Abstract
Objectives
The COVID-19 pandemic and resulting shelter-in-place orders have profoundly changed the everyday social environment. This study examines the relationship between pain and psychological distress (depression, anxiety, and loneliness) among U.S. adults ages 54 and older during the pandemic. We also test whether use of technology for social purposes moderates the association between pain severity and psychological distress.
Methods
Using cross-sectional data on 1,014 adults ages 54 and older (pain free, n = 637; mild pain, n = 106; moderate pain, n = 227; and severe pain, n = 64) from the 2020 Health and Retirement Study COVID-19 Project (Early, Version 1.0), we conducted regression analyses to test the association between pain severity and psychological outcomes and to assess social technology use frequency as a moderator.
Results
Compared with their pain-free peers, participants with mild-to-moderate pain reported more depressive symptoms and greater loneliness; those with severe pain reported higher levels of depression, anxiety, and loneliness. Social technology use was associated with lower levels of depression and loneliness. However, interaction analyses show that social technology use predicted an increase in depression for individuals with pain but a decrease in depression among pain-free individuals. For anxiety and loneliness, no significant effects of social technology use were observed.
Conclusion
Older adults with pain are at high risk of depression, anxiety, and loneliness during the pandemic. Although social technologies have become a common alternative to face-to-face interactions during the COVID-19 crisis, and overall they can provide mental health benefits, our results suggest that social technologies can be detrimental to psychological well-being among people with pain. These findings can inform technology-based interventions aiming to promote well-being among older adults with pain.
Keywords: Depression, Anxiety, Loneliness, COVID-19, Technology Use for Social Purpose
Introduction
The outbreak of the novel coronavirus disease 2019 (COVID-19) has led to profound social changes in the United States and elsewhere [1, 2], including reduced in-person interactions resulting from social distancing requirements. Before the pandemic, older adults with pain were known to be at higher risk of social isolation and poor psychological well-being than their pain-free peers [3]; it is thus plausible that the changed social circumstances resulting from COVID-19 restrictions exacerbated distress in this population.
The social changes brought on by the pandemic may affect individuals living with pain through at least two pathways [4]. First, people with pain may suffer more intensely from their condition because of reduced access to medical pain management during the pandemic. Second, social distance from others and reduced access to public spaces and social engagement could increase feelings of loneliness and disconnection [5, 6]. Overall, older adults with pain may be quite vulnerable to the negative effects of social changes in the current health crisis.
Technologies, such as computers and mobile devices, offer opportunities to buffer the negative association between pain and psychological well-being. They may increase the resilience of older adults with diverse needs by enabling them to connect to social media, communicate with others, and access telemedicine [7, 8]. Recent research shows that online social participation can reduce the negative impact of pain on the mental well-being of U.S. older adults [9]. It is possible that older adults who do not have access to or do not use social technologies struggle with a double burden of social exclusion, especially during the pandemic [10]. Therefore, researchers have called for greater attention to digital infrastructure access for older adults, who as a group are less likely to obtain high-quality information or services online [10, 11].
In this study, we explore the associations between pain, psychological distress, and social technology use among older adults during the COVID-19 pandemic. Specifically, we analyze whether 1) older adults with pain disproportionately suffer from loneliness, depression, and anxiety during the pandemic, compared with their pain-free counterparts, and 2) whether the use of social technologies moderates the associations between pain status and these outcomes.
Methods
Data
This study used secondary data from the 2020 HRS COVID-19 Project (Early, Version 1.0), part of the ongoing longitudinal Health and Retirement Study (HRS). The COVID-19 module of HRS 2020 surveyed a random subsample of respondents originally assigned to face-to-face interviewing; because of the pandemic, interviews were conducted by telephone. The dataset includes 3,266 respondents, an approximately 25% random sample of the original HRS sample. Two of our key outcomes (anxiety and loneliness) and our moderator (social technology use) were collected in the self-administered Leave-Behind Questionnaire, which was given to a random half sample (n = 1,168) of the 3,266 respondents. We also excluded participants with missing data on the variables of interest, yielding a final analytic sample of 1,014 individuals ages 54 and above.
Measures
We operationalized psychological distress using measures of depression, anxiety, and loneliness. Depression was assessed with the Center for Epidemiological Studies Depression (CES-D) eight-item scale [12], with two items (happy and enjoy life) reverse-coded (Cronbach’s alpha = 0.81). Higher scores indicate more depressive symptoms. Anxiety was assessed with the five-item scale from the Beck Anxiety Inventory [2]. Response options range from 1 (never) to 4 (most of time), with higher scores indicating more severe anxiety. We averaged the ratings of the five items (Cronbach’s alpha = 0.81). Loneliness was assessed with an 11-item scale derived from the Revised UCLA Loneliness Scale [13], with response categories of 1 = often through 3 = hardly ever or never. The loneliness index was created by reverse-coding four items (lack companionship, feel left out, feel isolated, alone) so that higher scores consistently indicate greater loneliness and by averaging the scores across all 11 items (Cronbach’s alpha = 0.88).
Pain severity was assessed with two questions: “Are you often troubled with pain?” and “How bad is the pain most of the time: mild, moderate, or severe?” We combined these items to create a four-category pain variable ranging from 0 = pain free to 3 = severe pain. This measure has been used previously, and through its strong association with functional limitations and mortality, it has been found to have good concurrent and predictive validity [14, 15]. The HRS does not ask follow-up questions to identify the location, cause, or duration of the pain. Questions elsewhere in the survey ask about specific conditions that are likely to be pain producing, such as arthritis, “persistent or troublesome” back pain, or headaches. Among members of our analytic sample reporting any level of pain, the percentages reporting arthritis, back pain, or headache were 33.23%, 27.92%, and 6.32%, respectively. These results suggest that those endorsing pain were likely to have musculoskeletal pain [15, 16]. We also assessed an alternative measure of pain that combined information on pain severity with pain-related disability, to produce three categories: no pain, mild or moderate pain without disability, and severe and/or disabling pain [17]. Results obtained with the alternative pain measure are reported in the supplemental analyses.
Social Technology Use
Previous approaches to assessing technology/Internet use for social purposes have typically focused on specific types of software or hardware used (e.g., e-mail, social networking sites, online video/phone calls, online chatting / instant messaging) [18] or on the social goals of the activity (e.g., connecting with friends, connecting with family, making new connections/friends, sharing photographs/data) [19]. We assessed social technology use by integrating both types of measures, using all available relevant questions in the HRS.
Specifically, we constructed an index of social technology use based on five items: “How often do you use one or more of [your] devices to do any of the following activities? 1) Take or share photos and videos, 2) send or receive instant messages, text messages, or e-mails, 3) access a social network site like Facebook, Twitter, or Instagram, 4) use WhatsApp, Snapchat, or similar apps to network with people, and 5) connect face to face with family and friends using an app (such as FaceTime, Skype).” Response options on each item ranged from 1 = daily to 5 = never. We recoded the data so that 0 equals never and 4 equals daily and then took the maximum score across the five items; higher scores thus indicate more frequent social technology use.
Health controls included chronic conditions (number reported of seven conditions: hypertension, diabetes, non-skin cancer, lung diseases, coronary heart disease, congestive heart failure, stroke) and activity of daily living (ADL) disability (whether or not the respondent was able to perform five common ADL tasks, e.g., dressing, walking, etc.).
Sociodemographic covariates included age, gender, race/ethnicity, education, whether married/partnered, and whether the respondent had at least one living child, as shown in Table 1.
Table 1.
Sample characteristics (N = 1,014; from 2020 HRS COVID-19 project)
| Percentage or Mean (SD), Sample Weight–Adjusted | Percentage or Mean (SD), Unadjusted | n | |
|---|---|---|---|
| Depressive symptoms (range: 0–8) | 0.94 (1.56) | 1.11 (1.75) | 1,000 |
| Anxiety index (range: 1–4) | 1.48 (0.52) | 1.52 (0.56) | 1,014 |
| Loneliness index (range: 1–3) | 1.51 (0.44) | 1.51 (0.44) | 1,006 |
| Pain severity | |||
| No pain (ref.) | 61.79 | 60.85 | 617 |
| Mild pain | 10.77 | 10.45 | 106 |
| Moderate pain | 21.53 | 22.39 | 227 |
| Severe pain | 5.91 | 6.31 | 64 |
| Social technology use (range: 0–4) | 3.41 (0.91) | 3.36 (1.15) | 1,014 |
| Number of chronic conditions (range: 0–7) | 1.42 (1.22) | 1.47 (1.22) | 1,014 |
| ADL-disability (range: 0–5) | 0.43 (0.77) | 0.48 (0.81) | 1,014 |
| Age, y (range: 54–101) | 67.07 (7.34) | 66.98 (7.91) | 1,014 |
| Sex (female = 1) | 52.28 | 56.31 | 517 |
| Race/ethnicity | |||
| Non-Hispanic White (ref.) | 80.84 | 64.30 | 652 |
| Non-Hispanic Black | 8.60 | 18.64 | 189 |
| Hispanic | 6.13 | 12.52 | 127 |
| Non-Hispanic other | 4.42 | 4.54 | 46 |
| Marital status (married = 1) | 68.12 | 63.31 | 643 |
| Have any living child | 86.19 | 86.79 | 880 |
| Education | |||
| No degree | 7.27 | 10.65 | 108 |
| High school degree (ref.) | 57.20 | 54.64 | 554 |
| Four-year college or above | 35.53 | 34.71 | 352 |
Analytic Strategy
After providing descriptive statistics for all key variables in our analyses, we report the results of a series of regressions. Because the number of depressive symptoms is a count variable, we used negative binomial models for that outcome; for the anxiety and loneliness indexes, we used ordinary least square regression analyses. The first set of models tests the additive effects of all independent variables on the three psychological distress outcomes (Models 1, 3, and 5). The second set of models tests the moderating effects of social technology use on the association between pain and the three outcomes (Models 2, 4, and 6). All models use the COVID-19 project preliminary sampling weights and specifying the cluster, stratification, and sample error correction to produce the weighted results, following prior recommendations [20].
Results
Descriptive Statistics
Table 1 shows descriptive statistics with sampling weight adjusted and unadjusted for the analytical sample (N = 1,014). The average number of depressive symptoms was 0.94 (range: 0 to 8). The average score on the anxiety index was 1.48 (range: 1–4), and the average score on the loneliness index was 1.51 (range: 1–3). Our analytical sample consisted of 617 individuals who reported no pain, 106 who reported mild pain, and 227 who reported moderate pain, while the remaining 64 reported severe pain. The weighted percentages of respondents with mild, moderate, and severe pain were 11%, 22%, and 6%, respectively. The frequency of the social technology use was 3.41, indicating an average use between several times per week and daily.
Regression Results
Table 2 shows the results of the regression models (all of which include all control variables). In Model 1, individuals with moderate and severe pain reported significantly more depressive symptoms than pain-free respondents; the higher the level of pain, the higher the average number of depressive symptoms. More frequent social technology use was significantly associated with fewer depressive symptoms (B = –0.12, P = 0.03).
Table 2.
Regression results of depressive symptoms, anxiety, and loneliness (from 2020 HRS COVID-19 project; weighted)
| Depressive Symptoms Negative Binomial Regression |
Anxiety Index OLS Regression |
Loneliness Index OLS Regression |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mode 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |||||||
| Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | |
| Pain severity (ref. no pain) | ||||||||||||
| Mild pain | 0.29 | 0.19 | 0.85** | 0.42 | −0.05 | 0.06 | 0.06 | 0.11 | 0.11* | 0.06 | 0.14* | 0.08 |
| Moderate pain | 0.69**** | 0.16 | 1.16**** | 0.25 | 0.07 | 0.05 | −0.08 | 0.09 | 0.09* | 0.05 | 0.11 | 0.08 |
| Severe pain | 0.85*** | 0.25 | 1.64**** | 0.43 | 0.26** | 0.11 | 0.44** | 0.19 | 0.16* | 0.10 | 0.27* | 0.15 |
| Social technology usea | −0.12** | 0.06 | −0.29**** | 0.07 | −0.04 | 0.02 | −0.03 | 0.03 | −0.08**** | 0.02 | −0.08**** | 0.02 |
| Pain severity× social technology usea | ||||||||||||
| Mild× social technology use | 0.35* | 0.19 | 0.07 | 0.06 | 0.02 | 0.06 | ||||||
| Moderate× social technology use | 0.31** | 0.14 | −0.10 | 0.07 | 0.01 | 0.05 | ||||||
| Severe× social technology use | 0.52*** | 0.19 | 0.12 | 0.10 | 0.07 | 0.07 | ||||||
| Number of chronic conditions | 0.14*** | 0.05 | 0.15*** | 0.05 | 0.05*** | 0.02 | 0.05*** | 0.02 | 0.05*** | 0.02 | 0.05*** | 0.02 |
| ADL-disability | 0.31**** | 0.06 | 0.31**** | 0.06 | 0.08** | 0.03 | 0.08*** | 0.03 | 0.04 | 0.02 | 0.04* | 0.02 |
| Age, y | 0.00 | 0.01 | 0.00 | 0.01 | 0.00* | 0.00 | 0.00 | 0.00 | −0.01*** | 0.00 | −0.01*** | 0.00 |
| Sex (female = 1) | 0.22* | 0.13 | 0.23* | 0.13 | 0.01 | 0.04 | 0.02 | 0.04 | −0.07** | 0.03 | −0.07** | 0.03 |
| Race/ethnicity (ref. White) | ||||||||||||
| Non-Hispanic Black | 0.13 | 0.11 | 0.14 | 0.11 | 0.01 | 0.05 | 0.02 | 0.04 | −0.05 | 0.05 | −0.06 | 0.05 |
| Hispanic | 0.51** | 0.20 | 0.45** | 0.20 | 0.09 | 0.11 | 0.09 | 0.11 | 0.02 | 0.06 | 0.01 | 0.06 |
| Non-Hispanic other | 0.17 | 0.26 | 0.21 | 0.26 | −0.10 | 0.07 | −0.10 | 0.07 | 0.05 | 0.08 | 0.05 | 0.08 |
| Marital status (married = 1) | −0.31** | 0.12 | −0.33*** | 0.12 | 0.00 | 0.04 | 0.01 | 0.04 | −0.10*** | 0.03 | −0.10*** | 0.03 |
| Have any living child (yes = 1) | −0.13 | 0.18 | −0.16 | 0.18 | −0.02 | 0.06 | −0.03 | 0.06 | −0.11** | 0.05 | −0.11** | 0.05 |
| Education (ref. high school) | ||||||||||||
| No degree | −0.03 | 0.16 | −0.02 | 0.15 | 0.02 | 0.06 | 0.04 | 0.06 | −0.06 | 0.06 | −0.06 | 0.07 |
| Four-year college or above | −0.10 | 0.15 | −0.10 | 0.15 | −0.02 | 0.04 | −0.02 | 0.04 | −0.05 | 0.04 | −0.05 | 0.04 |
| Intercept | −0.72 | 0.62 | −0.98 | 0.62 | 1.63**** | 0.17 | 1.59**** | 0.17 | 2.02**** | 0.16 | 2.00**** | 0.16 |
Social technology use is mean centered. OLS = Ordinary Least Squares.
P < 0.1,
P < 0.05,
P < 0.01,
P < 0.001.
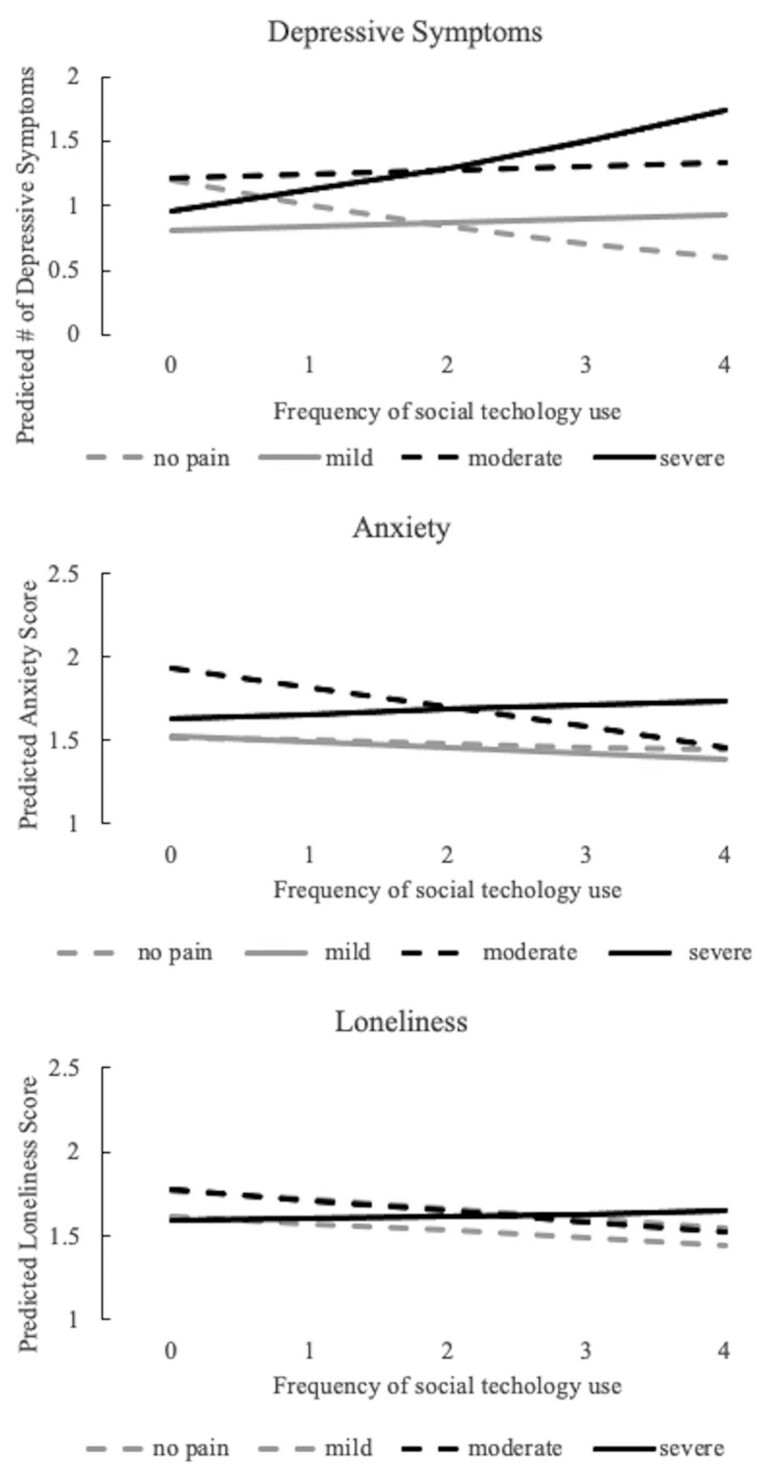
In Model 2, we tested whether using social technology moderates the association between pain and depressive symptomatology. Rather than reducing the depression disparity, technology use widened it; that is, more frequent social technology use predicted a lower number of depressive symptoms among pain-free individuals but a greater number among those with pain (see Figure 1, top panel).
Figure 1.
Predicted depressive symptoms, anxiety, and loneliness by pain severity and social technology use.
In Models 3 and 4, OLS regression results show that people with severe pain reported significantly higher levels of anxiety than their pain-free peers (B = 0.26, P < 0.05). Social technology use was not significantly associated with reduced anxiety in Model 3. In Model 4, the interaction terms were not statistically significant; although individuals with moderate pain showed steeper reductions in anxiety than other groups as they increased their social technology use, it was not statistically significant (see Figure 1, middle panel).
OLS regression results for loneliness are presented in Models 5 and 6. Compared with their pain-free counterparts, older adults with any level of pain reported marginally higher levels of loneliness (P < 0.10). More frequent social technology use significantly predicted lower levels of loneliness (B = –0.08, P < 0.05). In Model 6, the interaction terms were not statistically significant—i.e., the benefits of social technology use were of similar magnitude across all pain groups (Figure 1, bottom panel).
In addition to the associations among pain, social technology use, and psychological distress, we also found that health problems and other sociodemographic variables were associated with the three outcomes. First, more chronic conditions were associated with higher levels of depression, anxiety, and loneliness, whereas ADL disability was associated with higher levels of depression and anxiety but not loneliness. Moreover, age was negatively associated with loneliness but not with depression and anxiety. Women reported less loneliness than did men. There were no racial differences observed among the three outcomes, with one exception: Hispanic participants reported higher levels of depression than did White respondents. Married individuals reported lower levels of depression and loneliness than did unmarried respondents. Older adults with children also reported lower levels of loneliness. There was no observed difference between education and the three outcomes.
Supplemental Analyses
We performed several sensitivity analyses to test the robustness of our results. We first tested an alternative measure of pain that combined pain severity with information on pain-related disability to yield a three-category variable: no pain, mild or moderate pain without disability, and severe and/or disabling pain [17]. The findings were almost identical to the results shown here in which pain severity was used alone. We also tested an alternative measure of social technology use by using the average score across five items rather than the maximum score. The results were similar to the results shown here, except that the interaction coefficient of moderate pain and social technology use in the model with depression as the outcome was marginally significant (P < 0.10). We also compared the effects of two types of Internet use—real-time video conferencing apps (e.g., FaceTime, Zoom, Skype) vs asynchronous social networking apps (e.g., Facebook, Twitter)—and found that the results for using video conferencing apps mirrored the results shown here, but those for using social networking apps were not associated with significant changes in the outcomes, nor did their use moderate the effect of pain on psychological well-being. Thus, the effects of the social technology index on psychological distress were driven mainly by using real-time apps such as FaceTime and Zoom.
We then tested all the sociodemographic variables as moderators to assess whether the associations between social technology use and psychological well-being varied across age, gender, race/ethnicity, marital status, parenthood status, and education groups. We did not find any significant interactions for these variables. Finally, we controlled for the frequency of participating in vigorous, moderate, or mild physical activities; the results were similar to the results reported. All supplemental analyses are available upon request.
Discussion
This study used a nationally representative sample of adults ages 54 and older to assess whether pain status (no, mild, moderate, or severe chronic pain) was associated with psychological distress early in the COVID-19 pandemic (May 2020). We also sought to determine whether social technology use moderated this relationship. We found that, compared with their pain-free peers, respondents with moderate or severe pain reported significantly more depressive symptoms; those with severe pain reported significantly higher levels of anxiety. The main effect of social technology use in the full sample was beneficial; i.e., it predicted lower levels of depression and loneliness. This is consistent with research on Internet use among older adults during the pre-COVID period [9, 21, 22].
As a moderator, however, social technology use had a complex relationship with the pain–distress association, which depended on the particular outcome examined. Rather than buffering the negative association between pain severity and depression, social technology use amplified it: That is, more frequent technology use predicted an increase in depressive symptoms for those with pain but a decrease for those without. We found no significant interactions, however, between technology use, pain, and levels of anxiety or loneliness.
It is not surprising that older adults with pain reported greater psychological distress than their pain-free counterparts during the pandemic. Such associations have been extensively documented even before the COVID-19 outbreak, and there are ample theoretical reasons to expect this association to persist or strengthen during the early stages of the pandemic, through multiple pathways suggested by Karos and colleagues [4]. For example, social distancing, reduced access to public space, and limited social engagement could all exacerbate pain sufferers’ loneliness and social disconnection. Moreover, stay-at-home orders can increase exposure to overly protective behaviors and relationship stress among pain sufferers and their family members. Older adults with pain might also suffer from reduced access to high-quality pain management, which could increase levels of anxiety and depression.
However, our finding that more frequent social technology use predicted greater depressive symptoms in people with pain was unexpected and counterintuitive. Our findings differ from prior research, which found that online social participation was protective against pain-related depression. However, this earlier research was based on data collected before technologies such as Zoom were widely used, from a sample of older adults (ages 65 and older), with dichotomous measures of pain and Internet use [9]. Our findings may differ because of the different time period, sample characteristics, and measures. It is possible that during the pandemic, many or most in-person interactions were replaced by rather than supplemented with online social interactions. In-person activities may be more distracting or may involve physical activity (e.g., taking walks) that could help reduce perceived pain.
In addition, it is possible that greater technology use led to repetitive strain injuries (e.g., carpal tunnel syndrome) or screen fatigue, which may be particularly deleterious and heighten levels of depressive symptoms for people already experiencing chronic pain. In-person interactions often occur informally and in various settings, e.g., cafés, restaurants, or parks, where people sit or walk together. However, exclusively using computers or smartphones for social interaction could lead to excess use of keyboards and screens. Such overuse may cause hand injuries or spinal pain from poor posture. Recent research has found that misuse or overuse of technology devices was common during the pandemic and could cause such problems [23].
However, because our data are cross-sectional, we cannot rule out the possibility that people with higher levels of depression, especially those with pain, used technology to reach out to others more frequently. It is possible that persons with severe pain/depression were also individuals who were most likely to restrict their activity levels during the pandemic and turn to social technology use, whereas pain-free individuals may have been less likely to do so. In addition, individuals with moderate-to-severe levels of pain and those with greater depressive symptoms are more likely to experience sleep disturbance (vs pain-free individuals) and therefore may spend more time on the Internet because of this disturbance (e.g., spending time in bed on the Internet). Perhaps most importantly, the specific characteristics of online socialization may differ as a function of pain/depression status. People with pain/depression may be likely to reach out to other similar individuals (colleagues with pain; chronic pain support groups), leading to interactions that reinforce their illness experience. In this scenario, the online communication occurring may contribute to the persistence of pain/depressive symptoms.
There are several important clinical implications of this study’s findings. Our results reinforce the critical importance of screening frequently for depression and anxiety in individuals with pain during the pandemic. Providers for patients with pain/depression may wish to ask their patients to describe how they are coping during the pandemic and whether use of online tools is a strategy they are using to cope; if so, clinicians should be aware that for individuals with pain, there may be unexpected negative effects of certain types of Internet use.
This study has several limitations. First, given the cross-sectional nature of the data, we cannot compare levels of psychological distress at different time points. As vaccination rates increase and social restrictions diminish, psychological well-being for older adults may improve. The cross-sectional data also prevent us from making strong causal arguments; our findings are presented as suggestive associations. We encourage future researchers to track psychological distress among older adults with varying levels of pain and pain-related disability over the course of the pandemic.
In addition, we examined only social uses of the Internet or mobile devices; future research could further explore the role of the Internet for other purposes, such as information-seeking (e.g., finding health information) or instrumental purposes (e.g., work, business, banking, shopping). Moreover, as mentioned earlier, HRS does not ask follow-up questions to identify the location, cause, or duration of pain. We therefore encourage future research to obtain data with detailed pain measures to examine the associations among pain, social technology use, and psychological well-being. Last, because of data limitations, we are not able to control for the geographic location of participants, such as rural vs urban, or for neighborhood characteristics, which could affect the accessibility of high-quality pain care and technology use.
We encourage researchers to further investigate the relationship between social technology use and psychological distress among adults with chronic pain. Our results highlight the need for future studies to not only assess the benefits associated with social technology use in persons with pain but also to evaluate the potential unintended negative consequences. If the mechanisms leading to harmful effects can be identified, these negative outcomes of social technology use could potentially be prevented. Investigators should keep potentially negative effects in mind when designing technology-based interventions for pain patients. Future studies should assess whether existing pain coping strategy tools are appropriate for use in times of a pandemic and in particular whether they reduce or exacerbate psychological distress in the Internet era. Finally, clinicians providing medical care via telemedicine or other technologies should not assume that social technology is an innocuous or beneficial substitute for in-person interactions, at least among pain patients.
In conclusion, this study contributes to our understanding of psychological distress among older adults with pain during the COVID-19 pandemic and tests whether social technology use moderates the association between pain severity and several salient mental health symptoms. We find that compared with pain-free peers, individuals with pain reported more depressive and anxiety symptoms and higher levels of loneliness. Although more frequent social technology use reduces psychological distress on average, it appears to amplify depressive symptoms among pain sufferers. Given that social technology use represents an increasingly important resource for delivering interventions to individuals with a variety of health problems, understanding the social technology use experience of adults living with various types and levels of pain, as well as those living with other chronic conditions, constitutes an important topic for researchers, health practitioners, and policymakers.
Authors’ Contributions
Yulin Yang performed all statistical analyses and drafted the manuscript.
Hanna Grol-Prokopczyk, M. Carrington Reid, and Karl Pillemer supervised the data analysis and contributed to writing and revising the manuscript.
Funding sources: Dr. Reid is supported by grants from the National Institute on Aging of the National Institutes of Health (P30AGO22845, K24AGO53462).
Dr. Grol-Prokopczyk is supported by a grant from the National Institute on Aging of the National Institutes of Health (R01AG065351).
Dr. Pillemer is supported by a grant from the National Institute on Aging of the National Institutes of Health (P30AGO22845).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of interest: The authors report no conflicts of interest.
References
- 1. Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020;7(6):547–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Van Bavel JJ, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 2020;4(5):460–71. [DOI] [PubMed] [Google Scholar]
- 3. Smith T. “On their own”: Social isolation, loneliness and chronic musculoskeletal pain in older adults. Qual Ageing Older Adults 2017;18(2):87–92. [Google Scholar]
- 4. Karos K, McParland JL, Bunzli S, et al. The social threats of COVID-19 for people with chronic pain. Pain 2020;161(10):2229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berg-Weger M, Morley JE. Loneliness and social isolation in older adults during the Covid-19 pandemic: Implications for gerontological social work. J Nutr Health Aging 2020;24(5):456–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hwang T-J, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatrics 2020;32(10):1217–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eccleston C, Blyth FM, Dear BF, et al. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020;161(5):889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pillemer K, Czaja SJ, Reid MC. Caring for chronically ill older adults: A view over the last 75 years. J Gerontol Ser B 2020;75(10):2165–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ang S, Chen T-Y. Going online to stay connected: Online social participation buffers the relationship between pain and depression. J Gerontol Ser B 2019;74(6):1020–31. [DOI] [PubMed] [Google Scholar]
- 10. Seifert A, Cotten SR, Xie B. A double burden of exclusion? Digital and social exclusion of older adults in times of COVID-19. J Gerontol Ser B 2021;76(3):e99–e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Xie B, Charness N, Fingerman K, et al. When going digital becomes a necessity: Ensuring older adults’ needs for information, services, and social inclusion during COVID-19. J Aging Soc Policy 2020;32(4-5):460–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Measur 1977;1(3):385–401. [Google Scholar]
- 13. Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J Personal Assess 1996;66(1):20–40. [DOI] [PubMed] [Google Scholar]
- 14. Covinsky KE, Lindquist K, Dunlop DD, Yelin E. Pain, functional limitations, and aging. J Am Geriatr Soc 2009;57(9):1556–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grol-Prokopczyk H. Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. Pain 2017;158(2):313–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rice ASC, Smith BH, Blyth FM. Pain and the global burden of disease. Pain 2016;157(4):791–6. [DOI] [PubMed] [Google Scholar]
- 17. Zimmer Z, Zajacova A. Persistent, consistent, and extensive: The trend of increasing pain prevalence in older Americans. J Gerontol Ser B 2020;75(2):436–47. [DOI] [PubMed] [Google Scholar]
- 18. Chopik WJ. The benefits of social technology use among older adults are mediated by reduced loneliness. Cyberpsychol Behav Soc Network 2016;19(9):551–6. doi: 10.1089/cyber.2016.0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Szabo A, Allen J, Stephens C, Alpass F. Longitudinal analysis of the relationship between purposes of internet use and well-being among older adults. Gerontologist 2019;59(1):58–68. [DOI] [PubMed] [Google Scholar]
- 20. Fisher GG, Ryan LH. Overview of the health and retirement study and introduction to the special issue. Work Aging Retire 2018;4(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cotten SR, Ford G, Ford S, Hale TM. Internet use and depression among retired older adults in the United States: A longitudinal analysis. J Gerontol Ser B Psychol Sci Soc Sci 2014;69(5):763–71. [DOI] [PubMed] [Google Scholar]
- 22. Yu K, Wu S, Chi I. Internet use and loneliness of older adults over time: The mediating effect of social contact. J Gerontol Ser B 2021;76(3):541–50. [DOI] [PubMed] [Google Scholar]
- 23. Iyengar K, Upadhyaya GK, Vaishya R, Jain V. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr 2020;14(5):733–7. [DOI] [PMC free article] [PubMed] [Google Scholar]