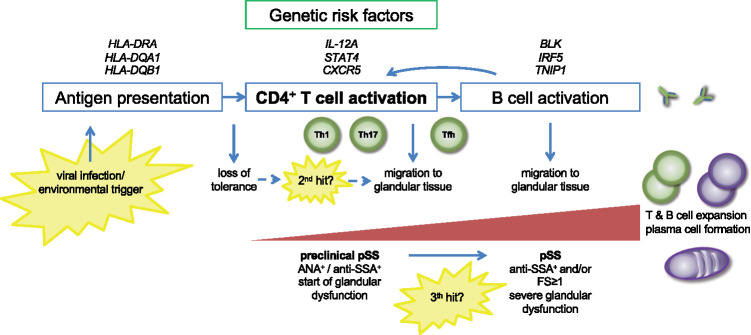
Fig. 1.
Proposed role of CD4+ T cells in primary Sjögren’s syndrome (pSS) pathogenesis
Antigen is presented to CD4+ T cells via MHC class II (HLA) molecules, resulting in CD4+ T cell activation. Risk loci in HLA-DR and HLA-DQ regions, associated with pSS, may be involved in a loss of tolerance to self-antigens. Depending on the type of antigen and additional environmental cues, differentiation of naïve cells into Th1 cells, Th17 cells and Tfh cells is induced. IL-12A and STAT4 risk variants may contribute to enhanced Th1 cell differentiation. A second, local hit may induce migration of effector CD4+ T cells to salivary and/or lacrimal gland tissues. This stage is clinically reflected in features suggestive of pSS, without the presence of focal periductal infiltrates and without evident signs of B cell hyperactivity. A third hit is probably required to establish a positive feedback loop between T cells and B cells, resulting in T cell–dependent B cell hyperactivity. In this stage, typical features associated with pSS become evident.