To the Editor: Since 1027, when the Tian Sheng Bronze Statue showing acupoints and meridians was first introduced for medical practitioners, it has evolved to the currently used acupoints and meridians atlas in traditional Chinese medicine (TCM).[1] To date, the acupoints represent defined areas on the body surface relative to certain landmarks. The acupoints in the extremity endings would connect anatomically with diverse associated visceral organs or tissues, forming a Meridian and Collateral network. Illustrated on the atlas, each main meridian is usually a virtual line connecting a group of adjacent acupoints that correlate with certain visceral organ. In modern medical science, the anatomical structures of main meridians remain largely unclarified.
In TCM, an acupoint is considered as a gateway for substances or bio-signals to enter or escape the meridians.[1] For several decades, sequential efforts were made to track the transport processes of an imaging tracer from the acupoints on the meridians. So far no one can find a conduit-like structure (other than the blood or lymph vessels) connecting the acupoints on the body surface and different visceral organs. However, the unique research strategy has lightened a physiological question that was initiated by Ernest Starling in 1896, that is, how the fluid flows in interstitial connective tissues or even circulates throughout the body like blood and lymph.[2]
Explorations of fluid flow from an acupoint: In the early 1960s, by hypodermic injection of a colored dye into the acupoints of animals, it was claimed that a conduit-like structure named “Bonghan ducts” could be observed for fluid flow from acupoints.[3] Since the 1990s, these structures have been re-investigated by the injection of Trypan blue or Alcian blue and were renamed as “primo-vessels” or “primo vascular system.”[4] Basically, the “primo-vessels” were described to be a new kind of micro-conduit lined with endothelial cells to support fluid flow and contain multiple channels surrounded by loose collagenous matrices.[5] However, the stated anatomical and histological structures of the “primo-vessels” remained ambiguous and the relationship with human acupoints was not clear.
In the 1950s to 1990s, by the hypodermic injection of an isotopic tracer into the acupoints in the hands or feet of humans, a long-distance migration channel from an acupoint could be visualized by radionuclide imaging techniques.[6,7] Meng et al[8,9] investigated the migration channels of technetium-99m from the acupoints of 12 main meridian channels and found that the isotopic tracer migrated over a long distance in either the upper or lower limbs. The radiotracer migration channels from the acupoint of Neiguan were distinct from those originating from a non-acupuncture and non-meridian point.[10] However, there is a lack of more comprehensive data to confirm whether all the other acupoints on the meridian lines have these isotopic channels development. By comparison, the trajectories of the radioactive tracers from acupoints were also different from those of intravenously injected isotopes and lymphotropic isotopes.[11,12] These studies suggested that the isotopic migration channel from an acupoint should be a unique interstitial fluid (ISF) flow pathway rather than a conduit-like vessel. Although somewhat similar to the 12 main meridian lines on the atlas, it is difficult to draw the relationship between the acupoint-originated isotope migration channels and the meridians in humans. Other published studies showed that the radiotracer from the acupoint entered the venous system via the lympho-venous anastomoses and therefore denied that the radiotracer migration proves the existence of the meridian lines.[13] Besides, the histological structures of the isotopic pathways could not be clearly identified due to the poor spatial resolution (approx. 1 cm) of scintigraphic images.
Since 2006, the contrast-enhanced magnetic resonance imaging (MRI) technique was used to investigate the fluid flow originating from an acupoint in healthy volunteers [Figure 1A and Figure 1B].[14,15] By the hypodermic injection of a paramagnetic tracer (gadolinium diethylenetriamine pentaacetic acid [Gd-DTPA]) into an acupoint of the hands or feet, the high spatial resolution (approx. 1 mm) MRI visualized two types of the long-distance fluid flow pathways originating from the acupoints: the smooth and non-smooth pathways. The smooth pathways showed a continuous trajectory, whereas the non-smooth pathways showed a discontinuous trajectory. Neither the smooth nor the non-smooth pathways from the same acupoints identified by MRI colocalized with the lymphatic vessels as visualized by iodized oil. If the injection point was not an acupoint but in the vicinity of a vein, only the smooth pathways were observed. If the injection point was an acupoint, then both the smooth and the non-smooth pathways can be observed at the same time. By comparison, neither the smooth pathways nor non-smooth pathways totally match the 12 main meridian lines on the atlas.
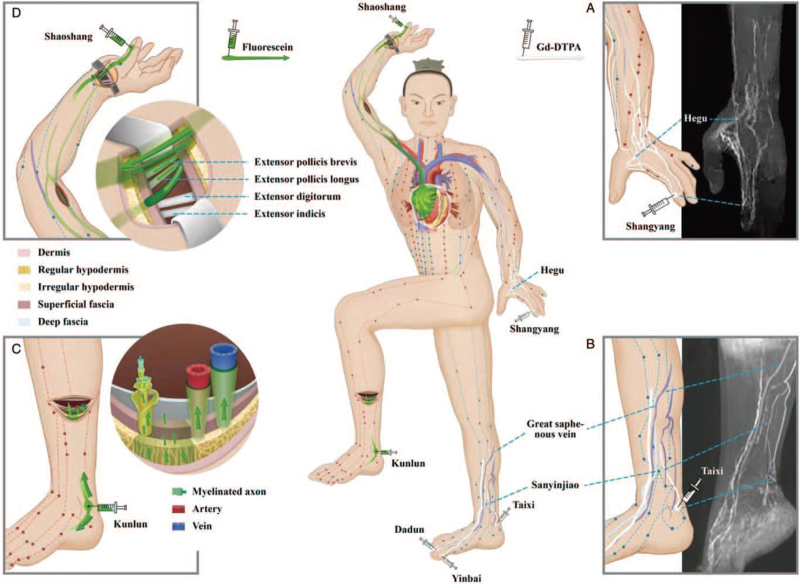
Figure 1.
A diagram of the acupoint-originated ISF flow pathways in the human body. Red, green dots and lines on the body surface represent the acupoints and main meridians in the atlas currently used in TCM. (A, B) shows the contrast-enhanced ISF flow pathways (white lines) originating from the acupoints in hand or foot by MRI. (C) shows the fluorescent ISF flow pathways (green arrows) from an acupoint in an ex vivo human leg sample, who took the acupoint injection before the lower leg amputation due to his severe foot gangrene. (D) shows the fluorescent ISF flow pathways from an acupoint in a cadaver that was performed by repeated chest compressions for 2.5 hours after the injection. (A) The ISF flow pathways (white lines) originating from Shangyang (the Jing-Well acupoint of Large Intestine Meridian) of a volunteer were found converging into one intersection point or pass by the downstream acupoint of Hegu in dorsal hand. (B) Originated from the three upstream acupoints of Yinbai in Spleen Meridian, Dadun in Liver Meridian, and Taixi in Kidney Meridian, it was found that the three ISF pathways (white lines) pass by the downstream acupoint of Sanyinjiao in different depths instead of converging into one intersection point. (C) At least four types of the fluorescent ISF pathways (green arrows) originating from Kunlun (the Jing-River point of the Urinary Bladder Meridian) were found in lower leg, including the cutaneous, perivenous, periarterial, and neural pathways. (D) The fluorescent ISF pathways (green arrows) originating from Shaoshang (the Jing-Well point of the Lung Meridian) were found to flow along the upper arm toward the right atrium and pericardium via the cutaneous pathway and venous PACT pathway along the veins in arm, superior vena cava, into the right atrial wall. The cutaneous pathways from the thumb can be seen on the skin of hand and lower forearm but not the skin above the level of the cubital fossa. When the skin of the wrist was opened layer by layer, the cutaneous pathways were found to contain layers of connective tissues, including the dermic, hypodermic, superficial, and deep fascial tissues on the tendons associated with thumb but not the tendons from the index finger. ISF: Interstitial fluid; MRI: Magnetic resonance imaging; PACT: Perivascular and adventitial connective tissue; TCM: Traditional Chinese medicine.
Unlike the fuzzy isotopic findings, the distinct MRI results raised a critical question: What is the relationship between the meridians in TCM and the fluid flow pathways enhanced by the tracer originating from an acupoint? Before answering, we should first clarify the anatomical and histological structures of such acupoint-originating fluid flow pathways in humans.
To identify the ISF pathways from an acupoint in physiological conditions, fluorescent imaging was adopted in an ex vivo human leg sample under a very special circumstance [Figure 1C].[16] In a patient with severe foot gangrene and preparing for lower leg amputation, a fluorescent tracer was injected hypodermically into the Kunlun acupoint at the ankle before the amputation. The lower leg was dissected carefully after amputation, revealing that several long-distance ISF flow pathways were revealed by the fluorescent tracer, which originated from the Kunlun acupoint at the ankle and extended to the upper end of the amputated leg. Based on the histological analysis under fluorescent microscopy, the following four types of pathways were identified: (1) a cutaneous pathway in the dermis and hypodermis tissues; (2) a perivascular and adventitial connective tissues (PACT) pathway along the venous vessels; (3) a PACT pathway along the arterial vessels; and (4) a neural pathway that is composed of the endoneurium, perineurium, and epineurium of a peripheral nerve. Compared with the MRI results, the cutaneous pathways were probably the non-smooth pathways, and the PACT pathways were probably the smooth pathways.[18] All the four types of pathways were composed of fibrous connective tissues rather than endothelial cells. These data provide confirmative evidence that the acupoint-originated pathways are distinct from the blood or lymph flow and should be a long-distance ISF flow pathway.
To detect the systemic distributions of the ISF flow pathways in visceral organs or tissues, a mechanical automatic chest compressor was used on human cadavers to simulate the heart beating and chest movements in live humans [Figure 1D].[17] Repeated chest compressions were performed for 2.5 hours after a hypodermic injection of the fluorescent tracer into the Shaoshang acupoint in the first knuckle of the thumb. Fluorescent imaging revealed a cutaneous and perivenous pathway from the Shaoshang acupoint of the thumb to the right atrium. The cutaneous pathways from the thumb were found in the hand and lower forearm, but not in the skin above the level of the cubital fossa. The cutaneous pathway contained the dermic and hypodermic tissues, and the superficial and deep fascial tissues from the thumb but not from the index finger. The PACT pathways from the thumb were observed along the veins of the arm, axillary sheath, superior vena cava, and into the pericardium and epicardium tissues over the right atrium. At the millimeter scale, micro-CT imaging showed that the interlobular septum of the adipose tissues in the cutaneous pathways was longitudinally assembled toward the direction of ISF flow. In contrast, the interlobular septum of the skin tissues outside the pathways was irregular. At the microscopic level, the intrinsic framework of the ISF pathways comprised abundant micron-sized fibers that are assembled longitudinally toward the direction of ISF flow. Under a confocal laser microscope, these longitudinally assembled fibers and their surrounding gel-like interstitial matrix were found fluorescently stained, which are the results of the long-distance ISF flow.
Connective tissues are one of the four basic types of animal tissue and are continuously distributed throughout the body. The identifications of the ISF flow pathways from acupoints in humans strongly indicates that the ISF may flow systematically in the interstitial connective tissues, comprising diverse types of the ISF pathways.
Explorations of fluid flow in interstitial connective tissues: Since Ernest Starling described the net flow of fluid between the connective tissue spaces and the capillary lumen in 1896, the transport pattern and mechanical mechanism of ISF flow through extravascular spaces or interstitial connective tissues have been explored by generations. Using porous matrix theory and the measurements of hydraulic conductivity of various tissues based on a method designed by Aukland and Fadnes[18] and Adair and Guyton,[19] it was found that ISF diffuses mainly for short distances through the tissue gel between capillaries and adjacent cells. Even though the ISF, can occasionally flow freely as small rivulets and vesicles for a short distance in the interstitium. As stated in the physiology textbook, when a dye is injected into the circulating blood, it often can be seen to flow along the surfaces of collagen fibers or surfaces of cells.[20] To study such ISF flow phenomena, the methods of observing the ISF flow with an imaging tracer are more direct by comparison with measuring the intricate interstitial pressure gradients.
In the 1950s to 1970s, a linear fluorescent pathway was observed along the elastic fibers of the interstitial connective tissues after the passage of fluorescent dye through the microvascular wall in the mesentery of the rabbits and cats.[21] The fluorescein transport occurs much faster than diffusion and the elastic fibers might have a passive transport or guide rail function for fluid flow between arterial and venous regions of the capillaries and lymphatic vessels. The fluorescein transport pathway in the interstitial connective tissues was marked as a “low-resistance” pathway or described as an extravascular fluid pathway by Kihara in 1956.[2]
The regional ISF flow after deriving from the capillaries was further studied by the incomplete dark field transillumination and electron microscopy. The movements of the marked ISF in interstitial connective tissues were named as prelymphatic or interstitial tissue channels by Catchpole,[22] Casley-Smith,[22] and Hauck[2] in the 1960s to 1970s, respectively. The tissue channels were believed to connect continuously with the initial lymphatic vessels, forming a random network of converging drainage pathways in interstitial connective tissues.[22] Illustrated by India ink suspension, fluorescein-isothiocyanate, and ferrocyanide precipitates, the positions of the tracers are found to be near the vessel wall or in the skeletal muscle tissues or intestinal wall and represent a water-rich region in interstitial connective tissues.[2,22] However, the spatial structures of such an interstitial tissue channel and its surroundings in the gel-like interstitial matrix for fluid flow have not been adequately stained and identified until now. Due to the indistinct definition, the tissue channel is insufficient to disclose a continuous spatial structure throughout the interstitial connective tissues for a long-distance ISF flow.
The above imaging studies suggested that: (1) ISF can flow through interstitial connective tissues but the spatial structures where the ISF flows need to be identified. (2) Revealing the spatial structures of the fibrous matrix for fluid flow, as well as their boundary structures and compositions, might be a key to reveal the mechanical mechanism of the long-distant ISF flow in interstitial connective tissues. (3) ISF flow may be not only a diffusive process but also guided by fibers, indicating a unique dynamic mechanism to drive the ISF besides the pressure and concentration gradients. Interestingly, the findings on the diverse types of the ISF flow pathways from an acupoint, especially the PACT pathways along vascular vessels, might reveal the spatial structures and driving mechanisms of the long-distance ISF flow in the interstitial connective tissues.
ISF can circulate via the PACT pathways along the vascular vessels around the body: Using the in vivo imaging technique and histological identification, the ISF flow along vascular adventitia has been identified in several veins and arteries of systemic and pulmonary circulation.[23,24] In rabbits, the peripheral ISF in the ankle dermis was found to flow constantly along the veins in the lower extremity veins, inferior vena cava in the abdomen and thorax, and into the epicardium forming pericardial fluid.[23] The velocity of the constant adventitial ISF flow was estimated as 3.6 to 15.6 mm/s.[24] Meanwhile, the peripheral ISF was found to enter the capillaries or lymphatic vessels and merged into blood circulation.[23,24] A constant ISF flow along the veins and arteries of lower limbs was also observed in mice as well.[25] In the rabbit pulmonary circulation, the ISF flow was found to flow along the pulmonary vein from the lung toward the heart.[24]
Unlike blood in a sealed cardiovascular conduit, the spaces in a PACT pathway for the ISF flow were unique. In live rabbits by real-time fluorescence stereomicroscopy, the ISF in a venous PACT pathway was found to flow in at least two layers[24]: (1) ISF flow between the covering fascia and adventitia and (2) ISF flow through adventitia. Under a confocal laser microscope, the venous adventitia was found to comprise abundant fluorescently stained fibers and their surrounding gel-like matrix, which were the results of the fluorescent ISF flowing in the PACT pathways.[24] In the fibrous matrix, neither the fibers nor the fascia nor the gel can flow. We named the spaces in the PACT pathways for the constant ISF flow as an “interfacial zone or interspace” between a solid phase (a fiber or fascia) and a liquid phase (the gel/liquid substance).[24,26] The patterns of ISF flow in a PACT pathway were named as “interfacial fluid flow.”[24] When fluid entered such topologically connected interfacial zones or poly-interspaces along the solid fibers or fascia in a PACT pathway, the ISF would flow constantly along the vessels under an actively dynamic driving power, such as the heart beatings and respiratory movements.[24] There were two patterns of a constant ISF flow found in the venous PACT pathways: (1) a longitudinal flow along the vascular vessel toward a driving center and (2) diffusion from the vessel into the surrounding tissues, like an irrigation system.[24]
Based on the pattern of pulling the ISF from a PACT pathway and the characteristics of the gel-like matrix to absorb and release water, a hypothetical “gel pump” has been proposed.[16,24,26–28] Generally, the gel-like fibrous connective tissues covering the cardiovascular system can work as a driver, that was named as “gel pump,” to regulate the ISF. When the heart contracts and relaxes repeatedly, the gel-like matrix covering on the heart will squeeze out fluid and release it into the surrounding cavity. Particularly, the matrix of the drivers might be a one-way “pump” that normally allows fluid to flow from the ISF pathways into the gel pump, and meanwhile to prevent the fluid within the gel pump from flowing back into the pathways. In the human cadaver experiments, the “gel pump” on the heart that was repeatedly compressed by an automatic cardiac compressor, had “pulled” the peripheral ISF in the thumb via the PACT pathways into the epicardium.[16] In live rabbits, the “gel pump” on the heart had “pulled” the peripheral ISF via the PACT pathways into the superficial tissues on the heart and entered the pericardial cavity, causing pericardial effusion.[23,24] The detailed driving mechanism needs further investigation. In short, the one-way gel pump mechanism suggests that the ISF flow in the network of interstitial connective tissue is a phenomenon of capillary flow (or interfacial fluid flow) driven by an actively force in biological and living system.[24]
An acupoint-originated interstitial fluid circulatory system throughout the body: Distinguished from the rodents, we have found diverse types of the long-distance ISF flow pathways originating from an acupoint in the human body: the cutaneous-, venous PACT-, arterial PACT-, fascial-, and neural-pathways. So far it is not clear whether the cutaneous, fascial and neural ISF may circulate systematically around the whole body like the adventitial ISF flow pathways. To comprehend the acupoint-originated ISF circulatory system, a working hypothesis is proposed: (1) There are one or more ISF flow pathways connecting with an acupoint on the body surface, including at least one cutaneous pathway. (2) An ISF circulatory network is constituted between different acupoints on the body surface and their associated visceral organs or tissues. (3) The acupoint-originated ISF circulation is regulated mainly by the cardiovascular system via the heart beatings and respiratory movements. (4) The acupoint-originated ISF circulatory network is part of an ISF circulatory system, communicating and coordinating functionally with the other systems of the human body, such as the nervous system and cardiovascular system. (5) The internal environment around the cells in a visceral organ or tissue can be modulated from certain acupoints on the body surface via the ISF circulatory system.
Using a mechanical automatic chest compressor and ventilator to simulate the heart beatings and respiratory movements, a network of the acupoint-originated ISF flow pathways from each acupoint on all fingers and toes can be found in the cadavers.[16] In contrast, enhanced or other specific MRI techniques, such a network can be visualized in live human subjects.[13,14] According to the 12 main meridians in TCM, the acupoint-originated ISF flow networks from all acupoints on each finger and toe might be divided into 12 groups. If a “node” is defined to correspond to an acupoint and the “lines” to the various types of the ISF flow pathways, 12 groups of the node-lines networks can be aligned and constructed as an acupoint-originated Human Interstitial Fluid Connectome Atlas (HIFCA).[26] The reflected projections of the 12 groups of the diverse node-lines on the body surface might be able to be compared with the 12 meridian lines on the TCM atlas. The connections with the visceral organs or tissues of the 12 groups of the node-lines networks might also be compared with the relations between the acupoints on the body surface and the corresponding internal organs described by the 12 main meridians in TCM.
Together with previous studies, an acupoint may become a historical intersection of ancient medical knowledge and modern medical science, where we could cherish ancestral treasures and inaugurate a new frontier for innovative medical applications.
Funding
This work was supported by grants from the Beijing Hospital Clinical Research 121 Project (No.121-2016002) and the National Natural Science Foundation of China (Nos. 82050004, 82050005, 12050001), and the CAMS Innovation Fund for Medical Sciences (CIFMS No. 2017-I2M-3-008).
Conflicts of interest
None.
Footnotes
How to cite this article: Li HY, Wang F, Chen M, Zheng ZJ, Yin YJ, Hu J, Li H, Sammer A, Feigl G, Maurer N, Ma C, Ji FS. An acupoint-originated human interstitial fluid circulatory network. Chin Med J 2021;134:2365–2369. doi: 10.1097/CM9.0000000000001796
References
- 1.Deng LY, Gan YJ, He SH. Zheng QW, Xue XL, Gu YH. An introduction to acupuncture points. Chinese Acupuncture and Moxibustion. Beijing: Foreign Languages Press; 1999. 115–134. [Google Scholar]
- 2.Hauck G. The connective tissue space in view of the lymphology. Experientia 1982; 38:1121–1122. doi: 10.1007/BF01955400. [DOI] [PubMed] [Google Scholar]
- 3.Kim BH. On the Kyungrak system. J Acad Med Sci (DPR Korea) 1963; 90:1–41. [Google Scholar]
- 4.Lee C, Seol SK, Lee BC, Hong YK, Je JH, Soh KS. Alcian blue staining method to visualize Bssonghan threads inside large caliber lymphatic vessels and x-ray microtomography to reveal their microchannels. Lymphat Res Biol 2006; 4:181–190. doi: 10.1089/lrb.2006.4402. [DOI] [PubMed] [Google Scholar]
- 5.Yoo JS, Ayati MH, Kim HB, Zhang WB, Soh KS. Characterization of the primo-vascular system in the abdominal cavity of lung cancer mouse model and its differences from the lymphatic system. PLoS One 2010; 5:e9940.doi: 10.1371/journal.pone.0009940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gu HS. Pilot study on the visualization of NaI125 from acupoints on pericardium meridians. Nat Mag 1980; 3:681–682. [Google Scholar]
- 7.Tiberiu R, Gheorghe G, Popescu I. Do meridians of acupuncture exist? a radioactive tracer study of the bladder meridian. Am J Acup 1981; 9:251–256. [Google Scholar]
- 8.Meng JB, Gao HH, Wang P, Tian JH, Liu YL. A pilot study to visualize the migration channels along meridians by isotope-labeled tracer (in Chinese). Zhen Ci Yan Jiu 1987; 12:77–81. [PubMed] [Google Scholar]
- 9.Meng JB, Gao HH, Chang BQ. Research of human meridian using radionuclide scintigraphy (in Chinese). Zhen Ci Yan Jiu 1989; 14:91–94. [Google Scholar]
- 10.Wen C. Observations on the injection of an isotopic radionuclide tracer into acupoints and non-acupoints of the upper limbs (in Chinese). Zhen Ci Yan Jiu 1989; Suppl IV:1. [Google Scholar]
- 11.Gao HH, Meng JB, Wang P, Wen C, Tian JH, Xu FL, et al. Research on meridian flow route by nuclear medicine (in Chinese). J Trad Chin Med 1987; 11:59–61. [Google Scholar]
- 12.Kovacs FM, Gotzens V, García A, García F, Román FS, Mufraggi N, et al. Experimental study on radioactive pathways of hypodermically injected Technetium-99m. J Nucl Med 1992; 33:403–407. doi: 10.1142/S0192415X96000128. [PubMed] [Google Scholar]
- 13.Lazorthes Y, Esquerre JP, Simon J, Guiraud G, Guiraud R. Acupuncture meridians and radiotracers. Pain 1990; 40:109–112. doi: 10.1016/0304-3959(90)91058-Q. [DOI] [PubMed] [Google Scholar]
- 14.Li HY, Yang JF, Chen M, Xu L, Wang WC, Wang F, et al. Visualized regional hypodermic migration channels of interstitial fluid in human beings: are these ancient meridians? J Altern Complement Med 2008; 14:621–628. doi: 10.1089/acm.2007.0606. [DOI] [PubMed] [Google Scholar]
- 15.Li H, Tong J, Cao W, Li H, Dai H, Xu L, et al. Longitudinal non-vascular transport pathways originating from acupuncture points in extremities visualised in human body. Chinese Sci Bull 2014; 59:5090–5095. doi: 10.1007/s11434-014-0633-7. [Google Scholar]
- 16.Li HY, Yang CG, Lu K, Zhang L, Yang L, Wang F, et al. A long-distance fluid transport pathway within fibrous connective tissues in patients with ankle edema. Clin Hemorheol Microcirc 2016; 63:411–421. doi: 10.3233/CH-162057. [DOI] [PubMed] [Google Scholar]
- 17.Li HY, Yang C, Yin Y, Wang F, Chen M, Xu L, et al. An extravascular fluid transport system based on structural framework of fibrous connective tissues in human body. Cell Prolif 2019; 52:e12667.doi: 10.1111/cpr.12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aukland K, Fadnes HO. Protein concentration of interstitial fluid collected from rat skin by a wick method. Acta Physiol Scand 1973; 88:350–358. doi: 10.1111/j.1748-1716.1973.tb05464.x. [DOI] [PubMed] [Google Scholar]
- 19.Adair TH, Guyton AC. Measurement of subcutaneous tissue fluid pressure using a skin-cup method. J Appl Physiol 1985; 58:1528–1535. doi: 10.2170/jjphysiol.35.1101. [DOI] [PubMed] [Google Scholar]
- 20.Guyton AC. The microcirculation and the lymphatic system: capillary fluid exchange, interstitial fluid, and lymph flow. Textbook Med Phys 2011. 177–190. [Google Scholar]
- 21.Hauck G, Brocker W, Weigelt H. The prelymphatic transinterstitial pathway. J Lymphol 1978; 2:70–74. [Google Scholar]
- 22.Casley-Smith JR. Calculations relating to the passage of fluid and protein out of arterial-limb fenestrae, through basement membranes and connective tissue channels, and into venous-limb fenestrae and lymphatics. Microvasc Res 1976; 12:13–34. doi: 10.1016/0026-2862(76)90003-0. [DOI] [PubMed] [Google Scholar]
- 23.Li HY, Chen M, Yang JF, Yang CQ, Xu L, Wang F, et al. Fluid flow along venous adventitia in rabbits: is it a potential drainage system complementary to vascular circulations? PLoS One 2012; 7:e41395.doi: 10.1371/journal.pone.0041395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li HY, You LV, Chen XL, Li B, Hua Q, Ji FS, et al. Layers of interstitial fluid flow along a “slit-shaped” vascular adventitia (in Chinese). J Zhejiang Univ-Sci B 2021; 22:647–663. doi: 10.1631/jzus.B2000590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kong Y, Yu X, Huang R, Li Z, Yin Y, Li H. Preliminary study on the drainage effect of the venous and arterial adventitia and perivascular connective tissue on edema of lower Limbs in mice (in Chinese). Chin J Geriatr 2021; 40:9–14. doi: 10.3760/cma.j.issn.0254-9026.2021.08.000. [Google Scholar]
- 26.Li HY, Yin Y, Yang C, Chen M, Wang F, Ma C, et al. Active interfacial dynamic transport of fluid in a network of fibrous connective tissues throughout the whole body. Cell Prolif 2020; 53:e12760.doi: 10.1111/cpr.12760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li HY, Han D, Li H, Chen M. A biotic interfacial fluid transport phenomenon in the meshwork of fibrous connective tissues over the whole body (in Chinese). Prog Physiol Sci 2017; 48:81–87. doi: 10.3969/j.issn.0559-7765.2017.02.001. [Google Scholar]
- 28.Li HY, Ji FS, Wang F, Yang CQ, Ma C, Yin YJ, et al. Research progresses on active interfacial fluid flow and its dynamic mechanism in a network of human fibrous connective tissues. Prog Physiol Sci 2021; 52:155–161. doi: 10.3969/j.issn.0559-7765.2021.02.016. [Google Scholar]