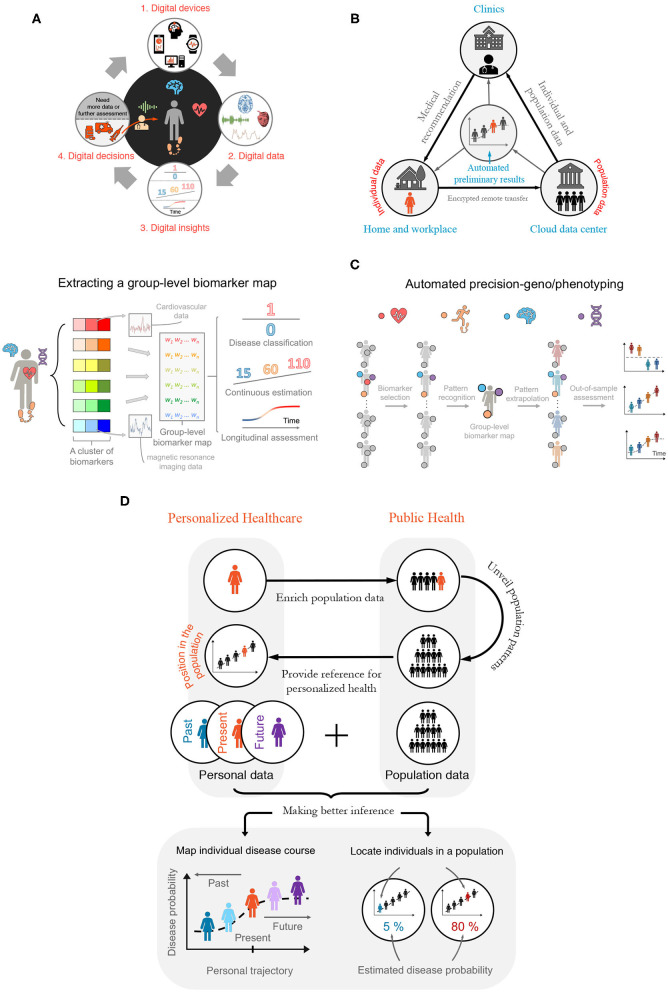
Figure 1.
Building a Digitalized Ecosystem. (A) Digitalization cycle—bridging digital health, data, and digitally enabled decision-making. From 1 to 2: Phenotypic information is recorded by, and made available on, digital devices. From 2 to 4 via 3: Advanced modeling and analyses are applied on digital data to guide health-care decisions by physicians, such as recommending potential treatments (see bottom of item 4) and suggesting conducting further diagnostic tests or analyses (from 4 to 1). (B) Semi-automated disease diagnosis and monitoring. Individual data are de-identified, encrypted, and transferred remotely via the cloud to secured data centers—where population-level disease analyses are performed. The individual data are then analyzed and compared with the population features to generate an automated preliminary diagnosis report. Should red flags be raised, the report is passed on to a medical professional. The medical professional looks at both the report and the individual-specific data to offer medical recommendations or to arrange for an on-site visit or remote consultation (e.g., telemedicine), depending on which further tests are anticipated. This process continues between an individual's periodic health checks to ensure earliest possible detection of symptoms and to compensate for long consultation intervals when regular assessment is too expensive or inconvenient. (C) Automated deep-geno/phenotyping. The digital health applications facilitate ensemble-learning, where multivariate genotypic and phenotypic (e.g., digital biomarker, imaging, and molecular diagnostics) data are combined to provide rich subject-specific and group-level information, which are used to position individuals within a relevant population or to predict outcomes for individuals, based on population norms. (D) The marriage between personalized health care and public health. There is a powerful interdependent and synergistic relationship between personalized health care and public health in the digital age. Top: When shared, personal digital health data bring rich heterogeneous information into the population data pool. In return, features identified in large-scale public health data will provide a reference for individuals, positioning them relative to comparable cohorts in the population, based on age, sex, ethnicity, etc. Bottom: Integrating individual and population data. Data collected longitudinally over months and years enable risk estimation and disease forecasts, such as estimating the likelihood of disease progression or quantifying response to different treatments.