Abstract
Objectives:
Health-care workers (HCW) exposed to COVID-19 are at risk of experiencing psychological distress. Although several cross-sectional studies have been carried out, a longitudinal perspective is needed to better understand the evolution of psychological distress indicators within this population. The objectives of this study were to assess the evolution of psychological distress and to identify psychological distress trajectories of Canadian HCW during and after the first wave of COVID-19.
Method:
This prospective cohort study was conducted from May 8 to September 4, 2020, and includes a volunteer sample of 373 HCW. Symptoms of post-traumatic disorder, anxiety, and depression were assessed using the Post-Traumatic Stress Disorder Checklist for Diagnostic and Statistical Manual of Mental Disorders fifth edition (PCL-5), the Generalized Anxiety Disorder-7, and the Patient Health Questionnaire-9. Descriptive statistics were used to illustrate the evolution of psychological distress indicators, whereas latent class analysis was carried out to identify trajectories.
Results:
During and after the first wave of COVID-19, the rates of clinical mental health symptoms among our sample varied between 6.2% and 22.2% for post-traumatic stress, 10.1% and 29.9% for depression, and 7.3% and 26.9% for anxiety. Finally, 4 trajectories were identified: recovered (18.77%), resilient (65.95%), subchronic (7.24%), and delayed (8.04%).
Conclusion:
The longitudinal nature of our study and the scarcity of our data are unique among existing studies on psychological distress of HCW in COVID-19 context and allow us to contextualize prior transversal data on the topic. Although our data illustrated an optimistic picture in showing that the majority of HCW follow a resilience trajectory, it is still important to focus our attention on those who present psychological distress. Implementing preventive mental health interventions in our health-care institutions that may prevent chronic distress is imperative. Further studies need to be done to identify predictors that may help to characterize these trajectories.
Keywords: COVID-19, health-care workers, psychological distress, post-traumatic, stress, anxiety, depression
Abstract
Objectifs:
Les travailleurs de la santé (TLS) exposés à la COVID-19 sont à risque d’éprouver une détresse psychologique. Bien que plusieurs études transversales aient été menées, il faut une perspective longitudinale pour mieux comprendre l’évolution des indicateurs de la détresse psychologique dans cette population. Les objectifs de la présente étude étaient d’évaluer l’évolution de la détresse psychologique et d’identifier les trajectoires de la détresse psychologique des TLS canadiens durant et après la première vague de la COVID-19.
Méthode:
La présente étude de cohorte prospective a été menée du 8 mai au 4 septembre 2020 et comporte un échantillon volontaire de 373 TLS. Des symptômes de trouble post-traumatique, d’anxiété et de dépression ont été évalués à l’aide de la Liste de contrôle du TSPT pour le DSM-5 (PCL-5), du trouble d’anxiété généralisée-7 (GAD-7), et du questionnaire sur la santé du patient-9 (PHQ-9). Des statistiques descriptives ont servi à illustrer l’évolution des indicateurs de la détresse psychologique alors qu’une analyse de structure latente a été menée pour identifier les trajectoires.
Résultats:
Durant et après la première vague de la COVID-19, les taux des symptômes cliniques de santé mentale au sein de notre échantillon variaient entre 6,2% et 22,2% pour le stress post-traumatique, 10,1% et 29,9% pour la dépression et 7,3% et 26,9% pour l’anxiété. Finalement, quatre trajectoires ont été identifiées: rétabli (18,77%), résilient (65,95%), sous-chronique (7,24%) et retardé (8,04%)
Conclusion:
La nature longitudinale de notre étude et la rareté de nos données sont uniques au sein des études existantes sur la détresse psychologique des TLS dans le contexte de la COVID-19 et permettent de contextualiser les données transversales antérieures sur ce sujet. Bien que nos données aient esquissé une image optimiste en montrant que la majorité des TLS suivent une trajectoire résiliente, il demeure important de centrer notre attention sur ceux qui présentent une détresse psychologique. Il est impératif de mettre en œuvre des interventions de santé mentale préventives dans nos institutions de santé qui peuvent prévenir la détresse chronique. D’autres études sont nécessaires afin d’identifier les prédicteurs qui peuvent contribuer à caractériser ces trajectoires.
Introduction
The COVID-19 virus (SARS-COV-2) reached North America in March 2020. At the time of writing this article (April 2021), Canada has tallied over 1,194,989 confirmed cases, causing 24,065 deaths. 1 Several elements of this unprecedented situation have put the general population at risk of experiencing psychological distress related to fear of infection, quarantine, social isolation, financial insecurities, 2 –6 and so on. Due to the nature of their professional role, health-care workers (HCW) could be even more at risk of experiencing psychological distress. Indeed, HCW are more likely to be in contact with infected patients and to experience job-related stress (workplace reorganization, learning and application of new protocols, and working extra hours). 7 Psychological distress is defined as a set of painful mental and health reactions, often estimated by self-reported measures of post-traumatic stress (PTS), anxiety, and depression. 8,9
As such, 4 literature reviews and meta-analyses showed that a high proportion of HCW were experiencing psychological distress after the first wave of COVID-19. 10 –13 For example, an early Chinese study reported high rates of anxiety (46%), depression (44%), insomnia (29%), and overall psychological problems (57%) in a HCW sample, 2 months after the outbreak. 14 Similar results were found in Italy with 37% of HCW presenting symptoms of PTS above the clinical cut-off, 71% showed clinical levels of anxiety, and 27% had symptoms of depression. 15 Finally, 1 review extracted pooled prevalence among 13 studies (n = 33,062) and reported prevalence of 23.21% for anxiety, 22.8% for depression, and 34.32% for insomnia in HCW. 12
Yet, these studies were cross-sectional and came mostly from Asian or European countries. 10 –13 Furthermore, it is well-documented that human reactions to a stressor or a potential traumatic situation vary widely, ranging from a state of resilience to the development of chronic psychopathology. 16 –19 Longitudinal data are thus needed to understand the evolution of psychological distress experienced by HCW in North America. For this reason, this study aims to assess the different trajectories of psychological reactions in HCW during and after the first wave of COVID-19. These findings will allow a deeper understanding of the evolution of emotional reactions after a disaster such as a pandemic and subsequently offer tailored support to prevent the emergence of mental health problems for workers facing adversity and distress.
As such, the objectives of the study are to (1) explore the evolution of psychological distress of Canadian HCW during and after the first wave of COVID-19 and (2) identify trajectories of psychological distress of these HCW using latent class analysis.
Methods
Study Design
Data of this prospective cohort study were collected through a mobile application during and after the first wave of COVID-19 in the province of Quebec, Canada, between May 8, 2020, and September 4, 2020. The period of the first wave has been set by the Institute of public health expertise and reference centre to be between February 23, 2020, and July 11, 2020. 20 The research team adapted the Ethica app, by integrating our 3 main questionnaires and other relevant questions. Ethica is being used in a variety of research projects worldwide (North America, Europe, and Australia), using both subjective (survey) and objective data (via smartphone sensors). 21
Participants were asked to fill several questionnaires through the mobile application on a weekly basis. Data collection was anonymous, confidential, and on a voluntary basis. The research ethics board of the Centre de recherche du Centre hospitalier de l’Université de Montréal approved the research project. Written consent of every participant was obtained before their participation. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines. 22
Three health-care institutions in the province of Quebec participated in the study, 2 in Montreal and 1 in Quebec City. The research team began by contacting research coordinators in every clinical setting. The communication services then distributed promotional material through various platforms to reach all employees. Interested HCW transmitted their consent (either through a web form or by directly emailing the research coordinator). After the reception of the consent form, sociodemographic information, and professional information from participants, instructions for installing the mobile application were sent to them to start data collection.
Study Population
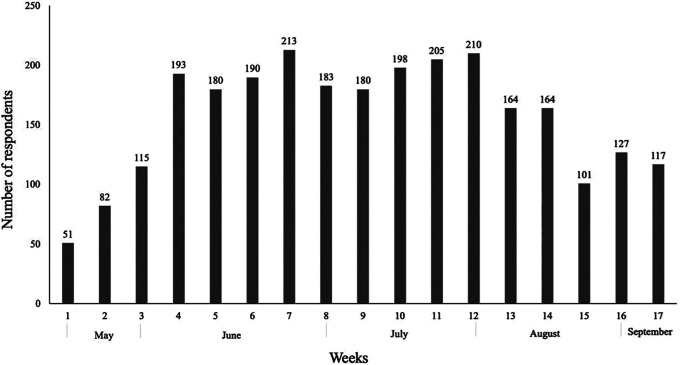
A total of 373 participants from 3 health centres in the province of Quebec in Canada participated in the study, but not all HCW replied to the questionnaires every week. Thereby, the number of respondents per week varies. No participants answered more than 12 times, with 39.94% of HCW answering10 times and more, 28.69% between 5 and 9 times, and a remaining 31.37% answering less than 5 times. Figure 1 shows the number of participants who completed our questionnaires weekly.
Figure 1.
Number of participants who completed questionnaires weekly.
Our sample included HCW from different sectors of health and social services (hospitals [71%], long-term-care hospitals [8%], local community services centres [11%], and unknown [10%]). All workers were invited to participate in the study regardless of the position they held within their establishment. A cessation of work for a reason unrelated to COVID-19 at the time of recruitment was considered as an exclusion criterion.
Measurements and Covariates
The mobile application used for data collection included questions about psychological distress which were quantified through 3 mental health indicators: (1) PTS, (2) anxiety, and (3) depression. We measured these indicators through the French version of the following standardized scales: the short version of Post-Traumatic Stress Disorder Checklist for Diagnostic and Statistical Manual of Mental Disorders, fifth edition (8 items; PCL-5); 23 the General Anxiety Disorder-7 (7 items; GAD-7), 24 and the Patient Health Questionnaire (9 items; PHQ-9). 25 The results were interpreted according to the following clinical cut-off scores: 13 for PCL-5, 10 for GAD-7, and 11 for PHQ-9. For each measure, the look-back period was 7 days.
Participants completed this self-monitoring questionnaire each week throughout the duration of the project. If participant’s score exceeds the clinical threshold, a message appeared at the end of the questionnaire to encourage them to contact help resources. Shared thoughts of death or self-hurting were conducted to a list of resources to contact. At the same time, the research coordinator received an email message, and HCW were contacted by email in the following days. If someone did not respond to the email in the following days, we contacted them by phone. We analyzed data every week, and weekly global reports on well-being of the workers were sent to the high management of the participating institutions.
Statistical Analysis
Data analyses were performed from October to November 2020. We conducted analysis in 3 stages. First, we used descriptive statistics to illustrate the evolution of the symptoms at several time-points. We calculated the percentage of HCW exceeding the clinical cut-offs on the PTS, Anxiety, and Depression Scales for each week. Second, we performed data analysis with R Version 4.0.3, 26 using the latent process mixed model for multivariate markers (MULTLCMM) package 27 to derive psychological functioning trajectories. The number of trajectories was determined using integrated completed likelihood (ICL) Bayesian information criterion (BIC), 28 which combines 2 criteria to ensure a balance between entropy, and the BIC, measuring the fit of the model. No data imputing nor removing was needed since MULTLCMM handled incomplete data in using all observations to compute full-information maximum likelihood parameter estimates. Finally, to ensure that the profile of the participant who answered frequently did not differ from the ones who had missing data, we ran t-test. Doing so, we tested to see whether HCW who responded less than 5 times had different mean baseline scores from those who answered 6 times or more. There was no significant difference between groups for our 3 outcomes (P > 0.05).
Results
Demographic Characteristics
A total of 373 HCW participated in this study. Most participants were women (87.5%) and were aged 18 to 64 years, with a mean (SD) age of 38.69 (9.73). The mean (SD) years of experience was 11.81 (8.91). All participants lived in urban areas and worked in one of the 3 Canadian health-care institutions participating in the project.
Evolution of Symptoms of Post-traumatic Disorder, Anxiety, and Depression
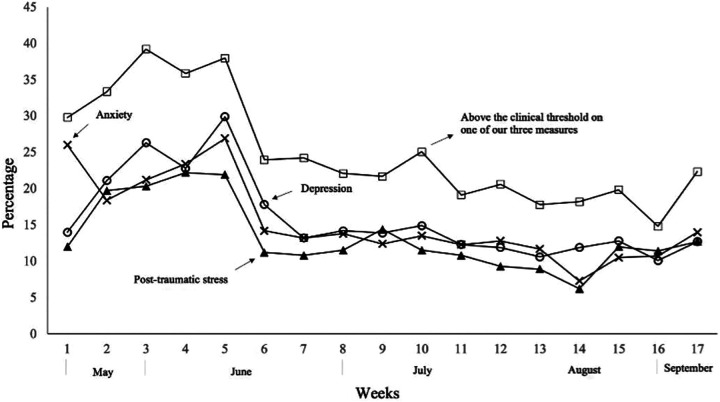
Figure 2 shows descriptive data regarding the percentage of participants exceeding the clinical cut-offs between May 8 and September 4, 2020. Between 14.8% and 39.2% of our sample were above the clinical threshold on one of our 3 measures (PLC-5, GAD-7, and PHQ-9) for this period. The percentages of participants who showed clinical levels of symptoms varied between 6.2% and 22.2% for PTS, 7.3% and 26.9% for anxiety, and 10.1% and 29.9% for depression. Figure 2 shows an increasing trend from weeks 1 to 5, reaching the highest percentage of participants (PCL-5 21.9%, GAD-7 26.9%, and PHQ-9 29.9%) exceeding the clinical cut-offs at week 5 (June 8 to 14, 2020). The graph shows a gradual decrease for our 3 indicators from weeks 5 to 7 and a more stable trend for weeks 7 to 14 with a percentage of HCW exceeding the clinical threshold on our 3 indicators varying between 6% and 15%. Finally, the percentage of HCW experiencing clinical symptoms of PTS, anxiety, and depression increased from weeks 14 to 17.
Figure 2.
Percentage of participants exceeding the clinical threshold.
Psychological Functioning Trajectories
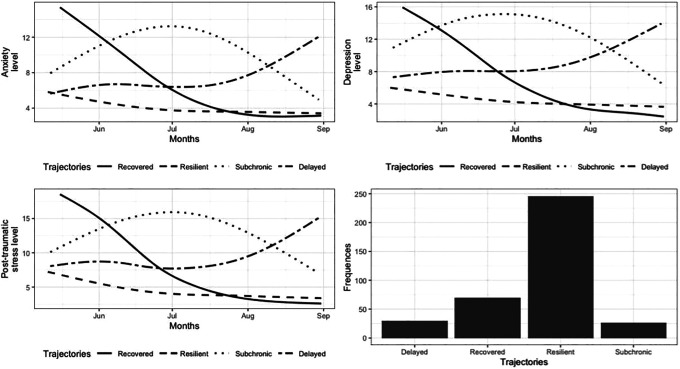
Based on the ICL-BIC values, the best fitting solution to identify the psychological functioning trajectories was a 5-class model. However, this model includes a trajectory that contains less than 5% of participants for a total of 11 participants. For this reason, a 4-class model was kept instead. Table 1 presents the parameter estimates and the model fit for the final model. Figure 3 shows each trajectory according to the 3 indicators as well as the proportion of participants included in each class.
Table 1.
Parameters Estimates and Model Fit for the 4 Latent Classes Model.
| Parameters | Four Latent Classes Model (n = 373) |
|---|---|
| Class 1: Recovered | |
| Proportion of sample | 18.77% |
| Intercept (SE) | 0.62 (0.28) |
| Class 2: Resilient | |
| Proportion of sample | 65.95% |
| Intercept (SE) | 1.57(0.26) |
| Class 3: Subchronic | |
| Proportion of sample | 7.24% |
| Intercept (SE) | −0.36(0.32) |
| Class 4: Delayed | |
| Proportion of sample | 8.04% |
| Intercept (SE) |
(reference) |
| Model fit and entropy | |
| N free parameters | 27 |
| Akaike information criterion | 41,261 |
| Bayesian information criterion | 41,367 |
| Entropy | 0.71 |
Figure 3.
Mean predicted scores of post-traumatic stress, anxiety, and depression symptoms by trajectories and proportion of participants.
The first latent class (recovered) comprised 70 participants (18.77%). This trajectory shows levels of PTS, anxiety, and depression symptoms highly above clinical threshold at the beginning of the study. Levels significantly decreased along summer to reach low sub-clinical levels in September (week 17). The second latent class (resilient) contained more than half of the total sample (246 [65.95%]). This trajectory shows a minimal decrease during summer but stays under clinical cut-offs on all 3 measures for the entire duration of the study. The third latent class (subchronic) included 27 HCW (7.24%). This trajectory presents a peculiar form with increased levels in midsummer (week 8), followed by a gradual decrease until week 17. Indeed, this group showed moderate symptoms of PTS, anxiety, and depression at the beginning (week 1). Their symptoms worsened in July (week 9 to 12) to reach severe levels. Then, symptoms on all measures gradually decreased to reach mild level in week 17. Finally, the fourth latent class (delayed) comprised 30 participants (8.04%). Unlike the other 3 trajectories, the 4th class showed an increase during the period of data collection, reaching its highest levels in week 17. This group showed sub-clinical (mild to moderate) level of PTS, anxiety, and depression to reach a severe level of symptoms at week 17 which correspond to the onset period of the second wave of COVID-19 in Canada.
Discussion
The objectives of the study were to (1) explore the evolution of psychological distress of Canadian HCW during and after the first wave of COVID-19 and (2) identify trajectories of psychological distress of these HCW using latent class analysis. This research included 373 HCW on a 4-month data collection period. The first wave of COVID-19 has been established to be between February 23 and July 11, 2020. The data collection started almost halfway through the first wave (May, 8) and ended at the gates of the second wave (September 4) in Quebec, Canada. 18 The longitudinal perspective of the study contextualized previous data. Instead of a snapshot image of psychological state, our data allowed us to better understand the evolution of psychological distress. As such, our data show a peak of psychological distress that lasted 2 to 4 weeks in June 2020 and resolved for most participants in the following weeks. June is also the month when COVID-19 deaths greatly decreased in the province of Quebec to reach rates of 6 to 10 daily deaths (compared to 150 daily deaths at the top of the curve [April 2020]). This longitudinal study provides a different perspective on the results of cross-sectional studies published to date. Indeed, reporting transversal data may sometimes sound alarming, but without considering the longitudinal evolution, these data do not demonstrate whether psychological distress is chronic or only transient.
Moreover, longitudinal analysis enabled us to identify 4 different trajectories of psychological distress among our participants: recovered, resilient, subchronic, and delayed. We found that 65.95% of the 373 HCW were in the resilient trajectory, which is characterized by the consistency of symptoms’ scores below clinical cut-offs for the entire data collection period. This again gives a clearer picture of the evolution of psychological distress among HCW as most of our participants did not present clinical symptoms of distress. This result is aligned with previous studies stating that resilience is the most prevalent response to adversity among HCW (65.7%). 19 Still, almost a third of our sample presented clinical levels of symptoms at one moment or the other between May and September 2020.
About a third (34.05%) of our HCW sample were distributed in 3 different trajectories: recovered (18.77%), subchronic (8.04%), and delayed (7.24%). For 2 of these 3 trajectories (recovered and subchronic), the presence of psychological distress was transitory, and their evolution suggests an adaptive response to the COVID-19 situation, especially for the recovered one. For the delayed class (8.04%), since they presented clinical scores at the end of the assessment period, we were not able to determine the nature of their evolution. Thereby, this longitudinal perspective showed a more optimistic picture than the ones depicted by the cross-sectional data reported so far in showing that for the majority of HCW, the distress experienced was transitory.
These 4 trajectories are consistent with what previous studies found in people who have experienced traumatic events (life-threatening medical events, bereavement, earthquake, and accident). 19 Based on 54 studies, a review showed that the most observed trajectories following a trauma were resilience (65.7%), recovery (20.8%), chronic (10.6%), and delayed (8.09%), with resilience being the modal response to adversity. 19 The class that was identified in these previous studies and that was not observed in our data is the chronic trajectory. Unlike prior trauma studies that observed individuals with the chronic level of psychological distress following a trauma, our data showed a category of HCW (subchronic) that had sub-clinical levels in early summer (week 1 to 3), became clinical in mid-summer (week 4 to 12), and returned to sub-clinical level in September (week 13 to 17). Some hypotheses allow us to explain this difference. First, unlike other types of traumatic events, the COVID-19 pandemic did not happen at a single point in time but rather manifested itself continuously in the reality of workers since March 2020. Another hypothesis is that the presence of psychological distress in mid-summer (week 14) by the delayed group may potentially be explained by personal rather than contextual variables. Considering that daily cases of COVID-19 and deaths were low at this time point, the psychological distress of these HCW could be explained by stress accumulation, tiredness, absence of vacation, family stressors, fear of second wave, and so on.
From a clinical standpoint, our results allowed us to identify classes that were more at risk. The delayed group and the subchronic face the highest risk, the first class (delayed) considering that they start the second wave in September 2020 with significant symptoms of psychological distress. We considered the subchronic class to be also potentially at risk for exacerbation of psychological distress, following a similar curved as they did in the first wave. This needs to be taken with great concern considering that we do not know for how long we are going to deal with COVID-19. Thereby, our study highlights the urgent need of providing psychological support to HCW to prevent at-risk workers from developing high levels of psychological distress. Considering our results, implementing mental health prevention procedures within health-care institutions is a priority. For those at-risk HCW, this could make the difference between remaining sub-clinical or presenting persistent symptoms of psychological distress. 29,30
Future research should evaluate potential predictors of class membership (gender, individual vulnerabilities, social and psychological support, etc.) to identify more at-risk HCW. This effort is essential to be able to offer targeted preventive intervention to HCW at risk and therefore to prevent the emergence of psychopathology.
Strengths and Limitations
This research has limitations that should be noted. The first important limitation is that participants did not respond to all the measurement points. Considering the pandemic context, we understand that the reality of workers makes constant engagement difficult, but this still represents a significant limitation of our data. It is also important to note that some of the samples’ characteristics may limit the generalization of the results, as the convenient and voluntary nature, and the high percentage of participants who worked in hospital settings (71%). The second limit is the self-reported nature of the data as social desirability and self-representation distortion. 31 However, self-report through a mobile app made this study possible in the pandemic context. The use of screening measures (GAD-7, PHQ-9, and PCL-5) may have overestimated the prevalence of what has been labelled as clinical cases.
Another limitation is the absence of a baseline measurement of psychological distress. This would have allowed us to assess if prior distress was present and could influence the data reported in the study. Finally, it is also relevant to note that Quebec was the most affected Canadian province during the first wave, and so, its reality is not a Pan-Canadian representation. Despite these limitations, to our knowledge, our study is the first to provide a longitudinal contextualization of psychological distress among HCW during and after the first wave of COVID-19.
Conclusion
The longitudinal nature of our study allowed us to contextualize prior transversal data on psychological distress among HCW during the COVID-19 crisis. Our data showed that approximately two-third (65.95%) of the 373 HCW were resilient and have not manifested significant distress during and after the first pandemic wave. The remaining third (34.05%) expressed clinical psychological distress at one moment or another between May and September 2020 but not throughout the entire period of the study. Although our data illustrated a more optimistic picture in showing that the majority of HCW follow a resilience trajectory or manifest transitory distress, it is still important to focus our attention on those who present psychological distress. Implementing preventive mental health interventions in our health-care institutions that may prevent chronic distress is imperative. It is also essential to continue assessing the long-term psychological distress of HCW, as new evolution may emerge, especially considering that we do not know how long the current pandemic will last. Further studies need to be done to identify predictors that may help to characterize these trajectories.
Acknowledgement
We thank all health-care workers who participated in this study and Rachel Primiani and Isabelle Laguë for their support with linguistic revision.
Authors’ Note: For reasons pertaining to confidentiality, the authors are not allowed to submit primary data.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research project was supported by a grant (#2020-2023-COVID19-PSOv2a-51476) from the Fonds de Recherche du Québec—Ministère de l’Économie et Innovation as well as a salary award (#268274) from the Fonds de Recherche du Québec—Institut de Recherche Robert Sauvé en Santé et Sécurité au Travail to the last author.
ORCID iDs: Marie-Michèle Dufour, PhD https://orcid.org/0000-0003-4293-9246
Steve Geoffrion, PhD https://orcid.org/0000-0001-6514-2980
References
- 1. Government of Canada . Coronavirus (COVID-19): outbreak update. Published 2021 [accessed 2021 Apr 28]. https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19.html.
- 2. Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning province, China: a cross-sectional study. Int J Environ Res Public Health. 2020;17(7):2381. doi:10.3390/ijerph17072381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi:10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ornell F, Schuch JB, Sordi AO, Kessler FHP. Pandemic fear and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020;42(3):232–235. doi:10.1590/1516-4446-2020-0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Daly M, Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J Psychiatr Res. 2021;136:603–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yarrington JS, Lasser J, Garcia D, et al. Impact of the COVID-19 pandemic on mental health among 157,213 Americans. J Affect Disord. 2021;286:64–70. doi:10.1016/j.jad.2021.02.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. El-Hage W, Hingray C, Lemogne C, et al. Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19): quels risques pour leur santé mentale?. L’Encéphale. 2020;46(3):S73–S80. doi:10.1016/j.encep.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Skari H, Skreden M, Malt UF, et al. Comparative levels of psychological distress, stress symptoms, depression and anxiety after childbirth—a prospective population-based study of mothers and fathers. BJOG. 2002;109(10):1154–1163. doi:10.1111/j.1471-0528.2002.00468.x [DOI] [PubMed] [Google Scholar]
- 9. American Psychology Association. APA dictionary of psychology. 2020. [accessed 2020 Nov 18]. https://dictionary.apa.org/psychological-distress.
- 10. Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med. 2020;13(1):40. doi:10.1186/s12245-020-00299-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic– a review. Asian Jr Psychiatr. 2020;51:102–119. doi:10.1016/j.ajp.2020.102119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi V, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi:10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alshehri M. The psychological effect of COVID-19 on healthcare workers: a systematic review. IJMDC. 2020;4(9):1495–1501. doi:10.24911/IJMDC.51-1594589748. [Google Scholar]
- 14. Que J, Shi L, Deng J, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr. 2020;33(3):e100259. doi:10.1136/gpsych-2020-100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Giusti EM, Pedroli E, D’Aniello GE, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. 2020;11:1684. doi:10.3389/fpsyg.2020.01684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59(1):20–28. doi:10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- 17. Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annu Rev Clin Psychol. 2011;7(1):511–535. doi:10.1146/annurev-clinpsy-032210-104526 [DOI] [PubMed] [Google Scholar]
- 18. Bonanno GA, Diminich ED. Annual research review: positive adjustment to adversity—trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatry. 2013;54(4):378–401. doi:10.1111/jcpp.12021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Galatzer-Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev. 2018;63:41–55. doi:10.1016/j.cpr.2018.05.008 [DOI] [PubMed] [Google Scholar]
- 20. Institut National de Santé Publique du Québec (INSPQ). Rapport épidémiologique descriptif de la COVID-19 au Québec du 23 février au 11 juillet 2020. Published 2021 [accessed 2021 Jan 15]. https://www.inspq.qc.ca/publications/3080-rapport-epidemiologique-covid19.
- 21. Katapally TR, Bhawra J, Leatherdale ST, et al. The SMART Study, a mobile health and citizen science methodological platform for active living surveillance, integrated knowledge translation, and policy interventions: longitudinal study. JMIR Public Health Surveill. 2018;4(1):e31. doi:10.2196/publichealth.8953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi:10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 23. Weathers FW, Litz BT, Keane TM, et al. The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD. Published 2021 [accessed Jan 25. www.ptsd.va.gov
- 24. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 25. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing: R package version 1.9.2. Published 2017 [accessed 2020 Nov 22]. https://cran.r-project.org/web/packages/lcmm/index.html2020.
- 27. Proust-Lima C, Philipps V, Diakite A, et al. Extended mixed models using latent classes and latent processes. J Stat Soft. 2017;78(2):1–56. doi:10.18637/jss.v078.i02. [Google Scholar]
- 28. McLachlan GJ, Peel D. Finite mixture models. New York, USA: Wiley; 2000. [Google Scholar]
- 29. Chirico F, Nucera G, Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych Int. 2020:1–2. doi:10.1192/bji.2020.39 34287401 [Google Scholar]
- 30. Irfan M, Naeem F, Afridi MI, Javed A. Prevention of occupational stress in health-care workers during COVID-19 pandemic. Indian J Psychiatry. 2020; 62(Suppl 3):S495–S497. doi:10.4103/psychiatry.IndianJPsychiatry_844_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Healthc Res 2011;2(4):320–322. doi:10.1504/IJBHR.2011.043414 [DOI] [PMC free article] [PubMed] [Google Scholar]