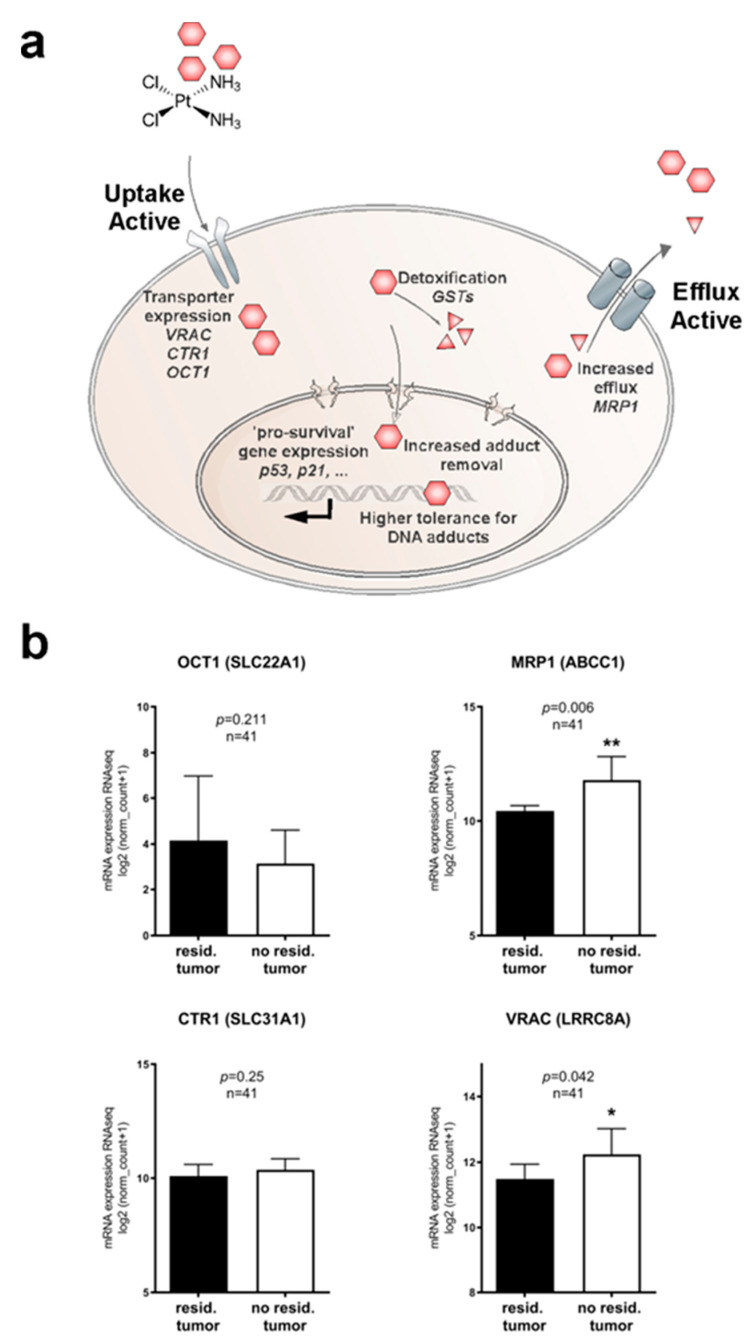
Figure 1.
Molecular pathways and potential clinically relevant players contributing to cisplatin resistance in HNSCC. (a) Cartoon depicting mechanisms potentially involved in cisplatin resistance. Reduced intracellular drug concentrations can be a consequence of reduced uptake, accelerated efflux, or intracellular detoxification. Additionally, improved DNA repair and various (indirect) pro-survival pathways may improve cancer cells’ ability to cope with cisplatin toxicity. (b) Bioinformatic identification of potential clinically relevant drug transporters in the transcriptomics dataset of HNSCC patients from The Cancer Genome Atlas (TCGA) (n = 565). Correlation of drug transporter transcription levels with residual tumors after first-line chemoradiotherapy and full clinical documentation (n = 41) were assessed. Low expression of drug import channels, i.e., reduced uptake of cisplatin, is expected to favor cancer cell survival and thus, tumor recurrences. We found an unexpected trend of decreased expression of OCT1, and expression levels of the drug uptake transporter CTR1 remain similar. However, enhanced expression of the drug export transporter MRP1 and increased expression of the drug uptake transporter VRAC significantly correlated with lower tumor recurrences. *, p < 0.05; **, p < 0.01.