbar spinal cord, conus medullaris, and cauda equine [1]. The severity of the injury ranges from complete to incomplete sectioning. Previously healthy people suddenly become paraplegic or quadriplegic due to accidents resulting in self-care impairments, requiring assistance from family members to defecate, sexual dysfunction, inability to work or attend school, and restricted social communication skills. These series of sudden negative events cause psychological stress in SCI patients that experience stages of ignorance, shock, denial, depression, opposition, independence, and adaptation [2].
Although the patients' limb function and self-care ability can be improved with rehabilitation therapy alone, most patients still retain different degrees of physical disability. Finding a way to improve the body's function to the greatest extent and reduce the degree of disability presents a significant difficulty in the field of rehabilitation medicine. As the current medical technology has not solved this problem, spinal cord injury remains a mental blow and causes a great deal of stress to patients. This kind of stress may have a negative impact on the rehabilitation of SCI patients while stress relief could improve its efficacy.
The study aimed to examine the effect of acceptance commitment therapy (ACT) in traumatic stressed SCI patients in reducing the psychological stress response, identifying differences between combined rehabilitation treatment and conventional rehabilitation alone, improving the rehabilitation effect in SCI patients, and reducing the degree of disability.
2. Materials and methods
2.1. Inclusion criteria
This study was approved by our ethics committee. Patients were included if (1) they met the SCI diagnostic criteria according to ICD-10 and (2) had no impaired consciousness and could provide a voluntary informed consent for this study.
2.2. Exclusion criteria
Patients were excluded from the study if (1) they had a history of mental illnesses and/or were on psychoactive drugs, and (2) were unconscious or unable to participate in psychotherapy.
2.3. Object grouping
Patients who met the above study criteria were randomly divided into a treatment group (rehabilitation treatment and ACT group) and a control group (rehabilitation treatment group). The 30 patients in the treatment group who completed the entire rehabilitation and ACT treatment included 20 men and 10 women aged 46.33 ± 17.17 years. The 30 patients in the control group who completed the entire rehabilitation treatment included 24 men and 6 women aged 43.73 ± 13.52 years. T test was used in the two groups. There was no significant difference between the treatment and control groups in terms of the demographic data (including sex, age, nationality, permanent residence, and years of education) and clinical characteristics (diagnosis, course of disease, and first onset of questionnaire survey data) (P > 0.05). The two groups were matched for the level and severity of spinal cord injury but were not matched for sex and cognitive level. The t-test could overcome the error caused by the above unbalanced conditions.
2.4. Test scales used in the treatment and control groups
2.4.1. Post-traumatic stress disorder (PTSD) scale
This scale is composed of 17 items. Each item has 7 grades, with a total score range of 17–85. The higher the score, the more serious the PTSD symptoms [3]. A score of 17–37 points showed no obvious PTSD symptoms; 38–49 points showed PTSD symptoms to a certain extent; and 50–58 points showed obvious PTSD symptoms.
2.4.2. Functional independence measure (FIM) scale
It includes two parts—motor function and cognitive function parts. The motor function part included self-care ability, sphincter control, and transfer and walking ability. The cognitive function part included communication ability and social cognition. Each item had 7 grades; 7 indicated complete independence and 1 indicated absolute dependence. The total FIM score was in the range of 18–126. The higher the score, the stronger the independent ability [4]. A score of 18 points meant complete dependence; 19–35 points meant extremely severe dependence; 36–53 points meant severe dependence; 54–71 points meant moderate dependence; 72–89 points meant mild dependence; 90–107 points meant conditional independence or mild dependence; 108–125 points meant basic independence; and 126 points meant complete independence.
2.5. Measurements
Test scale: FIM functional recovery was measured by licensed rehabilitation therapists, and a relief in PTSD symptoms was measured by licensed psychiatrists.
Evaluation using the PTSD and FIM scales was performed on the second day after admission and after one, two, and three months of treatment. Between- and within-group comparisons were performed for the control and treatment groups.
2.5.1. Rehabilitation treatment and nursing
In the control and treatment groups, rehabilitation treatment was conducted 5 days a week, 4 weeks per course, for a total of 3 courses. The rehabilitation nursing process involved steps such as right limb placement, skin care, and perineum care [5].
Rehabilitation evaluation included evaluation of the injured segments, sensory and motor scores, evaluation of muscle strength and muscle tension below the injury plane [6], and evaluation of the bladder, intestinal tract, and autonomic nerve function [2]. Rehabilitation treatment included comprehensive limb training, respiratory function training, balance training for sitting and standing, and bladder and intestinal function training [7].
2.5.2. Acceptance commitment therapy (ACT)
According to the previously published method [8], this treatment involved psychological intervention once a week, four 50-min sessions for each stage, for three stages, making a total of 12 times. The first psychotherapy method involved establishing a good doctor–patient relationship. According to the ACT method, we focused on six pathological models of patients; six treatment measures were used to improve the psychological flexibility of SCI patients and to ease their PTSD symptoms.
3. Results
3.1. Comparison of total PTSD scores and FIM scores between the two groups at each time point
There was no significant difference in the total PTSD score between the treatment and control groups at admission (t = 0.273) and 1 month after treatment (t = 1.939; P > 0.05). However, there was a significant difference between them at 2 months (t = 3.248) and 3 months (t = 5.45; P < 0.01) of treatment (Table 1,Fig. 1).
Table 1.
Comparison of PTSD scores between treatment group and control group before and after treatment (x ± s).
| treatment group (n = 30) | control group (n = 30) | t | P | |
|---|---|---|---|---|
| Before treatment | 49.67 ± 9.46 | 50.37 ± 8.48 | 0.273 | 0.787 |
| 1 month | 46.33 ± 8.84 | 51.03 ± 7.67 | 1.939 | 0.062 |
| 2 months | 42.30 ± 8.12 | 49.83 ± 7.42 | 3.248 | 0.003** |
| 3 months | 37.43 ± 7.27 | 48.2 ± 6.65 | 5.45 | 0.000** |
**P < 0.01.
Fig. 1.
Data expressed as mean ± standard error (SEM).
In the treatment group, the total PTSD score decreased significantly in a stepwise manner before and at 1 month (t = 11.87), 2 months (t = 11.96), and 3 months (t = 11.37) of treatment (P < 0.01). (Table 2,Fig. 2). The total FIM score increased in a stepwise manner at the end of 1-month (T = −10.78), 2-month (T = −7.505), 3-month (T = −7.187) treatments. The difference was statistically significant (P < 0.01). (Table 3,Fig. 2) (see Table 4).
Table 2.
Comparison of PTSD scores before and after treatment in the treatment group (x ± s).
| PTSD (n = 30) | t | P | |
|---|---|---|---|
| Before treatment | 49.67 ± 9.46 | ||
| 1 month | 46.33 ± 8.84 | 11.87 | 0.000** |
| 2 months | 42.30 ± 8.12 | 11.96 | 0.000** |
| 3 months | 37.43 ± 7.27 | 11.37 | 0.000** |
**P < 0.01.
Fig. 2.
Data expressed as mean ± standard error (SEM).
Table 3.
Comparison of FIM scores before and after treatment in the treatment group (x ± s).
| FIM(n = 30) | t | P | |
|---|---|---|---|
| Before treatment | 46.90 ± 24.31 | ||
| 1 month | 63.63 ± 22.90 | −10.78 | 0.000** |
| 2 months | 77.80 ± 21.36 | −7.505 | 0.000** |
| 3 months | 82.27 ± 20.72 | −7.187 | 0.000** |
**P < 0.01.
Table 4.
Comparison of PTSD scores before and after treatment in the control group (x ± s).
| PTSD (n = 30) | t | P | |
|---|---|---|---|
| Before treatment | 50.37 ± 8.48 | ||
| 1 month | 51.03 ± 7.67 | −1.088 | 0.286 |
| 2 months | 49.83 ± 7.42 | 2.226 | 0.034* |
| 3 months | 48.2 ± 6.65 | 3.505 | 0.002** |
*P < 0.05 **P < 0.01.
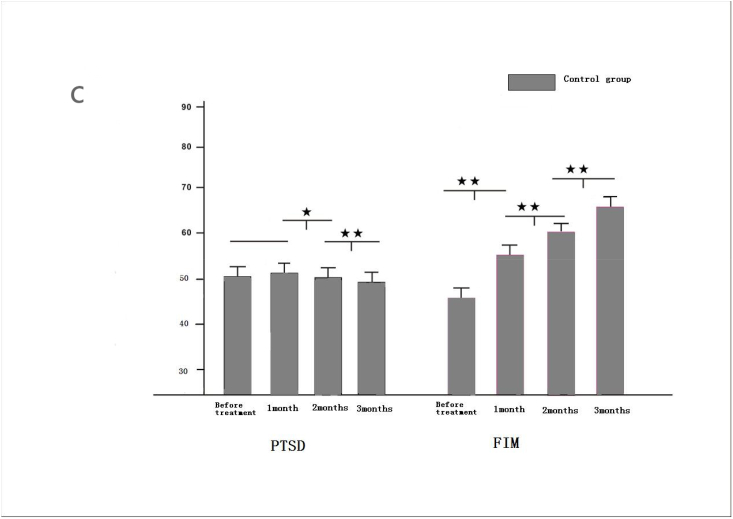
In the control group, there was no significant difference in the total PTSD score before treatment and 1 month after rehabilitation treatment (t = −1.088; P > 0.05). There was a significant difference between the two groups at 2 months (t = 2.226; P < 0.05) and 3 months after treatment compared with that at 1 month after treatment (t = 3.505; P < 0.01).(Table 3,Fig. 3).
Fig. 3.
Data expressed as mean ± standard error (SEM).
The total FIM score in the control group increased in a stepwise manner at the end of 1-month (T = −5.009), 2-month (T = −4.115), 3-month (T = −6.727) treatments. The difference was statistically significant (P < 0.01).(Table 5,Fig. 3).
Table 5.
Comparison of FIM scores before and after treatment in the control group (x ± s).
| FIM(n = 30) | t | P | |
|---|---|---|---|
| Before treatment | 45.10 ± 22.26 | ||
| 1 month | 54.67 ± 26.41 | −5.009 | 0.000** |
| 2 months | 60.67 ± 26.19 | −4.115 | 0.000** |
| 3 months | 66.50 ± 27.56 | −6.727 | 0.000** |
**P < 0.01.
Although the treatment group improved between the time of admission (t = −0.268) and 1 month after treatment (t = −1.248), there was no significant difference in the total FIM score between the treatment and control groups (P > 0.05). After 2 months (t = −2.523) (P < 0.05) and 3 months of treatment (t = −2.876) (P < 0.01), the total FIM score in the treatment group was higher than that in the control group, and there was a significant difference between the two groups (Table 6, Fig. 4) (Table 7).
Table 6.
Comparison of FIM scores before and after treatment between treatment group and control group (x ± s).
| treatment group (n = 30) | control group (n = 30) | t | P | |
|---|---|---|---|---|
| Before treatment | 46.90 ± 24.31 | 45.10 ± 22.26 | −0.268 | 0.791 |
| 1 month | 63.63 ± 22.90 | 54.67 ± 26.41 | −1.248 | 0.222 |
| 2 months | 77.80 ± 21.36 | 60.67 ± 26.19 | −2.523 | 0.017* |
| 3 months | 82.27 ± 20.72 | 66.50 ± 27.56 | −2.876 | 0.007** |
*p < 0.05, **P < 0.01.
Fig. 4.
Data expressed as mean ± standard error (SEM).
Table 7.
Correlation between the modified Barthel index and total PTSD score in the two Groups.
| The modified Barthel index (n = 60) | PTSD (n = 60) | r | |
|---|---|---|---|
| Before treatment | 24.23 ± 22.88 | 50.00 ± 8.94 | −39.7 |
| 1 month | 34.77 ± 23.54 | 48.52 ± 8.53 | −34.2 |
| 2 months | 41.5 ± 23.83 | 45.87 ± 8.60 | −29.5 |
| 3 months | 46.17 ± 24.14 | 42.58 ± 8.72 | −26.7 |
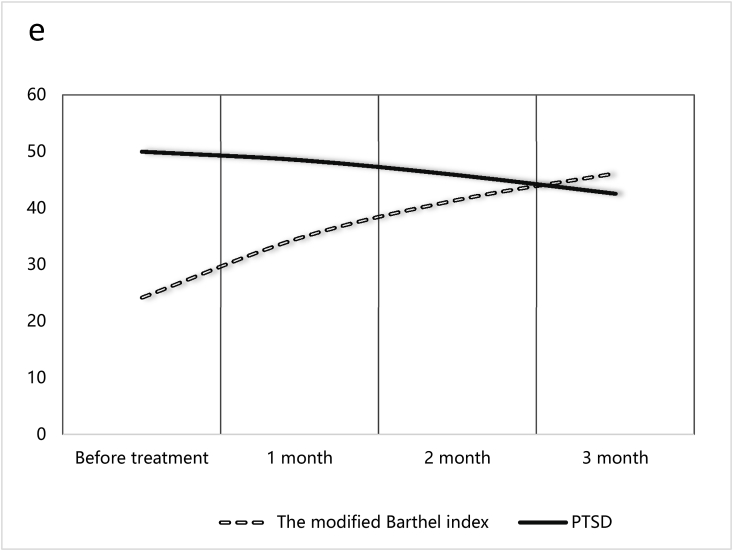
3.2. Correlation between the modified barthel index and total PTSD score in the two groups
Functional Independence Measure (FIM) Scale includes two parts—motor function and cognitive function parts. When we compared FIM with PTSD, the association between FIM AND PTSD was not obviously. For the rigorous scientific research, we use the modified Barthel index instead of the motor function of FIM.The modified Barthel Index positively correlated with FIM scale [9].
There was a significant negative correlation between the two groups before treatment (R = −39.7), 1 month (R = −34.2), 2 months (R = −29.5), and 3 months after treatment (R = −26.7) (Fig. 5).
Fig. 5.
Correlation between Barthel and PTSD scores.
4. Discussion
SCI is one of the most serious body trauma that results in limb dysfunction, defecation disorder, sexual inability, inability to work and perform housework, and varying degrees of loss of self-care ability. It brings great distress to individuals and is a heavy burden to their families. An important aspect of rehabilitation treatment is maximum restoration of impaired functions and abilities. However, in the current medical situation, even if maximum-effort rehabilitation treatment is performed, regardless of the cost, there will still be serious consequences such as limb dysfunction, decreased sensation, defecation disorders, and sexual dysfunction. It results in inability to work normally and affects the ability for self-care and contributes to psychological stress. We searched the impact of stress response on the mental health of SCI patients after trauma, to verify if this impact could hinder the recovery of physical and social functions in SCI patients, and we compared different psychotherapy techniques to find the most effective methods to reduce stress disorder in SCI patients.There are many methods of psychotherapy, such as cognitive behavioral, gestalt, psychoanalytic, and Morita therapies. Morita therapy advocates the acceptance of symptoms as these symptoms cannot be resolved or changed by the patients themselves; this means that patients go about their lives without focusing on the symptoms [10]. For SCI patients, applying this concept can help them face reality and accept past and present facts that cannot be changed; this may help in the recovery from SCIs. However, in reality, SCI is an organic injury, and Morita's idea is not readily accepted by SCI patients. Therefore, we chose ACT to treat psychological problems in SCI patients because this theory is more detailed and specific. It is based on a typical empirical avoidance of symptoms [11] along with cognitive fusion symptoms [11] of PTSD patients. The most effective way involves mindfulness, acceptance, and attention to the present, when patients have physical pain, disability, and psychological avoidance symptoms. Based on this, cognitive dissociation is done to help identify the value of symptoms and help patients define this value; thus, we can assist patients to actively invest in and cooperate with the rehabilitation treatment [12].
Our results showed that the PTSD score in all SCI patients was significantly higher than that in the healthy controls, indicating that SCI patients experienced different degrees of stress. In the treatment group, PTSD scores decreased significantly in the first month after rehabilitation treatment combined with ACT and decreased significantly over time after one month, two months, and three months of treatment. PTSD scores in the treatment group were significantly higher than those in the control group after 2 and 3 months of treatment, indicating that ACT had a positive effect in reducing the stress level of SCI patients. However, total PTSD scores in the control group decreased after 2 and 3 months of treatment, and the reduction in speed and degree of disability was significantly lower than that in the treatment group. Total FIM scores gradually increased with time in the treatment and control groups. From the second month of treatment, the FIM score increased and was significantly higher in the treatment group than in the control group. This was in accordance with the decreased PTSD score. There was no significant correlation between total PTSD and FIM scores, indicating that the improvement in social function in SCI patients was not significant in the early stage of rehabilitation treatment. However, the correlation analysis showed that there was a significant negative correlation between the modified Barthel index [13] and total PTSD score. The above results demonstrate that ACT combined with rehabilitation therapy was effective in reducing PTSD symptoms and improving body function and self-care ability, and played an important role in improving the effect of rehabilitation treatment. Early intervention with ACT psychotherapy among SCI patients was useful in promoting the recovery of body function and self-care ability, and in improving the curative effect of rehabilitation treatment. This research is worth popularizing and applying in general hospitals.
Funding source
This work was supported by Wuhu Bureau of Science and Technology and Anhui Province Wannan Rehabilitation Hospital.Item number 2016hm19.
Acknowledgments
Thanks to my colleagues: Help me collect materials, provide rehabilitation care and treatment.Thanks to my teacher, Dr. Jiangbo Li for instructing me to perfect and revise the article.
References
- 1.Cuccurullo SaraJ. Physical medicine and rehabilitation board review. Musculoskeletal Medicine. 2016;10:551–553. [Google Scholar]
- 2.Li J., Yang M., Yang D. Experts consensus on ‘assessment, treatment and rehabilitation of traumatic spinal cord injury’. Theory and Practice of Rehabilitation in China. 2017;23(3):274–287. [Google Scholar]
- 3.Pupo M.C., Jorge M.R., Schoedl A.F. The accuracy of the Clinician-Administered PTSD Scale(CAPS) to identify PTSD cases in victims of urban violence”. Phychiat Res. 2011;185:157–160. doi: 10.1016/j.psychres.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Flett HeatherM., Delparte JudeJ., Scovil CarolY. Determining pressure injury risk on admission to inpatient spinal cord injury rehabilitation: a comparison of the Functional Independence Measure, Spinal Cord Injury Pressure Ulcer Scale, and Braden scale”. Archives of Physical Medicine and Rehabilitation. 2019;100(10):1881–1887. doi: 10.1016/j.apmr.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Pellatt G.C. Perceptions of the nursing role in spinal cord injury rehabilitation”. British Journal of Nursing. 2003;12(5):292–299. doi: 10.12968/bjon.2003.12.5.11175. [DOI] [PubMed] [Google Scholar]
- 6.Hugues B., Michel L., Kathleen E. Walking after spinal cord injury: evaluation, treatment, and functional recovery. Physical Medicine and Rehabilitation. 1999;80(2):pp225–235. doi: 10.1016/s0003-9993(99)90126-0. [DOI] [PubMed] [Google Scholar]
- 7.Dijkers M.P., Zanca J.M. Factors complicating treatment sessions in spinal cord injury rehabilitation: nature, frequency, and consequences. The American Congress of Rehabilitation Medicine. 2011;10:11–15. doi: 10.1016/j.apmr.2012.11.047. [DOI] [PubMed] [Google Scholar]
- 8.Harris Russ. Act made simple: an easy-to-read primer on acceptance and commitment therapy. New Harbinger. 2009;11(5):54–60. [Google Scholar]
- 9.Gosman-Hedström G., Svensson E. Parallel reliability of the functional independence measure and the Barthel ADL index. Disability and rehabilitation. 2009;6(7):702–715. doi: 10.1080/09638280050191972. [DOI] [PubMed] [Google Scholar]
- 10.Li J.B. vol. 8. Peking University Medical Press; 2019. pp. 86–91. (Analysis of Morita Psychotherapy). [Google Scholar]
- 11.Chen Y., Zhu Z.H. Summarize of Acceptance commitment therapy for post-traumatic stress disorder”. Chinese Journal of Clinical Psychology. 2018;26(1):205–208. [Google Scholar]
- 12.Roush JaredF., Brown SarahL., Mitchell SeanM. Experiential avoidance, cognitive fusion, and suicide ideation among psychiatric inpatients: the role of thwarted interpersonal needs. Psychotherapy Research. 2019;11(4):1–10. doi: 10.1080/10503307.2017.1395923. [DOI] [PubMed] [Google Scholar]
- 13.Hong I., Yoonjeong L., Han H. Application of the Korean version of the modified Barthel index: development of a key form for use in clinical practice”. Hong Kong journal of occupational therapy. 2017;7(6):39–46. doi: 10.1016/j.hkjot.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]