Abstract
Background
The COVID-19 pandemic resulted in a rapid and expansive roll out of telehealth applications as a mode of intervention delivery. The effectiveness of this model of care is currently unclear.
Objective
A cross-sectional observational study evaluating the Irish physiotherapist’s experience of telehealth.
Method
Irish Physiotherapists completed an online survey, distributed by the Irish Society of Chartered Physiotherapists (ISCP), exploring considerations and barriers to commencing telehealth, advantages and disadvantages to telehealth, overall experience of telehealth, and their opinion on the future of telehealth. A descriptive approach and conceptual content analysis were used to analysis the data to derive determinants for the continuation of telehealth.
Results
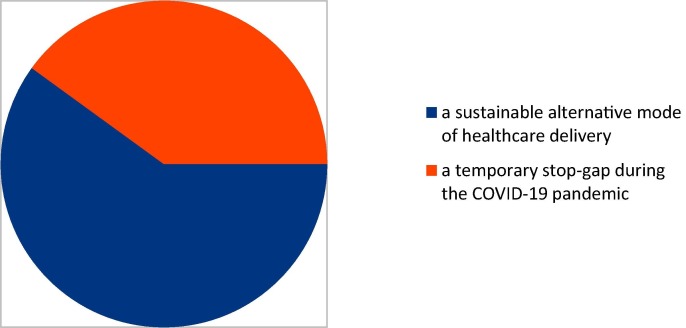
In total, 205 physiotherapists completed the survey. Seventy-eight per cent were female. Participant's mean age range was 36 to 45 years with 17 years of physiotherapy experience. Eighty-three per cent had no experience with telehealth pre COVID-19. Considerations to commencing telehealth included service user's suitability, adequate technical and organisational resources, physiotherapist's professional conduct, physiotherapist's skills and COVID-19 restrictions. No outstanding barrier to telehealth was identified. Respondents identify that telehealth offered a reduction in travel time for the service user (82%), offer flexibility in the delivery of physiotherapy (81%) and avoid contact with a potential COVID-19 spreader (92%). The limited scope of the physical examination (86%) via telehealth is the significant disadvantage. Telehealth is considered a temporary stop-gap during the COVID-19 pandemic by forty per cent of physiotherapists while sixty per cent consider telehealth as a sustainable alternative mode of health care delivery.
Conclusion
At present, health care providers have not universally accepted telehealth as a mode of health care delivery. Our study’s findings identify key areas to address to encourage acceptance.
Keywords: Telehealth, COVID-19, Physiotherapist, Healthcare delivery, Blended care
1. Introduction
There was a rapid and expansive roll out of telehealth during the COVID-19 pandemic. It was the only mode of intervention available to physiotherapy during the periods of strictest public restrictions. Pre pandemic the widespread uptake of telehealth was slow [1], [2]. Digital health care is supported globally with many countries formally recognising the value of using digital modes of care delivery [3]. The effectiveness of this model of care is unclear in comparison to face-to-face care [4].
The term digital practice, telehealth, telerehabilitation and telemedicine can be used interchangeably. There is no agreed terminology [5]. Telehealth will be used here. Telehealth is the distribution of health-related services via electronic and telecommunication technologies [6] such as internet, wireless, satellite and telephones [7]. It allows long-distance patient and clinician contact, care, advice, reminders, education, intervention, monitoring, and remote admissions [8], [9].
In the Republic of Ireland, during the COVID-19 pandemic, there were periods of nil and limited access to out-patient physiotherapy clinics. Physiotherapists introduced telehealth to continue physiotherapy provision, distance-learning, meetings and presentations. This was a relatively new work method and included telephone consultations, virtual consultations and teleconferencing, delivered in real-time/live streaming. Different applications/programs/platforms were used. Hybrid/blended telehealth was then adopted which combines face-to-face consultations and telehealth services [10].
Some organisations have considered their approach to telehealth since the onset of COVID-19, while others rapidly adopted telehealth services [11]. The experience of the practitioner and the patient will shift the views of this service delivery method [11]. A pre COVID-19 study of service providers’ pre-use perceptions of telehealth, for the management of service users with chronic musculoskeletal conditions, suggest that service provider’s acceptance is the most influential factor for the success of telehealth [12]. Irish physiotherapists involved in palliative care suggest that telehealth was used in limited capacities during COVID-19, mostly by outpatient physiotherapists [13]. Telehealth has been shown to reduce non-attendance rates and improve wait times within an Irish emergency department physiotherapy clinic [14].
Currently there is no published literature on the Irish physiotherapist’s experience of telehealth during the specific period of the COVID-19 pandemic. This study aims to explore the Irish physiotherapist’s perspective of telehealth during this time. It questions the ISCP members on their telehealth usage, the considerations and barriers to commencing telehealth, the overall experience and the future of telehealth in physiotherapy.
2. Methods
A cross-sectional observational design was adopted using an originally designed anonymous online survey.
Qualitative and quantitative studies on telehealth [12], [15] aided formulation of a survey. Quantitative and qualitative data were collected. Questions included consent, gender, age, years working as a physiotherapist and area of physiotherapy speciality during 2020. Respondents rated their I.T. skills, commented on their prior use of telehealth and the purpose of the utilised telehealth modalities. They listed factors considered prior to commencing telehealth, rated the barriers they encountered, and identified the advantages and disadvantages listed. They commented on their overall experience of telehealth and the viability of telehealth for the future (see Appendix 1).
The survey’s value was established by two peers. They ensured the questions were clear, concise, of suitable language, without bias, avoidance of negative items where possible and did not assign causality. It was pilot tested on four participants and revised. It was conducted anonymously on www.smartsurvey.co.uk. Physiotherapists were invited to participate via email invitation and this was distributed to the ISCP membership by the ISCP office administrator. The ISCP was chosen as the sample population as it is the professional body for the physiotherapy profession in Ireland. Eligible physiotherapists were those who engaged in telehealth during 2020. Email invitation included the links to the participant information leaflet and survey, time frame for return of survey and consent information. It was available for three weeks.
A qualitative descriptive approach to analysis was taken [16], [17] to determine characteristics of the survey population. The majority of the data were categorical, continuous or ordinal level of measurement. Multiple answers could be chosen for barriers, advantages and disadvantage to telehealth. Valid answers were summed up over all participants and then ranked. Conceptual content analysis was applied to the free text answers in the open-ended questions. The answers were read, themes identified with flexibility to add categories, then coded for the frequency of a theme and rules developed to distinguish between themes [18]. There is transparency in the conduction and reporting of this analysis, and examples are provided to give insight into the process of analysis and interpretation. Data were edited interactively and responses analysed for completeness, duplication, outliers and logical consistency. The STROBE cross sectional checklist was used when writing our report. It is an internationally recognised checklist to strengthen the reporting of observational studies [19].
3. Results
The survey was emailed to 2,587 ISCP members. The number of members who engage in telehealth is unknown. A sample size of 193 respondents was required to achieve an 85% confidence level with a margin of error of 5%. In total 205 eligible participants completed the survey. Seventy-eight per cent (n = 159) of respondents were female and twenty-two per cent (n = 46) were male. The average age range was 36 and 45 years. The years of physiotherapy experience ranged from 'current student' to 44 years with a mean of 17 years. Musculoskeletal, orthopaedic and rheumatology physiotherapists were the highest responders (37%, n = 75), followed by private practice physiotherapists (26%, n = 54). Forty-four per cent (n = 91) rated their I.T. skills as average prior to COVID-19, forty-five per cent (n = 93) rated their skills as above average and ten per cent (n = 21) rated their skills as below average (see Table 1 ).
Table 1.
Survey participants' sociodemographic data (n = 205).
| % | n | |
|---|---|---|
| Gender | ||
| male | 22.44 (46) | |
| female | 77.56 (159) | |
| Age | ||
| 18–20 years | 0 | (0) |
| 21–29 years | 13.66 | (28) |
| 30–39 years | 35.12 | (72) |
| 40–49 years | 32.20 | (66) |
| 50–59 years | 15.12 | (31) |
| 60–69 years | 3.90 | (8) |
| 70 or older | 0 | (0) |
| mean minimum age = 36 years | ||
| mean maximum age = 45 years | ||
| Years working as a physiotherapist | ||
| mean = 16.92 | ||
| missing = 1 | ||
| Physiotherapy speciality | ||
| Adult Physical and Sensory Disabilities | 1.46 | (3) |
| Musculoskeletal, Orthopaedic and Rheumatology Outpatients | 36.59 | (75) |
| Paediatrics | 13.66 | (28) |
| Primary Care | 17.56 | (36) |
| Neurology and Gerontology | 9.76 | (20) |
| Respiratory | 6.83 | (14) |
| Private Practice | 26.34 | (54) |
| Women's and Men's health | 6.83 | (14) |
| Other: | ||
| Management | 1.46 | (3) |
| Education | 1.95 | (4) |
| Palliative Care, oncology, lymphoedema | 2.44 | (5) |
| Cardiac | 0.49 | (1) |
| Student | 0.49 | (1) |
| Other speciality areas mentioned and included in the above areas are; pain clinic, hand therapy plastics, paediatric primary care, paediatric pelvic health, first contact UK based, intellectual disabilities, musculoskeletal triage, redeployment to COVID-19 test centre and assessment hub. | ||
| Self rated I.T. Literacy | ||
| Far above average | 4.88 | (10) |
| Above average | 40.49 | (83) |
| Average | 44.39 | (91) |
| Below average | 9.76 | (20) |
| Far below average | 0.49 | (1) |
Seventeen per cent (n = 34) of respondents reported using telehealth prior to COVID-19 while eighty-three per cent (n = 171) reported no prior experience. Eighty-two per cent (n = 168) reported using the telephone, eighty-six per cent (n = 177) used live streaming platforms and forty-two per cent (n = 87) used mobile applications. Mobile applications and live streaming platforms used were Zoom (60%, n = 122), Attend Anywhere (42%, n = 87), Cisco WebEx (31%, n = 64), Whatsapp (31%, n = 64) and Microsoft teams (29%, n = 60). Thirty-five other programs were mentioned, usage varied between 0.5% (n = 1) to 7% (n = 15). These programs and the telephone were used by eighty-nine per cent (n = 183) for physiotherapy assessment and eighty-eight per cent (n = 180) for physiotherapy treatment (advice, education, rehabilitation, exercise prescription and review). Eighty per cent (n = 164) of physiotherapists attended meetings and presentations, while sixty-three per cent (n = 129) reported using them for distance learning. Eleven per cent (n = 22) use telehealth for other purposes, of note four per cent (n = 9) used it for conducting classes (see Table 2 ).
Table 2.
Telehealth usage.
| % | (n) | |
|---|---|---|
| Use of telehealth prior to COVID-19 pandemic | ||
| Yes - I did use telehealth | 16.59 | (34) |
| No previous use of telehealth | 83.41 | (171) |
| Telehealth modalities used during the COVID-19 pandemic | ||
| telephone | 81.95 | (168) |
| live streaming/real time platforms | 86.34 | (177) |
| mobile applications | 42.44 | (87) |
| Other: paypal, email, exercise videos uploaded to hospital website | 1.46 | (3) |
| The purpose of utilising telehealth | ||
| Physiotherapy Assessment | 89.27 | (183) |
| Physiotherapy Treatment | 87.80 | (180) |
| Distance-learning | 62.93 | (129) |
| Meetings and/or presentations with colleagues | 80.00 | (164) |
| Other: Classes (exercise, pilates, antenatal, group education) | 10.73 | (9) |
| Recording health promotion information | (1) | |
| Musculoskeletal triage | (2) | |
| Multidisciplinary clinics | (1) | |
| Liaising with service user's family | (1) | |
| Teaching and training others | (2) | |
| Interviewing | (1) | |
| Consulting | (1) | |
| Virtual trauma clinic | (2) | |
| Research | (2) | |
| The future of telehealth | ||
| a temporary stop-gap during the COVID-19 pandemic | 40.49 | (83) |
| a sustainable alternative mode of healthcare delivery | 59.51 | (122) |
3.1. Considerations to commencing telehealth
This free text commentary asked respondents to list the factors they considered prior to commencing telehealth. Fifty answers were evaluated and categorised according to similar theme/word/meaning. Four themes emerged; service user suitability, adequate resources, physiotherapist’s professional conduct and physiotherapist’s skills. These answers were re-evaluated to ensure accuracy of categorisation. The identified themes guided the remaining responses. ‘Adequate resources’ was subdivided into two, ‘technical resources and considerations’ and ‘organisational resources and considerations’. One further theme was added; ‘COVID-19 restrictions’. 197 respondents answered this question. The frequency and the percentages refer to the number of respondents who communicated that particular word/phrase or text.
Theme 1: Service user suitability; respondents identified that the service user is selected for their suitability to engage with telehealth. Criteria identified include capacity to engage, cognitive ability, health literacy, medical history, visual/hearing/communication impairments, difficulty with mobility and dexterity, possible compliance and anxiety (14%, n = 28). The severity and nature of the presenting symptoms (11%, n = 22), service user's willingness to partake in telehealth (10%, n = 19) and service user's age (9%, n = 18) was specifically mentioned. For example, age was considered “a predictive indicator of how well they would manage a telehealth session” and consideration for “elderly patients’ ability to use technology”. Words stated for severity and nature of presenting symptoms were urgent referrals, pathology of the condition and affected body part. Twenty-seven per cent (n = 54) considered digital literacy but it was unspecified if this was the digital literacy of the service user, physiotherapist or both.
Theme 2: Technical resources and technical considerations; respondents listed sufficient internet connectivity (31%, n = 61), access to adequate technology hardware (smart phone, tablet, desktop computer, laptop, webcam, headset) (30%, n = 59), access to adequate technology software (application access, internet access) (18%, n = 35) and ease of use (15%, n = 29) as prerequisites for the physiotherapist and the service user. Approved platforms and software security (9%, n = 17), functionality of the telehealth platforms (7%, n = 13) and IT services support (4%, n = 8) were considered. Platform functions specified were ability to video call, conduct meeting and record sessions, an available exercise library and electronic notes, and suitability for group intervention.
Theme 3: Organisational resources and considerations; availability of a suitable environment for the physiotherapist and the service user (lighting, private space, acoustics, camera positioning, picture quality) were considered by twenty per cent (n = 39). Nine per cent (n = 17) contemplated the cost for both parties with one service user reporting receipt of local enterprise office funding while others debated “how much should I charge?”. Resources available pre session (x-ray, assessment and treatment equipment) and appropriate preparedness were listed by five per cent (n = 9).
Theme 4: Physiotherapist's professional conduct; Clinical governance (safeguarding of the client, adverse event management, risk assessment and patient satisfaction) were mentioned by twenty per cent (n = 40). Factors considered were informed consent (18%, n = 36), privacy and confidentiality (18%, n = 36), GDPR and ethical consideration (17%, n = 34), documentation/policies, procedures and guidelines/pathways/statistics/audit (13%, n = 25) and chaperone/assistant/carer for client (6%, n = 12).
Theme 5: Physiotherapist's skills; respondents deliberated over the necessity of telehealth (4%, n = 7) and the goals of intervention (3%, n = 5), e.g. “what would the physiotherapist and the client gain” from telehealth? They considered the quality of their assessment (10%, n = 20), how best to modifying their assessment, treatment and clinical reasoning (7%, n = 13), their ability to out rule serious pathologies (3%, n = 5), methods of education (4%, n = 8), their communication skills (3%, n = 5), applicable modalities to use (2%, n = 4) and devised patient information leaflets (5%, n = 9). Five per cent up skilled before commencing telehealth (n = 10).
Theme 6: COVID-19 restrictions; nine per cent felt telehealth needed embracing secondary to infection prevention and control of COVID-19 (n = 17) stating “needs must”, sustainability of a priority service (2%, n = 3) and to maintain meaningful contact (2%, n = 3).
3.2. Barriers
204 physiotherapists rated the nine listed barriers in order of importance or ticked 'not applicable'. An average of 158 respondents gave a rating to a barrier. An average of 11 respondents perceived a barrier as not applicable. No conclusive barrier was identified. Over fifteen per cent rated availability of resources to support telehealth (23%, n = 38) and a perceived depersonalisation of care (15%, n = 24) as their most significant barrier. The availability of workspace was considered the most important barrier by fifteen per cent (n = 27) while another fourteen per cent (n = 25) did not recognise this as a barrier. Again, the availability of technical support was considered the principal barrier by sixteen per cent (n = 31) while another eleven per cent (n = 22) did not consider it a barrier. Full details are available on request.
3.3. Advantages and disadvantages
Respondents marked the identifiable advantages and all respondents answered. Over eighty per cent identifies that telehealth prevents contact with a potential COVID-19 spreader (93%), offers flexibility in physiotherapy delivery (81%) and reduces travel for the service user (82%). Over sixty-five per cent recognise it is useful for continuous professional development (77%), it is efficient for meetings (66%) and it modernises our approach to communication (66%) (see Table 3 ).
Table 3.
Advantages of telehealth.
| % | (n) | |
|---|---|---|
| avoiding contact with a potential COVID-19 spreader | 92.68 | (190) |
| reduction in travel for the service user | 82.44 | (169) |
| offers flexibility in how physiotherapy is delivered | 80.98 | (166) |
| useful for continuing your professional development | 77.07 | (158) |
| more efficient for conducting and attending meetings | 66.34 | (136) |
| modernises our approach to communication | 65.85 | (135) |
| improved access to healthcare | 49.27 | (101) |
| the rollout of telehealth was quick | 35.12 | (72) |
| reduces 'Did Not Attend' rate | 34.63 | (71) |
| an adequate subjective and objective assessment can be completed | 30.73 | (63) |
| good service user's satisfaction | 30.24 | (62) |
| adequate to out rule serious pathologies | 21.95 | (45) |
| less time consuming than conventional interventions | 20.49 | (42) |
| good job satisfaction for the physiotherapist | 18.54 | (38) |
| Other (available on request) | 18.54 | (38) |
All respondents identified at least one disadvantage. The outstanding disadvantage identified, by eighty-six per cent of physiotherapists, is the limited scope for a physical examination. Over fifty-six per cent report it reduces job satisfaction for the physiotherapist (57%) and there is poor computer literacy among service users (59%) (see Table 4 ).
Table 4.
Disadvantages of telehealth.
| % | (n) | |
|---|---|---|
| limited scope for the physical examination | 86.34 | (177) |
| computer literacy of the service users is poor | 59.02 | (121) |
| reduces job satisfaction for the physiotherapist | 56.59 | (116) |
| the technology will fail regularly | 48.78 | (100) |
| inadequate ability to out rule serious pathologies | 47.80 | (98) |
| more time consuming than conventional interventions | 46.83 | (96) |
| difficult to build a rapport with the service user | 45.37 | (93) |
| difficult to prescribe a specialised treatment plan | 40.98 | (84) |
| exhausting | 40.00 | (82) |
| reduces service user satisfaction | 38.05 | (78) |
| difficult to alleviate service user's concerns regarding their health | 30.24 | (62) |
| difficult to communicate “bad news” to service users | 29.27 | (60) |
| difficult to ensure privacy and confidentiality | 19.51 | (40) |
| overwhelming | 15.61 | (32) |
| increases the 'Did Not Attend' rate | 11.22 | (23) |
| difficult to obtain consent | 8.29 | (17) |
| the rollout of telehealth was quick | 3.41 | (7) |
| Other: included specific elements of the physical examination (n = 10) | 14.63 | (30) |
| others available on request (n = 20) |
3.4. Overall experience
Forty per cent (n = 83) of physiotherapists consider telehealth as a temporary stop-gap during the COVID-19 pandemic while sixty per cent (n = 122) consider telehealth as a sustainable alternative mode of health care delivery (see Fig. 1 ). Respondents commented on their experience. Responses were divided into the above two categories and coded by terms used. The frequency and the percentages refer to the number of respondents who communicated that particular word/phrase or text.
Physiotherapists who consider telehealth as a temporary stop-gap
Fig. 1.
Perceived future of telehealth.
Theme 1: Positive commentary; they felt face-to-face contact was preferential (31%, n = 26) or a blended approach (7%, n = 6) should be adopted. Some felt telehealth was positive (22%, n = 18) or adequate (14%, n = 12) or it was useful during the COVID-19 restrictions (18%, n = 15), e.g. “it is a good addition to keep in contact with my caseload”. It is a good long-term addition to services allowing access remotely and to specialised services (16%, n = 13), useful for screening, review appointments, exercise progression and classes (13%, n = 11), excellent for meetings and continuous professional development (11%, n = 9).
Theme 2: Negative commentary; some felt it was negative (12%, n = 10). It is difficult to complete a thorough assessment (22%, n = 18), less personal (14%, n = 12) and time consuming (10%, n = 8). Respondents felt “we should remember the value of interpersonal interaction in healthcare” and “I can see many potential logistical benefits but for me the joy is meeting clients in person”. It is stressful, frustrating (10%, n = 8) and exhausting (8%, n = 7) with comments of “telehealth fatigue is real”. There are regular technology issues (8%, n = 7), difficult to diagnose accurately and educate (5%, n = 4) and difficult to provide an adequate treatment (6%, n = 5). It can “create a health inequality in an area with poor socioeconomics” due to a digital divide (1%, n = 1). Specific difficulty within paediatric physiotherapy services was observed; “it is difficult for parents who had just received a child’s diagnosis and this was their first experience of therapy so they had no marker of what therapy should look like or what could be achieved with good handling/positioning. They also needed more support and discussion about their child’s needs and how they were developing. Also the child, with limited concentration and attention, constantly moved or wished to play with the screen”.
Those who felt it was sustainable alternative mode of health care delivery
Theme 1: Positive commentary; commented that telehealth was a positive experience (52%, n = 64) or a mixed experience (15%, n = 18), “it was surprising how well we adapted”. A blended approach was considered preferential by twenty-five per cent (n = 30) with adequate training, IT and managerial support (3%, n = 4). “It has encouraged the necessary funding to upgrade ICT (information communication technology) infrastructures within organisations”. It was effective during the pandemic (12%, n = 15) and service users embraced it (4%, n = 5). It is a great adjunct for future physiotherapy intervention (14%, n = 17), convenient (8%, n = 10), good for progressing treatment (5%, n = 6), empowers service user's self-management (4%, n = 5) and improves access (4%, n = 5) especially with vast catchment areas. Physiotherapists reported a great learning curve (5%, n = 6), “we were catapulted into using certain modes and our up skilling happened as a natural consequence of that”. It is excellent for meetings and continuous professional development (5%, n = 6).
Theme 2: Negative commentary; However it took time to become accustomed (5%, n = 6) and its success is dependent on the client suitability and clinical presentation (22%, n = 27), respondents were concerned about “missing subtle cues for red flags”. Technology issues are on-going (22%, n = 27), it is difficult to do a thorough assessment (11%, n = 14), it’s time consuming (9%, n = 11) and fatiguing (6%, n = 7). “Good to have as an alternative but I found it a frustrating experience as a manual therapist”.
4. Discussion
Attitudes and determinants towards telehealth are presented in the results. The merit of this research is validated as no previous telehealth experience is reported by the majority which is consistent with the literature reporting an international slow uptake of telehealth prior to 2020 [1], [2]. The live streaming platforms have been embraced which is a positive adoption of the newer technologies. Few smart phone applications are currently endorsed by the Irish National Health Service provider and this may explain the lesser use of this technology.
The availability of equipment, technology failures, patient confidentiality [20], inadequate technology training and regulatory constraints [21] have all been suggested in the literature as facilitators or barriers to commencing telehealth. Our respondents agreed. Suitable service users need to be selected for telehealth and it cannot be offered generically. Certain selection criterion is identified. However procedure and protocols should be devised to ensure equitable access to services. Telehealth delivery should be flexible and tailored towards service user's needs [18] and abilities as concerns were expressed in relation to digital literacy and client suitability. Variation in technical supports exist, however technology specific barriers can be overcome through training and change-management techniques [22]. Respondents considered their professional conduct. Service providers need to be proactive in comprehending current laws and regulations to ensure compliance with an ever changing environment and avoid legal consequences [23]. As telehealth expands, additional medico legal concerns will arise and will need to be addressed. A contingency plan should be established before commencing telehealth when a patient is not located on the clinical site [23]. The availability of a suitable and appropriate environment should be considered locally as every work location offers different space.
The overwhelming advantages include flexibility, reduction in travel for the service user, safety during the COVID-19 pandemic, modernisation, conducting meetings and for the continuing professional development of the physiotherapist. The overwhelming concern is the execution of a sufficient physical examination. Telehealth requires the clinician to depend on the service user to provide information that may be normally derived from the physical examination [24] and a greater provision of consultation time is required for telehealth [19]. The service users' computer literacy may be poor and technology may fail [20], [23]. In future this may create a digital divide between areas with different educational opportunities and varying internet speeds.
The physiotherapist's perspective of the longevity of telehealth was inconclusive with a 60/40 percentage split. The literature suggests that the most influential factor for the success of telehealth is service provider's acceptance [18], [25], [26], [27]. Half of the physiotherapists, who considered telehealth as a sustainable alternative, described it as a positive experience and it should supplement face-to-face intervention. However they are concerned about on-going technology issues and a service user should be selectively chosen. On the contrary, physiotherapists who considered telehealth as a temporary stop gap did not consider blended care as a future option. They reported less job satisfaction while using telehealth. The experience of the practitioner and the patient will shift views of this service delivery method [11].
Although the considerations, barriers, advantages and disadvantages mirror those reported in the literature, it was important to consider these from the Irish perspective, physiotherapist's perspective and during a global pandemic. Physiotherapy practice is characterised by reflective behaviour and systematic clinical reasoning, both contributing to and underpinning a problem-solving approach to patient-centric care [28]. We propose that these characteristics are similar to many other medical disciplines. This research will provide information to key stakeholders with governance over telehealth roll out and protocol. Physiotherapy management locally and nationally will primarily benefit. Irish physiotherapy healthcare is delivered publicly and privately and this research may be transferable internationally and to other health service disciplines. It will enable further planning for telehealth within the physiotherapy service as the pandemic and public movement restrictions continue and cease.
4.1. Limitations
The study sample size was limited and it is not known if saturation was achieved. A selection bias by respondents needs to be considered as the majority of contributors were from private practice and musculoskeletal, orthopaedic and rheumatology physiotherapy services. A volunteer bias may exist also; those with moderate opinions of telehealth may be less likely to participate. We did not evaluate the quantity of real time contact with telehealth and this may have implications for the attitudes towards it and therefore generalisation of our findings needs to be applied carefully.
5. Conclusion
The service provider should be involved in the early stages of design and implementation of telehealth to ensure clinical acceptance and long term continuation [25]. It is proposed that telehealth is most effective when utilised in combination with face-to-face care, with suitable service users, when adequate resources, supports and training are available. Digital availability and literacy will need to be investigated to ensure equitable access to healthcare services. Cyclical evaluation of the healthcare provider's perspective is warranted as telehealth is still in the early stage of implementation. Further research is required to investigate the service user’s experience of telehealth. Evaluation of clinical, economic and service utilisation outcomes need to be investigated also.
Ethical approval
Ethical approval was obtained from the Health Service Executive's North East Area Research Ethics Committee.
Funding
This research didn’t receive specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The researchers acknowledge the support of peers who completed the survey, read draft copies of the survey and the paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijmedinf.2021.104613.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Tanriverdi H., Iacono C.S. Diffusion of Telemedicine: a knowledge barrier perspective. Telemed. J. 1999;5(3):223–244. doi: 10.1089/107830299311989. [DOI] [PubMed] [Google Scholar]
- 2.Wade V.A., Taylor A.D., Kidd M.R., Carati C. Transitioning a home telehealth project into a sustainable, large-scale service: a qualitative study. BMC Health Serv. Res. 2016;16 doi: 10.1186/s12913-016-1436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Confederation of Physical Therapy, March 2020. Report of the WCPT/INPTRA Digital Physical Therapy Practice Task Force. https://world.physio/sites/default/files/2020-06/WCPT-INPTRA-Digital-Physical-Therapy-Practice-Task-force-March2020.pdf.
- 4.Laver K.E., Adey-Wakeling Z., Crotty M., Lannin N.A., George S., Sherrington C. Telerehabilitation services for stroke. Cochrane Database System. Rev. 2020;(1) doi: 10.1002/14651858.CD010255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bashshur R., Shannon G., Krupinski E., Grigsby J. The taxonomy of telemedicine. Telemed eHealth. 2011;17(6):484–494. doi: 10.1089/tmj.2011.0103. [DOI] [PubMed] [Google Scholar]
- 6.The Health Resources and Services Administration. 17/10/21. What is Telehealth? Last reviewed September 2021. https://www.hrsa.gov/rural-health/telehealth/what-is-telehealth.
- 7.Achenbach Samantha J. Telemedicine: benefits, challenges, and its great potential. Health Law Policy Brief. 2020;14(1) Article 2. Available at: https://digitalcommons.wcl.american.edu/hlp/vol14/iss1/2. [Google Scholar]
- 8.Masson M. Benefits of TED Talks. Can. Family Phys. 2014;60(12):1080. PMID: 25500595; PMCID: PMC4264800. [PMC free article] [PubMed] [Google Scholar]
- 9.Shaw D.K. Overview of telehealth and its application to cardiopulmonary physical therapy. Cardiopulmonary Phys. Therapy J. 2009;20(2):13–18. PMID: 20467533; PMCID: PMC2845264. [PMC free article] [PubMed] [Google Scholar]
- 10.HealthIT.gov. Last reviewed on April 15, 2019. What tyes of telehealth services can I offer? https://www.healthit.gov/faq/what-types-telehealth-services-can-i-offer.
- 11.Cottrell M.A., Russell T. Telerehabilitation for musculoskeletal physiotherapy. Musculoskeletal Sci. Practice. 2020;48 doi: 10.1016/j.msksp.2020.102193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cottrell M.A., Hill A.J., O’Leary S.P., Raymer M.E., Russell T.G. Service provider perceptions of telerehabilitation as an additional service delivery option within an Australian neurosurgical and orthopaedic physiotherapy screening clinic: a qualitative study. Musculoskelet. Sci. Pract. 2017 Dec;32:7–16. doi: 10.1016/j.msksp.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Drouin J.S., Chigbo N.N., Newstead A.H. Physiotherapist adaptations to cancer, HIV/AIDS, and hospice and palliative care on the COVID-19 Era: a global perspective paper. J. Rehabil Oncol. 2020 doi: 10.1097/01.REO.0000000000000231. [DOI] [Google Scholar]
- 14.Kelly M., Higgins A., Murphy A., et al. A telephone assessment and advice service within an ED physiotherapy clinic: a single-site quality improvement cohort study. Arch Physiother. 2021;11:4. doi: 10.1186/s40945-020-00098-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waschkau A., Flagel K., Goetz K., Steinhauser J. Evaluation of attitudes towards telemedicine as a basis for successful implementation: a cross-sectional survey among postgraduate trainees in family medicine in Germany. Z. Evid. Fortbild. Qual. Gesundh. Wesn (ZEFQ) 2020;156-157:75–81. doi: 10.1016/j.zefq.2020.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Sandelowski M. Focus on research methods-whatever happened to qualitative description? Res. Nurs. Health. 2000;23(4):334–340. doi: 10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 17.Milne J., Oberle K. Enhancing rigor in qualitative description: a case study. J. Wound Ostomy Continence Nurs. 2005;32(6):413–420. doi: 10.1097/00152192-200511000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Columbia Universit Mailman School of Public Health 2019 (accessed 9th August 2021). www.publichealth.columbia.edu/research/population-health-methods/content-analysis.
- 19.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandebroucke J.P. The Strengthening the Reporing of Oservational Studies in Epidemiology (STROBE) Statement: guideline for reporting observational studies. BMJ. 2007;335:806. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simpson R., Robinson L. Rehabilitation after critical illness in people with COVID-19 Infection. Am. J. Phys. Med. Rehabil. 2020;99(6):470–474. doi: 10.1097/PHM.0000000000001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee A.C. COVID-19 and the advancement of digital physical therapist practice and telehealth. Phys. Ther. 2020;100(7):1054–1057. doi: 10.1093/ptj/pzaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scott Kruse C., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howard I.M., Kaufman M.S. Telehealth applications for outpatients with neuromuscular or musculoskeletal disorders. Muscle Nerve. 2018;58(4):475–485. doi: 10.1002/mus.26115. [DOI] [PubMed] [Google Scholar]
- 24.Hinman R.S., Nelligan R.K., Bennell K.L., Delany C. “Sounds a Bit Crazy, But It Was Almost More Personal:” A Qualitative Study of Patient and Clinician Experiences of Physical Therapist-Prescribed Exercise For Knee Osteoarthritis Via Skype. Arthritis Care Res. (Hoboken) 2017;69(12):1834–1844. doi: 10.1002/acr.23218. [DOI] [PubMed] [Google Scholar]
- 25.Brewster L., Mountain G., Wessels B., Kelly C., Hawley M. Factors affecting front line staff acceptance of telehealth technologies: a mixed-method systematic review. J. Adv. Nurs. 2014;70(1):21–33. doi: 10.1111/jan.12196. [DOI] [PubMed] [Google Scholar]
- 26.Whitten P.S., Mackert M.S. Addressing telehealth's foremost barrier: provider as initial gatekeeper. Int. J. Technol. Assess. Health Care. 2005;21(4):517–521. doi: 10.1017/S0266462305050725. [DOI] [PubMed] [Google Scholar]
- 27.Wade V.A., Eliott J.A., Hiller J.E. Clinician acceptance is the key factor for sustainable telehealth services. Qual. Health Res. 2014;24(5):682–694. doi: 10.1177/1049732314528809. [DOI] [PubMed] [Google Scholar]
- 28.Physiopedia 2021. 23/09/2021. Physiotherapy introduction www.physio-pedia.com/Physiotherapy_/_Physical_Therapy.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.